NUR 114 Partial Focus Notes Final Fall 2019
This does not include any of Ms. Jordans lectures only for McLean and Ms. Pizzotti’s
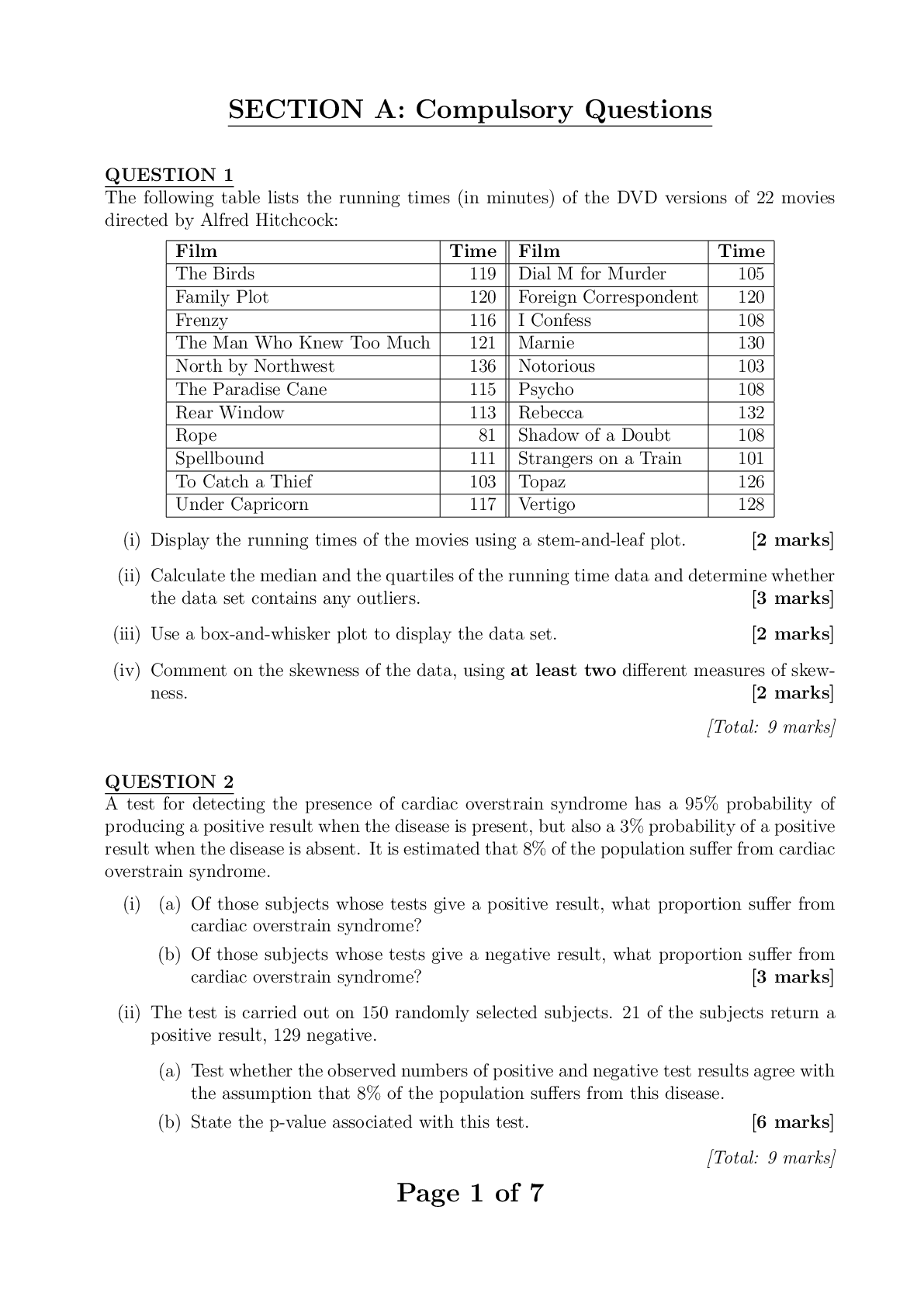
Conversions, medication math for PO, IV rates mcg/min, ml/min, gtts/min, mcg/kg/min
CONC
...
NUR 114 Partial Focus Notes Final Fall 2019
This does not include any of Ms. Jordans lectures only for McLean and Ms. Pizzotti’s
Conversions, medication math for PO, IV rates mcg/min, ml/min, gtts/min, mcg/kg/min
CONCEPT OF SEXUALITY
• Recommendations for testing and assessment for PAP smears, Breast cancer, Prostate CA,
Testicular CA. HPV
◦ PAP SMEAR:
▪ a cytological study that is effective in detecting precancerous and cancerous cells within the
female patient’s cervix.
▪ When to get tested:
• Not recommended for women under 21 (unless SEXUALLY ACTIVE)
• 21-29 every 3 years
• 30-65 every 5 years + HPV test
• 65+ whom has had normal Pap’s in the past should not receive pap test.
• Other’s suggest 60+ every 3 years
• Those who have had a Hx of cervical cancer should get tested yearly for at least 20 years
after the diagnoses regardless of age.
◦ HPV test: can identify many high-risk types of HPV infections associated with the development
of cervical cancer.
▪ When to get tested:
• At the time of a pap for women 30+
• for any woman of any age who have had an abnormal pap result.
◦ PSA test:
▪ a prostate-specific antigen test is used to screen for prostate cancer and to monitor the disease
after treatment.
▪ Normal lab value: 0-2.5
▪ An elevated PSA should decrease a few days after a prostatectomy. If it has not it shows that
it has reoccurred.
▪ Elevated numbers are associated with prostate cancer.
▪ Older men (Esp. AA men) often have a higher PSA.
▪ Should be drawn before a digital rectal exam because the exam can cause an increase in PSA
due to prostate irritation.
◦ Mammogram: ** 40 is the magic number
▪ A mammogram is a x-ray of the soft tissue of the breast. Mammograms assess differences in
the density of breast tissue.
▪ Helpful in evaluating poorly defined masses, multiple masses or nodules, nipple discharge or
changes, skin changes, or pain.
▪ AGE INFORMATION:
• Women ages 40 to 44 should have the choice to start annual breast cancer if they wish –
Women age 45 to 54 should get mammograms every year.
• Women aged 40 years and older be offered screening mammography annually
• Women age 55 and older should switch to mammograms every 2 years, or have the
choice to continue yearly screening.• American College of Obstetricians and Gynecologists recommends annual screening
mammography for women age 40 and over
• Yearly screening is recommended at age 40 because younger women have higher
density in breast tissue and the test is less effective.
▪ In older women, the amount of fatty tissue is higher. Therefore, fatty tissues appear lighter
than cancer
▪ Cancer and cysts usually have the same density. However, cysts are smooth borders and
cancers are usually star-burst shape
◦ Testicular Cancer:
▪ Rare form of cancer that most often effects men between ages of 20-35 years of age.
▪ With early detection there is a 95% cure rate
▪ Most common type is germ cell tumors arising from sperm-producing cells
• Seminoma tumors are usually localized, metastasize late, and respond to treatment.
▪ Least common type is non-germ cell tumors in stromal, interstitial, or Leydig cells
• Most do not metastasize
• Adroblastomas sometimes secrete estrogen, which causes feminization and gynecomastia
▪ Men with cryptocordism or HIV have higher risk of testicular tumors.
▪ Common tumor markers that confirm testicular cancer are alfa-fetoprotein, hCG, and LDH
• What are the types and s/s of benign breast disorders?
Benign Breast disorders
1. Fibroadenoma
o Most common benign tumor in women during reproductive years
o Mass of connective tissue unattached to surrounding breast tissue
o Tumors are oval, freely movable, rubbery
2. Fibrocystic Breast Condition (FBC)
o Fibrocystic changes of breast (may involve lobules, ducts, stromal tissues)
o Common in pre-menopausal women between 20 and 50 years of age
o Thought to be caused by imbalance in normal estrogen-to-progesterone ratio
o Symptoms: Breast pain, tender lumps, swelling (often before menstrual period)
o Two main features of FBC: fibrosis and cysts
Fibrosis made up of connective tissue and are hard and firm
Cysts are fluid filled and glandular cells – Breast US is used to confirm presence of
cysts.
o Postmenopausal women taking hormonal replacement may develop FBC or have worsening
symptoms.
o This does not increase her chances of Breast CANCER; however, if a firm mass arises a
mammogram may be done to rule out cancer
o A needle biopsy may be done to rule out cancer IF:
No fluid is aspirated Mammogram is positive
Mass remains palpable after aspiration
Aspirated fluid reveals cancer cells
o Management of FBC:
Analgesics
Limit salt intake before menses
Wear supportive bra at all times
Ice or heat may help
Reduce or eliminate caffeine, dairy product
Needle aspiration may be necessary
diuretics
Oral contraceptives or selective estrogen receptor modulators may be prescribed
o Explain to women the benefits and risks associated with hormonal drug therapy for FBC,
such as stroke, liver disease, and increased intracranial pressure. Teach them to seek medical
attention immediately if any signs or symptoms of these complications occur.
3. Ductal Ectasia
o Benign breast problem of women approaching menopause
o Caused by dilation and thickening of collecting ducts in subareolar area
o Hard mass; irregular borders, tender
o Greenish-brown nipple discharge, enlarged axillary nodes, redness and edema over mass
o Management
May improve without treatment
Reduce anxiety regarding threat of breast cancer
Warm compresses
Antibiotics
May require surgical removal
4. Intraductal Papilloma
o Occurs most often in women 40 to 55 years of age
o Benign process in epithelial lining of duct, forming a pedunculated outgrowth of tissue
o Trauma and erosion within duct; bloody or serous nipple discharge
o Mass is rarely palpableo Must rule out breast cancer
Breast cancer types, S/S, High risk groups, risk factors, treatments, diagnostics
Invasive VS noninvasive:
• There are two broad categories of breast cancer: noninvasive and invasive. Most of these
cancers arise from the intermediate ducts.
a. Non-invasive cancers account of about 20% of BC – occurs when the cancer remains
within the duct.
b. Invasive BC is the other 80% – occurs when the BC penetrates the surrounding tissue
around the duct.
• Metastasis occurs when the cancer cells leave the breast via blood or lymph fluid – permits
spread of cancerous cells to distant sites
• Common sites of metastasis are lung, bone, brain, and liver.
Noninvasive Breast Cancers
• Ductal carcinoma in situ (DCIS)
◦ early noninvasive form of breast cancer
◦ cancer cells located within the duct – have not invaded the surrounding fatty breast
tissue.
◦ mammography screening and earlier detection has caused the # of women diagnosed
with DCIS to >
◦ left untreated, it is estimated that 14% to 53% of DCIS would become invasive and
spread into the breast tissue surrounding the ducts over a period of 10 years
◦ Currently there is no way to determine which DCIS lesions will progress to invasive
cancer and which ones will remain unchanged – causes anxiety and decisional
conflict in many women diagnosed with this
◦ differs from invasive cancer – DCIS cells lack the biologic capacity to metastasizs
• lobular carcinoma in situ (LCIS)
◦ rare and occurs as an abnormal cell growth in the lobules (milk-producing glands) of
the breast
◦ not a true cancer, but having LCIS increases one's risk for developing a separate
breast cancer later
◦ usually diagnosed before menopause in women 40 to 50 years of age.
◦ Traditionally, treated with close observation only
◦ Women with LCIS and other breast cancer risk factors may want to consider
prophylactic treatment options such as tamoxifen, raloxifene, or prophylactic
mastectomy
Invasive Breast Cancers
• Infiltrating ductal carcinoma
◦ most common type of invasive breast cancer
◦ originates in the mammary ducts and grows in the epithelial cells lining these ducts
◦ Once invasive, the cancer grows into the tissue around it in an irregular pattern
◦ If a lump is present, it is felt as an irregular, poorly defined mass
◦ As tumor continues to grow, fibrosis (replacement of normal cells with connective tissue and
collagen) develops around the cancer▪ fibrosis may cause shortening of Cooper's ligaments – resulting typical skin dimpling –
Late sign
▪ another late sign: edematous thickening and pitting of breast skin called peau d'orange
(orange peel skin)
• inflammatory breast cancer
◦ rare but highly aggressive form of invasive breast cancer
◦ Symptoms include swelling, skin redness, and pain in the breasts.
◦ IBC seldom presents as a palpable lump and may not show up on a mammogram
◦ usually diagnosed at a later stage than other types of breast cancer – often harder to treat
successfully
Mutations
1. BRCA1 and BRCA2, are related to hereditary breast cancer
2. People who have specific mutations in either one of these genes are at a high risk for developing
breast cancer as well as ovarian cancer
3. only 5% to 10% of all breast cancers are hereditary
4. Only women with a strong family history and a reasonable suspicion that a mutation is present have
genetic testing for BRCA mutations.
Other BC information
• Estrogen and progesterone receptor-negative cancers:
◦ harder to treat because the drug choices and treatment options are limited at they will not affect
the cancer.
• HER2 receptors
◦ Human epithelial receptors are in normal breast and help them grow.
◦ In some breast cancers there are way too many and the cancer grows rapidly
• REMEMBER these are Signs in LATE stages cancers:
• dimpling may occur due to shortening of cooper’s ligaments
◦ caused by fibrosis which is the replacement of normal cells with connective tissue and
collagen
• Peau d’orange is visible with edema of the breast (peeling of orange skin)
◦ Edematous thickening and pitting of the breast skin
How to preform Self breast exam. Patient teaching.
o Self-Breast EXAM steps:
Lie down on your back and place your right arm behind your head
Use the finger pads of the three middle fingers on your left hand to feel for lumps in
the right breast. Use an overlapping dime shaped circular motion to feel for lumps
Use three different levels of pressure to feel. Light feels closest to the skin, medium
is a little deeper, and firm pressure feels close to the chest wall.
It is normal to feel a curved ridge in the lower curve of each breast
Move around the breast in an up and down pattern starting at an imaginary line
drawn straight down your side from the underarm and moving across the breast to the
middle of the chest bone. Be sure to check the entire breast area going down until
you feel the ribs and up to the neck.
Repeat on the left side
While standing, exam the size, shape, contour, dimpling, and look at nipples. Stand
with arms by your side in front of a mirror.
Exam under the arms with your arm elevated only slightly.o Assessing a breast mass
Identify the location of the mass by using the face of a clock method
Describe the shape, size, and consistency of the mass
Assess whether the mass is fixed or movable
Note any skin changes ( dimpling, peau d’orange)
Assess axillary and supraclavicular lymphatic nodes
Ask patient if they experience pain or soreness in the area of the mass
Care of the patient pre and post op Mastectomy and breast reconstruction
postoperative care for a Mastectomy:
o Sign in room and inform staff to not use the affected arm
o Assess vitals every 30 mins for 2 hrs and every hour for 2 hours, and then every 4 hours.
o Check dressing for bleeding
o Monitor for amount and color of drainage
o Assess position to make sure drainage system is not being pulled nor kinked
o HOB 30 degrees
o Elevated affect arm
o Basic comfort measures
o Analgesics
o Ambulation and regular diet begin day after surgery
o During a modified radical mastectomy
the surgeon places one or two drainage tubes, usually Jackson-Pratt drains, under the
skin flaps and attaches the tubes to a small collection chamber.
Gentle suction is exerted, and fluid that would accumulate under the flaps and delay
healing is collected.
When taking vital signs, monitor for the amount and color of drainage. Add this
information to the intake and output record.
o Patients undergoing a lumpectomy may also have drainage tubes (usually Jackson-Pratt
drains) placed if the lump is large or if axillary node dissection is performed.
o Assess the incision and flap of the post-mastectomy patient for signs of bleeding, infection,
and poor tissue perfusion.
o With short hospital stays, drainage tubes are usually removed about 1 to 3 weeks after
hospital discharge when the patient returns for an office visit.
The drainage amount should be less than 25 mL in a 24-hour period
Inform the patient that tube removal may be uncomfortable although these tubes lie
just under the skin
Provide or suggest analgesia before they are removed
Document all findings, and report any abnormalities to the surgeon immediately.
o Instruct the patient to avoid the hunched-back position with the arm flexed because of the risk
for elbow contractures
o Beginning exercises that do not stress the incision can usually be started on the first day after
surgery.
These exercises include squeezing the affected hand around a soft, round object (a
ball or rolled washcloth) and flexion/extension of the elbow. Postoperative mastectomy exercises:
o Hand-wall climbing:
Face the wall and place hands on wall at shoulder level
Flex your fingers so that your finger walk up the wall
Stop when your arms feel fully exerted
Slowly “walk” back down the wall
o PULLEY:
drape a 6 ft long rope over a curtain or door. Grab the ends of the rope and extend
your arms out to the sides
Keeping your arms straight go down with the left and up with the right
o ROPE turning:
tie rope to knob of closed door
Hold rope with arm extended out in front of you
Swing the rope in a circular motion starting with small circles and increasing in
size.
Postoperative Care of the Patient After Breast Reconstruction
o Assess the incision and flap for signs of infection (excessive redness, drainage, odor) during
dressing changes.
o Assess the incision and flap for signs of poor tissue perfusion (duskiness, decreased capillary
refill) during dressing changes.
o Avoid pressure on the flap and suture lines by positioning the patient on her nonoperative
side and avoiding tight clothing.
o Monitor and measure drainage in collection devices, such as for Jackson-Pratt drains.
o Teach the patient to return to her usual activity level gradually and to avoid heavy lifting
o Remind the patient to avoid sleeping in the prone position
o Teach the patient to avoid participation in contact sports or other activities that could cause
trauma to the chest.
o Teach the patient to minimize pressure on the breast during sexual activity.
o Remind the patient to refrain from driving until advised by the physician.
o Remind the patient to ask at the 6-week postoperative visit when full activity can be resumed.
o Reassure the patient that optimal appearance may not occur for 3 to 6 months postoperatively.
o If implants have been inserted, teach the proper method of breast massage to enhance
expansion and prevent capsule formation (consult with the physician).
o Emphasize breast self-awareness; if the patient performs breast self-examination (BSE),
review her technique.
o Remind the patient of the importance of clinical breast examination and follow-up
surveillance by her physician.
Endometriosis s/s treatments diagnostics
o Care:
Assessment: menstrual history, sexual history, bleeding characteristics
PAIN IS THE MOST COMMON SYMPTOM OF ENDOMETRIOSIS
Usually peaks just before the menstrual flow; is usually located in the abdomen
and causes a sense of rectal pressure
Degree of pain not related to the extent, but it is related to the site Other s/s include: painful intercourse, painful defecation, low backache, infertility,
nausea, diarrhea are also common
Pelvic assessment may reveal pelvic tenderness, tender nodules in the posterior vagina,
and limited movement of the uterus.
Psychosocial assessment may reveal anxiety
Diagnostic tests to rule out PID caused by chlamydia or gonorrhea.
Serum CA-125 (cancer antigen) may be positive
Transvaginal ultrasound-determine if masses are malignant or endometriosis
a laparoscopy is the most definitive diagnosis in endometriosis
o Interventions:
Hormonal and surgical management may be used
Collaborations consists of interventions that:
Reduce pain
Restore sexual function
Alleviate anxiety r/t the disease and the uncertainty of the diagnosis
Educate the pt about the disease and its treatment
Alleviate fear r/t the possibility of laparoscopy or surgery
Prevent self-concept disturbance r/t infertility
Nonsurgical Management:
Oral contraceptive to control menstrual cycle or progestins such as:
o Oral medroxyprogesterone acetate and norethindrone acetate
o Injectable forms of progestins: medroxyprogesterone acetate (depoprovera)
Continuous low-level heat using wearable heat packs
Relaxation techniques, yoga, massage, biofeedback
Calcium and Magnesium supplements may relieve cramping
Surgical Management:
Ablation- a laprascopic removal of endometrial implants and adhesions; sameday surgery – unless you are like me and had complications :)
Surgeon may use a laser to treat endometriosis by vaporizing adhesions and
endometrial implants.
Teach pt that temporary postop pain from CO2 used during laparoscopy to better
visualize internal organs, can occurs in the shoulders or chest
Toxic Shock syndrome s/s treatments diagnostics
o Can result from menstruation and tampon use
o Other conditions associated with TSS:
Surgical wound infection
Nonsurgical infections
Gynecologic surgeries
Use of internal contraceptives
o Menstrual blood provides a growth medium for Staphylococcus aureus
exotoxins produced from the bacteria cross the vaginal mucosa to the bloodstream via
microabrasions from tampon insertion or prolonged useo Can be fatal
o Usually develops within 5 days after the onset of menstruation
o Most common s/s:
Fever
Rash
Myalgias
Sore throat
Edema
Hypotension
Rash often looks like sunburn
Broken capillaries in eyes and skin
o Treatment:
Removal of infection source (tampon, usually)
Restore fluid and electrolyte balance
Administer drugs to manage hypotension
IV antibiotics
Transfusion to reverse low platelet counts
Corticosteroids to treat skin changes
o Prevention:
Wash hands before inserting a tampon
Do not use a dirty tampon
Inset the tampon carefully to avoid injuring the delicate tissue in your vagina
Change your tampon every 3-6 hours
Do not use superabsorbent tampons
Use sanitary napkins at night
Call HCP if you suddenly experience a high temperature, vomiting or diarrhea
Do not use tampons at all if you have had TSS
Not using tampons almost guarantees that you will not get toxic shock syndrome
Menopause and Osteoporosis
Menstrual disorders (amenorrhea, dysmenorrhea)
Infertility
Family Planning Contraception and Sterilization
Premenstrual Dysphoric Disorder (PMDD)
Leiomyomas s/s treatments diagnostics, Uterine Fibroids
• fibroids that are benign, slow-growing solid tumors of uterine myometrium
• Intramural leiomyomas
◦ are contained in the uterine wall within the myometrium
• Submucosal leiomyomas
◦ protrude into the cavity of the uterus and can cause bleeding and disrupt pregnancy
• Subserosal leiomyomas
◦ protrude through the outer surface of the uterine wall and may extend to the broad ligament,
pressing other organs
• Pedunculated leiomyomas◦ are attached by a pedicle (stalk) to the outside of the uterus and occasionally break off and attach
to other tissues
• Leiomyomas are the most common reason for hysterectomies.
Prostatectomy Pre and post op care
Surgical Management:
◦ Surgery is the most common intervention for a cure
◦ Minimally invasive surgery (MIS) or, less commonly, an open surgical technique for radical
prostatectomy (prostate removal) is usually performed
◦ A bilateral orchiectomy (removal of both testicles) is another palliative surgery that slows the
spread of cancer by removing the main source of testosterone
Preoperative Care:
◦ Preoperative care depends on the type of surgery that will be done
◦ Minimally invasive surgery (MIS)
▪ most appropriate for localized prostate cancer and is used as a curative intervention
◦ The most common procedure is the laparoscopic radical prostatectomy (LRP)
▪ most often with robotic assistance
◦ Patients who qualify for LRP must have a PSA less than 10 ng/mL and have no previous
hormone therapy or abdominal surgerie.
◦ Other newer procedures include transrectal high-intensity focused ultrasound (HIFU) and
cryosurgery
Operative Procedures:
◦ For the LRP procedure, the patient is placed in lithotomy positioning with steep Trendelenburg
▪ Nurses in the OR ensure that the patient maintains a balanced body temperature and positions
the patient to prevent injury
▪ The urologist makes one or more small punctures or incisions into the abdomen
▪ A laparoscope with a camera on the end is inserted through one of the incisions while other
instruments are inserted into the other incisions
▪ The robotic system may be used to control the movement of the instruments by a remote
device
▪ The prostate is removed along with nearby lymph nodes, but perineal nerves are not affected.
◦ The open radical prostatectomy can be performed via several surgical approaches, depending on
the patient's desired outcomes and the staging of the disease
◦ The transperineal and retropubic (nerve-sparing) approaches are most commonly use
▪ The surgeon removes the entire prostate gland along with the prostatic capsule, the cuff at the
bladder neck, the seminal vesicles, and the regional lymph nodes
▪ The remaining urethra is connected to the bladder neck
▪ The removal of tissue at the bladder neck allows the seminal fluid to travel upward into the
bladder rather than down the urethral tract, resulting in retrograde ejaculations
Postoperative Care:
◦ Nursing interventions include all the typical care for a patient undergoing major surgery
▪ Maintaining hydration
▪ caring for wound drains (open procedure)▪ managing pai
▪ , and preventing pulmonary complications are important aspects of nursing care.
Care of the Patient After an Open Radical Prostatectomy
• Encourage the patient to use patient-controlled analgesia (PCA) as needed.
• Help the patient get out of bed into a chair on the night of surgery and ambulate by the next day.
• Maintain the sequential compression device until the patient begins to ambulate.
• Monitor the patient for deep vein thrombosis and pulmonary embolus.
• Keep an accurate record of intake and output, including Jackson-Pratt or other drainage device drainage.
• Keep the urinary meatus clean using soap and water.
• Avoid rectal procedures or treatments.
• Teach the patient how to care for the urinary catheter because he may be discharged with the catheter in
place.
• Teach the patient how to use a leg bag.
• Emphasize the importance of not straining during bowel movement. Advise the patient to avoid suppositories
or enemas.
• Remind the patient about the importance of follow-up appointments with the physician to monitor progress.
Pelvic Inflammatory Disease: PID
Clinical Diagnostic Criteria for PID:
◦ One or more of the following minimum criteria must be present on pelvic examination to
diagnose PID:
▪ Cervical motion tenderness
▪ Uterine tenderness
▪ Adnexal tenderness
◦ The following criteria can improve the specificity of the diagnosis:
▪ Oral temperature > 101°F (> 38.3°C)
▪ Abnormal cervical or vaginal mucopurulent discharge
▪ Presence of abundant numbers of white blood cells on saline microscopy of vaginal fluid
Elevated erythrocyte sedimentation rate
▪ Elevated C-reactive protein level
▪ Laboratory documentation of cervical infection with gonorrhea or chlamydia
◦ The following test results are the most specific criteria for diagnosing PID:
▪ Endometrial biopsy with histopathologic evidence of endometritis
▪ Transvaginal sonography or magnetic resonance imaging techniques showing thickened,
fluid-filled tubes with or without free pelvic fluid or tubo-ovarian complex, or Doppler
studies suggesting pelvic infection (e.g., tubal hyperemia)
▪ Laparoscopic abnormalities consistent with PID
Treatment:
◦ Antibiotic therapy, self-management measures and rarely surgery. If oral antibiotic therapy is not
successful, hospitalization and IV antibiotic therapy is needed.▪ Option 1 Ceftriaxone (Rocephin) 250 mg IM in a single dose plus Doxycycline 100 mg
orally twice per day for 14 days with or without Metronidazole (Flagyl) 500 mg orally twice
per day for 14 days
▪ Option 2 Cefoxitin plus 2 g IM in a single dose administered concurrently with probenecid (1
g orally) Doxycycline 100 mg orally twice per day for 14 days with or without Metronidazole
500 mg orally twice per day for 14 days
▪ Option 3 Other parenteral thirdgeneration cephalosporin (e.g., ceftizoxime [Cefizox],
cefotaxime [Claforan]) plus Doxycycline 100 mg orally twice per day for 14 days with or
without Metronidazole 500 mg orally twice per day for 14 days
◦ Teach: Patient to finish all of the antibiotics and to avoid sexual intercourse until treatment and
symptoms are gone. Sexual partners should be treated regardless of their lack of symptoms.
◦ Screening for chlamydia and gonorrhea in young women has been shown to decrease the
incidence of PID in high-risk populations
STI’S (STD’s)
• Syphilis, Herpes, Genital warts, HPV, Candidiasis, Trichomoniasis, chlamydia, Gonorrhea, s/s
treatments diagnostics
• Syphilis
◦ Syphilis is a complex sexually transmitted disease (STD) that can become systemic and cause
serious complications, including death.
◦ The causative organism is a spirochete called Treponema pallidum
◦ The infection is usually transmitted by sexual contact and blood exposure, but transmission can
occur through close body contact such as kissing.
◦ Syphilis progresses through four stages: primary, secondary, latent, and tertiary
◦ 1st stage:
▪ The appearance of an ulcer called a chancre is the first sign of primary syphilis
▪ It develops at the site of entry (inoculation) of the organism from 10 to 90 days after exposure
(3 weeks is average
▪ Chancres may be found on any area of the skin or mucous membranes but occur most often
on the genitalia, lips, nipples, and hands and in the mouth, anus, and rectum
▪ During this highly infectious stage, the chancre begins as a small papule
▪ Within 3 to 7 days, it breaks down into its typical appearance: a painless, indurated, smooth,
weeping lesion
▪ Regional lymph nodes enlarge, feel firm, and are not painful.
▪ Without treatment, the chancre usually disappears within 6 weeks; however, the organism
spreads throughout the body and the patient is still infectious.
◦ 2nd stage:
▪ Secondary syphilis develops 6 weeks to 6 months after the onset of primary syphilis
▪ During this stage, syphilis is a systemic disease because the spirochetes circulate throughout
the bloodstream
▪ Commonly mistaken for influenza, manifestations include flu-like symptoms (malaise, lowgrade fever, headache, muscular aches, sore throat) and a generalized rash
▪ There is no typical appearance of this rash except for its presence on the palms and soles of
the feet and on mucous membranes▪ It can appear as diffuse macules (reddish brown), papules (usually less than 5 mm) or
pustules, scaly psoriasis-like lesions or gray-white wart-like lesions (condylomata lata)
▪ All of these lesions are highly contagious and should not be touched without gloves
▪ Patchy alopecia on the scalp or facial hair (missing part of the eyebrow, “moth-eaten”
appearance) is another symptom
▪ The rash subsides without treatment in 4 to 12 weeks.
◦ 3rd stage:
▪ After the second stage of syphilis, there is a period of latency
▪ Early latent syphilis occurs during the first year after infection, and infectious lesions can
recur
▪ Late latent syphilis is a disease of more than 1 year's duration after infection
▪ This stage is not infectious except to the fetus of a pregnant woman
▪ Patients with latent syphilis may or may not have reactive serologic test (e.g., Venereal
Disease Research Laboratory [VDRL]) findings)
◦ 4th stage:
▪ Tertiary, or late, syphilis occurs after a highly variable period, from 4 to 20 years
▪ This stage develops in untreated cases and can mimic other conditions because any organ
system can be affected
▪ Manifestations of late syphilis include:
• Benign lesions (gummas) of the skin, mucous membranes, and bones
• Cardiovascular syphilis, usually in the form of aortic valvular disease and aortic aneurysms
• Neurosyphilis, causing central nervous system symptoms (e.g., meningitis, hearing loss,
generalized paresis [weakness])
◦ Conduct a physical examination, including inspection and palpation, to identify manifestations of
syphilis. Wear gloves while palpating any lesions because of the highly contagious treponemes
that are present. Observe for and document rashes of any type because of the variable presentation
of secondary syphilis.
◦ After the physical examination, the health care provider obtains a specimen of the chancre for
examination under darkfield microscope
▪ Diagnosis of primary or secondary syphilis is confirmed if T. pallidum is present.
◦ Blood tests are also used to diagnose syphilis.
▪ The usual screening and/or diagnostic nontreponemal tests are the Venereal Disease Research
Laboratory (VDRL) serum test and the more sensitive rapid plasma reagin (RPR).
▪ These tests are based on an antibody-antigen reaction that determines the presence and
amount of antibodies produced by the body in response to an infection by T. pallidum.
▪ They become reactive 2 to 6 weeks after infection
▪ VDRL titers are also used to monitor treatment effectiveness
▪ The antibodies are not specific to T. pallidum, and false-positive reactions often occur from
such conditions as viral infections, hepatitis, and systemic lupus erythematosus
▪ If a VDRL result is positive, the health care provider requests or the laboratory may
automatically perform a more specific treponemal test, such as the fluorescent treponemal
antibody absorption (FTA-ABS) test or the microhemagglutination assay for T. palladum
(MHA-TP), to confirm the infection
Drug Therapy for Syphilis
◦ Benzathine penicillin G given IM as a single 2.4 million-unit dose is the evidence-based treatment
for primary, secondary, and early latent syphilis◦ Patients in the late latent stage receive the same dose every week for 3 weeks
◦ A different regimen, found in the CDC's STD Treatment Guidelines, is recommended for patients
who are HIV-infected or pregnant.
Genital Herpes
Pathophysiology:
◦ Genital herpes (GH) is an acute, recurring, incurable viral diseases
◦ Two serotypes of herpes simplex virus (HSV) affect the genitalia:
▪ type 1 (HSV-1) and type 2 (HSV-2)
▪ Most nongenital lesions such as cold sores are caused by HSV-1, transmitted via oral-oral
contact.
▪ Historically, HSV-2 caused most of the genital lesions; however, this distinction is academic
because the transmission, symptoms, diagnosis, and treatment are nearly identical for the two
types
▪ Either type can produce oral or genital lesions through oral-genital or genital-genital contact
with an infected person.
▪ HSV-2 recurs and sheds asymptomatically more often than HSV-1
▪ Most people with GH have not been diagnosed because they have mild symptoms and shed
virus intermittently
◦ The incubation period of genital herpes is 2 to 20 days, with the average period being 1 week.
Many people do not have symptoms during the primary outbreak. When subsequent outbreaks of
genital herpes occur, they are usually more severe and occasionally require hospitalization.
ASSESSMENT OF GH
◦ The diagnosis of GH is based on the patient's history and physical examination
◦ Ask the patient if he or she felt itching or a tingling sensation in the skin 1 to 2 days before the
outbreak, known as the prodrome
◦ These sensations are usually followed by the appearance of vesicles (blisters) in a typical cluster
on the penis, scrotum, vulva, vagina, cervix, or perianal region at the site of inoculation
◦ The blisters rupture spontaneously in a day or two and leave painful ulcerations that can become
extensive
◦ Assess for other symptoms such as headaches, fever, general malaise, and swelling of inguinal
lymph nodes.
◦ Ask if urination is painful. External dysuria is a painful symptom when urine passes over the
eroded areas. Patients with urinary retention may need to be catheterized.
◦ After the lesions heal, the virus remains in a dormant state in the sacral nerve ganglia.
Periodically, the virus may activate and symptoms recur.
▪ These recurrences may be triggered by many factors, including stress, fever, sunburn, poor
nutrition, menses, and sexual activity.
Antiviral drugs are used to treat GH
Acyclovir (Zovirax, Avirax image), famciclovir (Famvir), or valacyclovir (Valtrex) may be prescribed
Condylomata Acuminata (Genital Warts):
• Encourage women to have a Pap test annually, starting at age 21 years; after they have had three
normal smears, they should have a Pap test every 3 years if no new risk factors are present (e.g., new
partner, other STDs)
• The presence of warts should increase suspicion that the patient may have had exposure to other
STDs, which warrants additional testing
• VACCINES:◦ Gardasil protection from human papilloma virus cervical cancer, genital warts, and cancer
of the anus, vagina, and vulva
▪ Approved for use in male and female patients ages 9–26
◦ Gardasil 9 same protection as the original Gardasil, plus protection against five additional types
of high-risk HPV
▪ Approved for use in male patients ages 9–15 and female patients ages 9–26
◦ Cervarix protects against only the types of HPV that cause cervical cancer
▪ Approved for use solely in female patients ages 9–25
Chlamydia Trachomatis
• an intracellular bacterium & causative agent of genital chlamydia infections
◦ It invades the epithelial tissues in the reproductive tract.
◦ Incubation is 1 to 3 weeks but the pathogens may be presents for months without producing
symptoms.
◦ Chlamydia is a reportable condition to health departments in all states.
◦ 20 – 40% of women who become infected with chlamydia develop Pelvic Inflammatory Disease
(PID)
• Often asymptomatic but some signs and symptoms may include:
◦ *Vaginal or Urethral discharge
◦ *Dysuria (painful urination)
◦ *Frequent Urination
◦ *Pelvic pain
[Show More]



_removed.png)