Determine appropriate treatment plan for Michelle. Discuss medications, doses,
Durable Medical Equipment, and any testing, and apply these directly to her case.
Provide your rationale with evidence.
Treatment Plan:
P
...
Determine appropriate treatment plan for Michelle. Discuss medications, doses,
Durable Medical Equipment, and any testing, and apply these directly to her case.
Provide your rationale with evidence.
Treatment Plan:
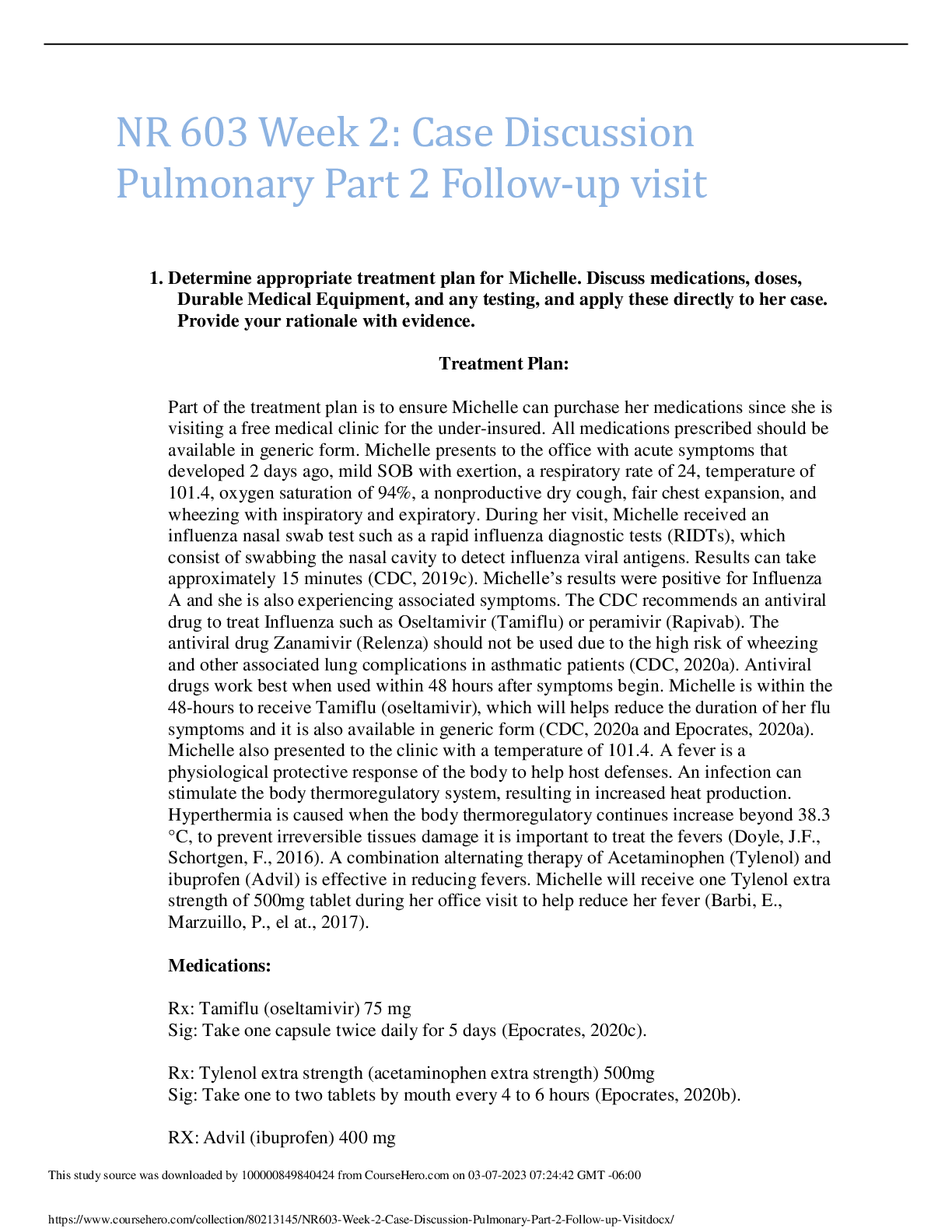
Part of the treatment plan is to ensure Michelle can purchase her medications since she is
visiting a free medical clinic for the under-insured. All medications prescribed should be
available in generic form. Michelle presents to the office with acute symptoms that
developed 2 days ago, mild SOB with exertion, a respiratory rate of 24, temperature of
101.4, oxygen saturation of 94%, a nonproductive dry cough, fair chest expansion, and
wheezing with inspiratory and expiratory. During her visit, Michelle received an
influenza nasal swab test such as a rapid influenza diagnostic tests (RIDTs), which
consist of swabbing the nasal cavity to detect influenza viral antigens. Results can take
approximately 15 minutes (CDC, 2019c). Michelle’s results were positive for Influenza
A and she is also experiencing associated symptoms. The CDC recommends an antiviral
drug to treat Influenza such as Oseltamivir (Tamiflu) or peramivir (Rapivab). The
antiviral drug Zanamivir (Relenza) should not be used due to the high risk of wheezing
and other associated lung complications in asthmatic patients (CDC, 2020a). Antiviral
drugs work best when used within 48 hours after symptoms begin. Michelle is within the
48-hours to receive Tamiflu (oseltamivir), which will helps reduce the duration of her flu
symptoms and it is also available in generic form (CDC, 2020a and Epocrates, 2020a).
Michelle also presented to the clinic with a temperature of 101.4. A fever is a
physiological protective response of the body to help host defenses. An infection can
stimulate the body thermoregulatory system, resulting in increased heat production.
Hyperthermia is caused when the body thermoregulatory continues increase beyond 38.3
°C, to prevent irreversible tissues damage it is important to treat the fevers (Doyle, J.F.,
Schortgen, F., 2016). A combination alternating therapy of Acetaminophen (Tylenol) and
ibuprofen (Advil) is effective in reducing fevers. Michelle will receive one Tylenol extra
strength of 500mg tablet during her office visit to help reduce her fever (Barbi, E.,
Marzuillo, P., el at., 2017).
Medications:
Rx: Tamiflu (oseltamivir) 75 mg
Sig: Take one capsule twice daily for 5 days (Epocrates, 2020c).
Rx: Tylenol extra strength (acetaminophen extra strength) 500mg
Sig: Take one to two tablets by mouth every 4 to 6 hours (Epocrates, 2020b).
RX: Advil (ibuprofen) 400 mg
Sig: Take one pill every four hours or two pills every 6 to 8 hours (Epocrates, 2020c).
This study source was downloaded by 100000830772748 from CourseHero.com on 05-12-2022 08:30:07 GMT -05:00
https://www.coursehero.com/file/80213145/NR603-Week-2-Case-Discussion-Pulmonary-Part-2-Follow-up-Visitdocx/
2. Decide whether she is safe to return home, include any prescriptions, or if a referral
to a higher level of care is required. Discuss the criteria used to make your decision,
how a referral is made and defend your position.
Michelle is also experiencing an exacerbation of her asthma due to an acute illness of
influenza A. Based on the Global Initiative for Asthma (GINA), an asthma exacerbation
can be treated in the primary care setting. A physical examination can determine the
severely of the exacerbation and the need for emergency care. Exacerbation with the
presents of drowsiness, confusion, respiratory rate greater than 30, accessory muscle
use, heart rate of 120 or greater, and oxygen saturation less than 90% require emergency
care (GINA, 2020). Michelle’s current symptoms do not warrant emergency care or a
referral to pulmonologist since she has controlled asthma. Michelle can be treated in a
primary care setting and can be home with the prescriptions listed above. Michelle will
be instructed to use her inhaler as needed for respiratory symptoms at home. Since
Michelle is having wheezing, she will receive an albuterol treatment before leaving the
office. Michelle will be instructed to seek emergency care if she experiences any of the
following symptoms such as shortness of breath, chest pain, abdominal pressure,
seizures, unable to urinate, persistent dizziness, confusion, severer muscle pain or
weakness, worsening of fever or cough after improvement and the worsening of preexisting chronic condition(s) (CDC, 2020a). If Michelle chronic symptoms worsen an
admission to hospital maybe needed and a pulmonologist can be consulted as needed
(GINA, 2020).
3. Discuss relevant education and follow up plan.
Influenza incubation period is about 1 to 4 days after initial exposure. The shedding of
the virus usually occurs one day before the onset of symptoms, this is when the virus
can be spread. Michelle will be instructed to self-isolate for at least 24-hours to void the
spread of the virus to others. She will also be instructed to take her medications as
prescribed and intake adequate fluids (MacPherson, & Ho, 2016). Since Michelle is a
high-risk patient due to her asthma, she will receive education on the importance of
receiving the influenza vaccine yearly (CDC, 2019b). Influenza is a self-limited
condition with a recovery period of 3 to 7 days and usually only requires supportive care
for symptoms. Unless Michelle condition worsens no follow-up, appointment is needed
at this time. However, Michelle will receive a wellness call in 1 week for a status
update. (Ghebrehewet, MacPherson, & Ho, A., 2016). Before leaving the office,
Michelle will receive an action plan and instructed to seek emergency care if she
experiences any emergency warning symptoms (GINA, 2020).
[Show More]


 (1).png)