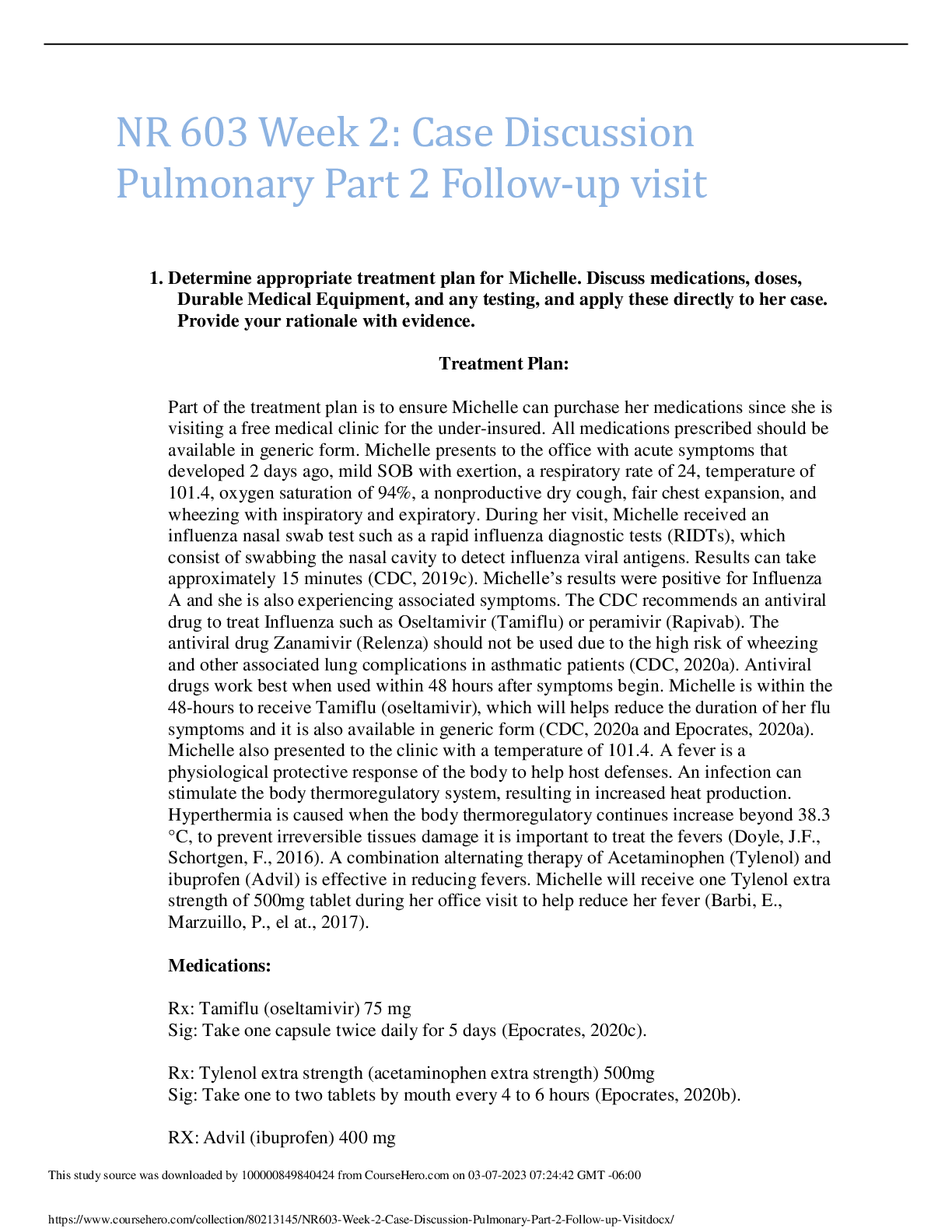
Determine appropriate treatment plan for Michelle. Discuss medications, doses, Durable
Medical Equipment, and any testing, and apply these directly to her case. Provide your
rationale with evidence.
Influenza infectio
...
Determine appropriate treatment plan for Michelle. Discuss medications, doses, Durable
Medical Equipment, and any testing, and apply these directly to her case. Provide your
rationale with evidence.
Influenza infections are a respiratory disease that can trigger asthma attacks and cause worsening
asthma symptoms (CDC, 2019). Adults that have asthma and become infected with influenza are
more likely to develop pneumonia after getting sick with influenza than those who do not have
asthma (CDC, 2019). Treatment with antiviral medications work best when started within 48
hours after symptoms start (Gaitonde, et al., 2019). Antiviral medications work by fighting
against influenza and preventing the virus from making more viruses in the body (CDC, 2019).
Oseltamivir or Peramivir are the two antiviral medications that can be used in patients with
asthma (Gaitonde, et al., 2019). A different antiviral medication, Relenza, should not be used in
patients with asthma due to the risk of causing wheezing (CDC, 2019). Michelle your symptoms
began 2 days ago (within the 48 hour window), therefore allowing you to be a candidate for
antiviral therapy. Michelle you also have an allergy to strawberries and erythromycin. These
allergies will allow you to take Oseltamivir.
Influenza can cause a dry or productive cough, fever, muscle aches, congestion, increased
shortness of breath, or wheezing (CDC, 2019). The Infectious Disease Society of America
(IDSA) recommend that providers who have a diagnosis of influenza are discouraged to use
unnecessary antibiotics (Uyeki, et al., 2018). If a patient with confirmed influenza, such as
Michelle, does not demonstrate clinical improvement with antiviral treatment or demonstrates
clinical deterioration during or after treatment, additional testing should be considered to rule out
other infectious diseases, such as pneumonia (Uyeki, et al., 2018). Symptom relief is a goal for
those diagnosed with influenza (CDC, 2019). Staying home and getting plenty of rest, drinking
lots of fluid to avoid dehydration, and treating fever are all ways to help relief symptoms
(Kennedy-Malone, et al., 2019). NSAIDs can exacerbate symptoms of asthma and should not be
used (Kennedy-Malone, et al., 2019). Acetaminophen is a good alternative to relieve fever or
pain and does not exacerbate asthma (Kennedy-Malone, et al., 2019). Michelle, I want you to
avoid NSAIDs, such as, ibuprofen and to take acetaminophen as needed over-the-counter for
fever. Your asthma symptoms have been well-controlled with a low-dose inhaled corticosteroid
inhaler, Singulair, and Albuterol as needed. If asthma symptoms are well-controlled there is no
need to modify current treatment rather the goal is to treat the risk factor that is causing
symptoms (GINA, 2020). Spirometry and peak flow testing should be avoided unless there is an
urgent need to prevent the spread of viral particles (GINA, 2020). The appropriate test has
already been completed to confirm a diagnosis of influenza-A.
Decide whether she is safe to return home, include any prescriptions, or if a referral to a
higher level of care is required. Discuss the criteria used to make your decision, how a
referral is made and defend your position.
This study source was downloaded by 100000830772748 from CourseHero.com on 05-12-2022 08:34:39 GMT -05:00
https://www.coursehero.com/file/66191791/NR-603-Week-2-Part-2-Case-Studydocx/
Michelle I am sending you home on Oseltamivir as discussed above. Oral corticosteroids are a
common treatment for acute asthma flare-ups or exacerbations by another illness to reduce
inflammation and swelling in the airways (Castillo, et al., 2017). Oral corticosteroids have been
proven to reduce emergency room visits and hospitalizations for asthma (Castillo, et al., 2017).
Oral steroids should be given for asthma exacerbations preferably in the morning for no more
than 5-7 days at either 40-50mg per dose (GINA, 2020). Michelle, these are the following
medications I am ordering for you today:
Oseltamivir 75mg Capsule
Sig: Take 1 capsule by mouth twice daily for 5 days
Disp: 10
Refills: 0
(Gaitonde, et al., 2019).
Predisone 50mg tablets
Sig: take one each morning by mouth for 5 days
Disp: 5
Refills: 0
(GINA, 2020).
Acetaminophen 500mg capsules/tablet
Sig: Take 2 caplets by mouth every six hours as needed for fever
Over-the-counter
Features such as a history of near-fatal asthma requiring intubation, poor adherence to
medication, or lack of a written action plan should raise concern for asthma-related deaths and
should be triggered for further intervention (GINA, 2020). If the patient is confused, drowsy,
silent chest, and/or has low oxygen saturations (below 90%) in a primary care setting, they
should be transferred to an acute care facility (GINA, 2020). Appropriate oxygen saturations for
adults with asthma are 94-98% on room air (GINA, 2020). Michelle does not present with
confusion, drowsiness, or low oxygen saturation, she has audible respiratory sounds, and is
compliant with her medications, therefore making it safe for her to return to home. Michelle
does not require a referral to a higher level of care.
Discuss relevant education and follow up plan.
Michelle I am providing you with a written action plan appropriate for your level of asthma
control and health literacy, so you will be able to recognize and respond to worsening asthma
(GINA, 2020 & Kennedy-Malone, et al., 2019). The written action plan includes your regular
asthma medication, when to start the oral corticosteroid, and how to access medical care if
This study source was downloaded by 100000830772748 from CourseHero.com on 05-12-2022 08:34:39 GMT -05:00
https://www.coursehero.com/file/66191791/NR-603-Week-2-Part-2-Case-Studydocx/
symptoms fail to respond (GINA, 2020). Michelle the following are signs of worsening asthma:
difficulty breathing, confusion, dizziness, seizure, not urinating, fever or cough that improves but
then returns or worsens, and severe weakness (CDC, 2019). You will need to return to the office
in 1 week for re-evaluation of the symptoms and treatment. Early follow-up after an exacerbation
of no longer than 7 days is recommended (GINA, 2020 & Kennedy-Malone, et al., 2019).
Ben
References:
Castillo, J., Peters, S., & Busse, W. (2017). Asthma exacerbations: pathogensis, prevention, and
treatment. Journal of Allergy Clinical Immunology Practice, 5 (4): 918-927. Doi:
10.1016/j.jaip.2017.05.001
Center for Disease Control and Prevention (2019). Flu and People with Asthma.
https://www.cdc.gov/flu/highrisk/asthma.htm
Gaitonde, D., Moore, F., & Morgan, M. (2019). Influenza: diagnosis and treatment. American
Family Physician. Aafp.org/dam/AAFP/documents/journals/afp/influenza.pdf
Global Initiative for Asthma (2020). Pocket Guide for Asthma Management and Prevention.
https://ginasthma.org/wp-content/uploads/2020/04/Main-pocket-guide_2020_04_03-finalwms.pdf
Kennedy-Malone, L., Martin-Plank, L., & Duffy, E. (2019). Advanced Practice Nursing in the
Care of Older Adults (2nd ed). F.A. Davis Company: Philadelphia, PA.
Uyeki, T., Bernstein, H., Bradley, J., Englund, J., File Jr, T., Fry, A., Gravenstein, S., Hayden, F.,
Harper, S., Hirshon, J., Ison, M., Johnston, L., Knight, S., McGeer, A., Riley, L., Wolfe, C.,
Alexander, P., & Pavia, A. (2019). Clinical practice guidelines by the infectious diseases society
of America: 2018 update on diagnosis, treatment, chemoprophylaxis, and institutional outbreak
management of seasonal influenza. Clinical Infectious Diseases, 68 (6): e1-e47.
https://doi.org/10.1093/cid/ciy866
[Show More]


 (1).png)