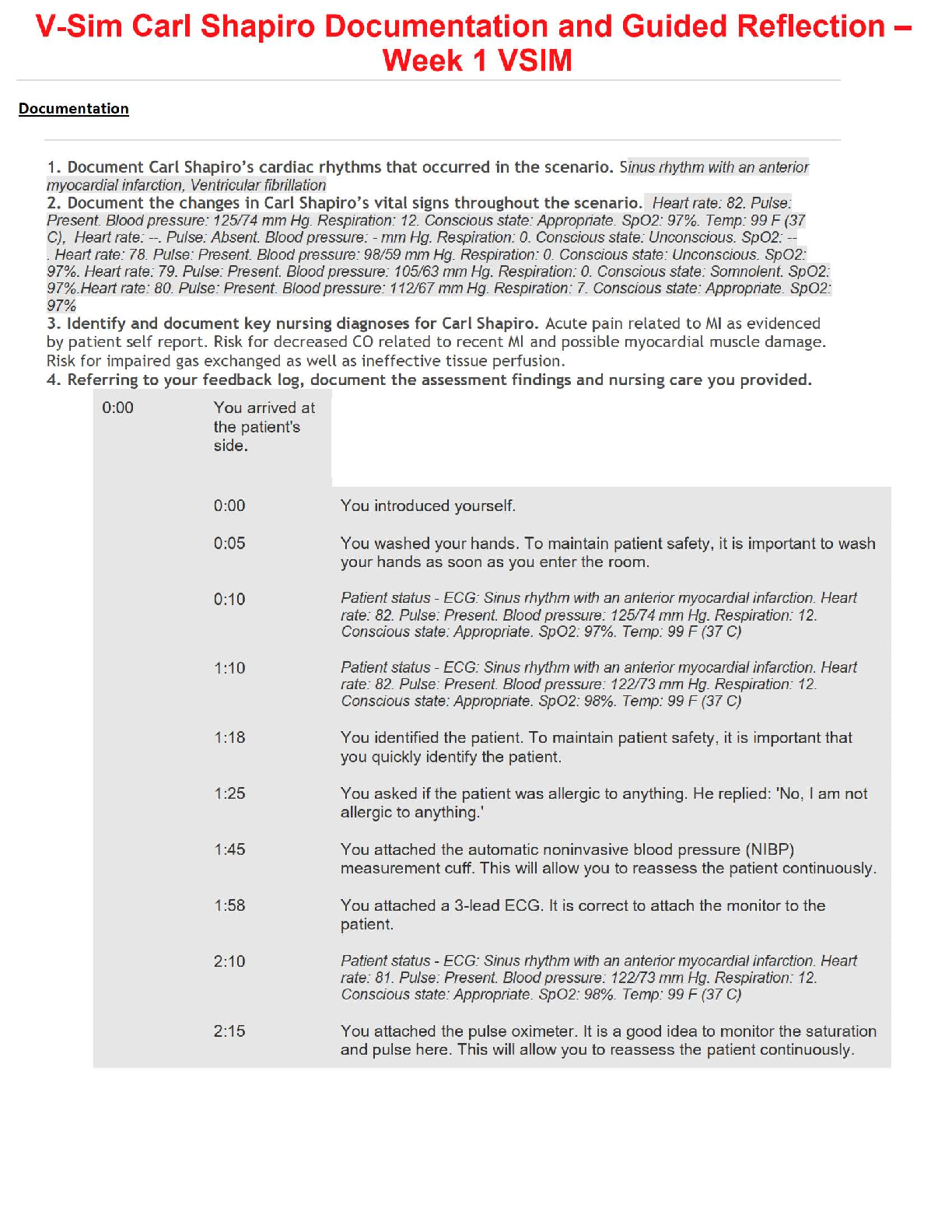
Patient Introduction
Charlie Snow is a 6-year-old Caucasian male staying with his aunt and uncle while his
parents are serving overseas in the military. Charlie presents in the emergency
department with tachycardia an
...
Patient Introduction
Charlie Snow is a 6-year-old Caucasian male staying with his aunt and uncle while his
parents are serving overseas in the military. Charlie presents in the emergency
department with tachycardia and dyspnea with mild stridor. His aunt and uncle report
that he accidentally ate a cookie containing peanuts, and he has peanut allergies. When
Charlie began having difficulty breathing, they rushed him to the emergency
department.
He is currently able to talk through the dyspnea and is on a nasal cannula at 2 liters. A
saline lock has been placed in his left arm. He has been connected to a cardiac/apnea
monitor with a SpO2 probe in place. Charlie is in bed, and the health care provider has
been notified of Charlie's arrival.
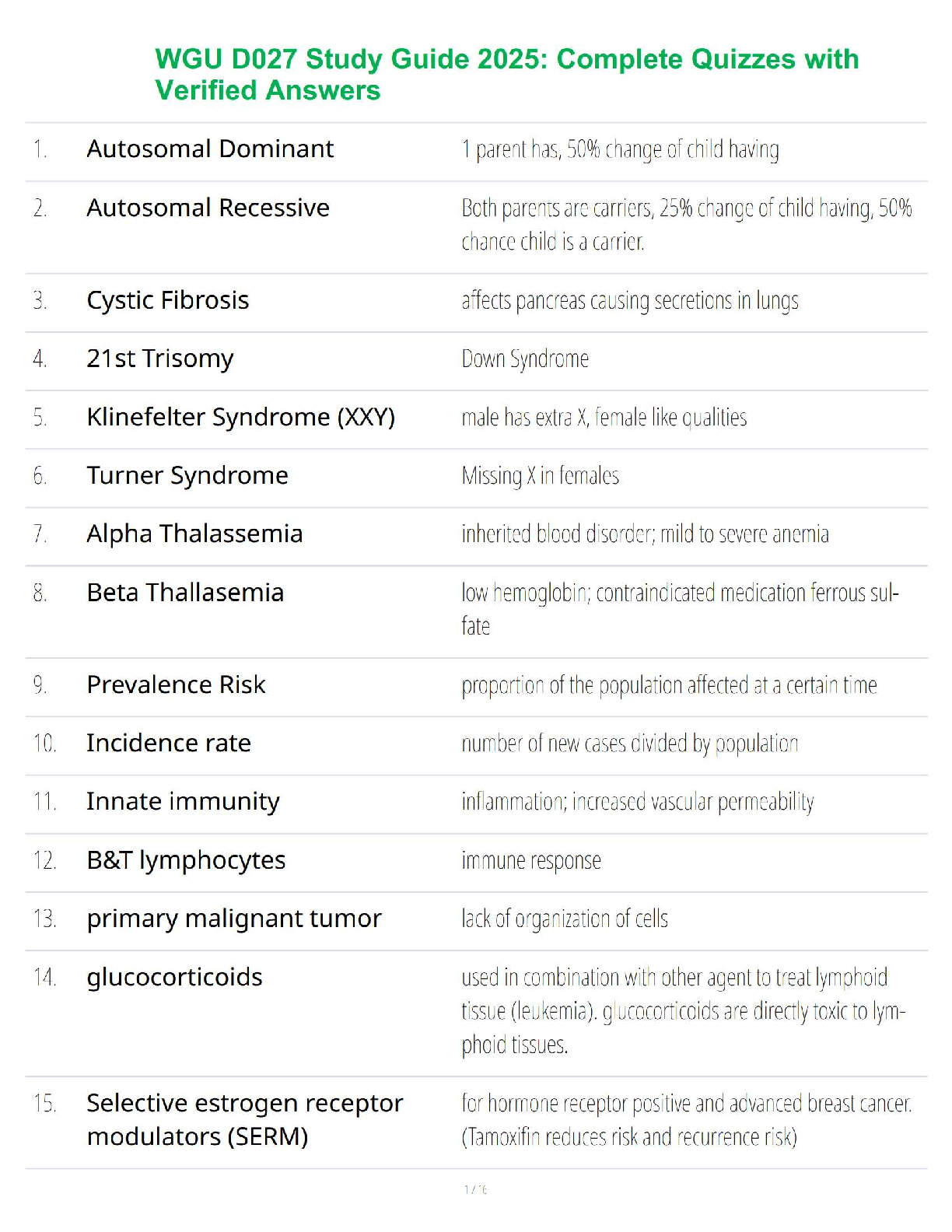
Therapeutic Levels for DRUGS
Name of Drug: Diphenhydramine hydrochloride
Therapeutic Level/Peak Level; 25 and 112 ng/mL
Antihistaminic effect: 30−50 ng/mL; sedative effect: 50−300 ng/mL
Name of Drug: Epinephrine
Therapeutic Level/Peak Level; 0.3 to 0.5 mg (0.3 mL to 0.5 mL)
Name of Drug: Methylprednisolone
Therapeutic Level/Peak Level; 30 to 200 ng/ml
Name of Drug: Ranitidine hydrochloride
Therapeutic Level/Peak Level; 36 to 94 ng/mL.
Name of Drug: Diphenhydramine hydrochloride
Therapeutic Class: Allergy, cold and cough remedy, antihistamine, antitussive
Pharmacologic Class: Antihistamine
Therapeutic Level/Peak Level: PO: Peds: 6–11 yr. Allergic reactions or motion sickness—
12.5–25 mg q 4–6 hr prn (max: 150 mg/day). Antidyskinetic—
0.5–1 mg/kg q 6–8 hr prn (max: 300 mg/day). Antitussive—12.5 mg q
4 hr prn (max: 75 mg/day).
IV: Peds: 1.25 mg/kg q 6 hr prn (max: 300 mg/
day)
List the indication for each medication:
Allergy, anaphylaxis, sedation, motion sickness, antitussive
The nursing interventions associated with each drugs are:
Assess purpose of medication prior to administration as applicable to individual patient.
- Assess for urticaria and for patency of airway.
- Assess allergy signs/symptoms such as EPS, N/V, skin condition, sleep patterns, cough, and
lung sounds
- Anticholinergic effects (dry mouth, nausea, chest tightness, thick secretions, hypotension,
blurred vision, headache, blurred vision, constipation, sedation)
- Caregiver/patient should avoid other over-the-counter cough and cold remedies
Patient Teachings:
- Educate parents or caregivers about proper dosage because an overdose, especially in infants
and children, can cause hallucinations, seizures, or death.
- Educate parents/caregivers on sleep hygiene techniques such as dark room, quiet, bedtime
ritual, limit daytime napping.
- Educate parents/caregiver to use sunscreen and protective clothing to prevent photosensitivity
reactions.
- Educate parent/caregiver to stop giving medication 4 days before diagnostic skin tests;
antihistamines can prevent, reduce, or mask positive skin test response.
Name of Drug: Epinephrine
Therapeutic Class: Antiasthmatics, bronchodilator, vasopressor
Pharmacologic Class: Adrenergic agonist
Therapeutic Level/Peak Level: 0.01 mg/kg (0.01 ml/kg of a 1:1,000 solution) or 0.3
mg/m2
(0.3 ml/ m2 of a 1:1,000 solution) S.C. Dose not to exceed 0.5 mg. May be repeated at
20-minute to 4-hour intervals, p.r.n. Or 0.02 to 0.025 mg/kg (0.004 to 0.005 ml/kg) or 0.625
mg/m2
(0.125 ml/m2
) of a 1:200 solution. May be repeated but not more often than q 6
hours. Or 0.1 mg (10 ml of a 1:100,000 dilution) I.V. slowly over 5 to 10 minutes followed by
a 0.1 to 1.5 mcg/ kg/minute I.V. infusion. Children 30 kg (66 lbs) Or More
0.3 to 0.5 mg (0.3 to 0.5 mL) to
IV: Peds: Anaphylactic reactions—0.01 mg/kg q 20 min.- 0.3 mg (0.3 mL) per injection,
repeated every 5 to 10 minutes
IV: Peds: Anti-inflammatory/Immunosuppressive—0.5–1.7 mg/kg/day or 5–25 mg/m2/day in
divided doses q 6–12 hr.
List the indication for each medication:
Asthma and COPD exacerbations, allergic reactions, cardiac arrest, anesthesia adjunct
Patient Teaching:
- Teach parents or caregivers signs and symptoms of anaphylaxis, how to use auto-injector safely,
and to get the child to a hospital as soon as possible.
- Teach parent to discuss allergy and use of auto-injector with responsible adult.
- Maintain adequate fluid intake (2000–3000 mL/day) to help liquefy tenacious secretions.
- Educate caregiver/parent to consult HCP if respiratory symptoms are not relieved or worsen
after treatment or if chest pain, headache, severe dizziness, palpitations, nervousness, or
weakness occurs.
- Educate caregiver/parent on medication administration steps, placement and to only give two
sequential doses
- Educate parent/caregiver to seek immediate care and report adverse reactions immediately to
HCP.
The nursing interventions associated with each drug are:
Patient harm or fatalities have occurred from medication errors with epinephrine.
Side effects include angina, tachycardia, hypertension, restlessness, nervousness, hyperglycemia
• Use with MAOI may lead to hypertensive crisis
Administer the rights for medication administration due to patient harm or fatalities occurring
from medication errors
- Assess lung sounds, pulse, BP, and other hemodynamic parameters such as blood glucose
monitoring
- Instruct caregiver/patient to use as directed
- Caregiver/patient should ensure adequate fluid intake to liquefy secretions
- Caregiver must enforce rinsing of mouth after inhalation
Name of Drug: Methylprednisolone
Therapeutic Class: Antiasthmatics, corticosteroids
Pharmacologic Class: Corticosteroids
Therapeutic Level/Peak Level: Peds: Anti-inflammatory/
Immunosuppressive—0.5–1.7 mg/kg/day or 5–25 mg/m2/day in divided doses q 6–12 hr.
List the indication for each medication:
Inflammation, allergy, autoimmune disorders, prevent organ rejection
The nursing interventions associated with each drugs are:
- Decrease wound healing
- Assess blood sugar, cholesterol, and lipid levels.
- Assess for signs of infection (sore throat)
Monitor intake and output ratios and daily weights. Observe patient for peripheral edema, steady
weight gain, rales/crackles, or dyspnea. Notify health care professional if these occur.
Children should have periodic evaluations of growth.
Patient Teaching
Caution patient to avoid vaccinations without first consulting health care professional.
Instruct patient to notify health care professional immediately if exposed to chicken pox or measles.
Instruct patient to notify health care professional of all Rx or OTC medications, vitamins, or herbal
products being taken and to consult health care professional before taking any Rx, OTC, or herbal
products.
Advise patient to notify health care professional of medication regimen before treatment or surgery.
Discuss possible effects on body image. Explore coping mechanisms.
Instruct patient to inform health care professional if symptoms of underlying disease return or worsen.
Advise patient to carry identification describing disease process and medication regimen in the event of
emergency in which patient cannot relate medical history
Potential Nursing Diagnoses
Risk for infection (Side Effects)
Disturbed body image (Side Effects)
[Show More]