HESI Foundations Review. Ultimate Study Guide. Grade A+. All the Best
Document Content and Description Below
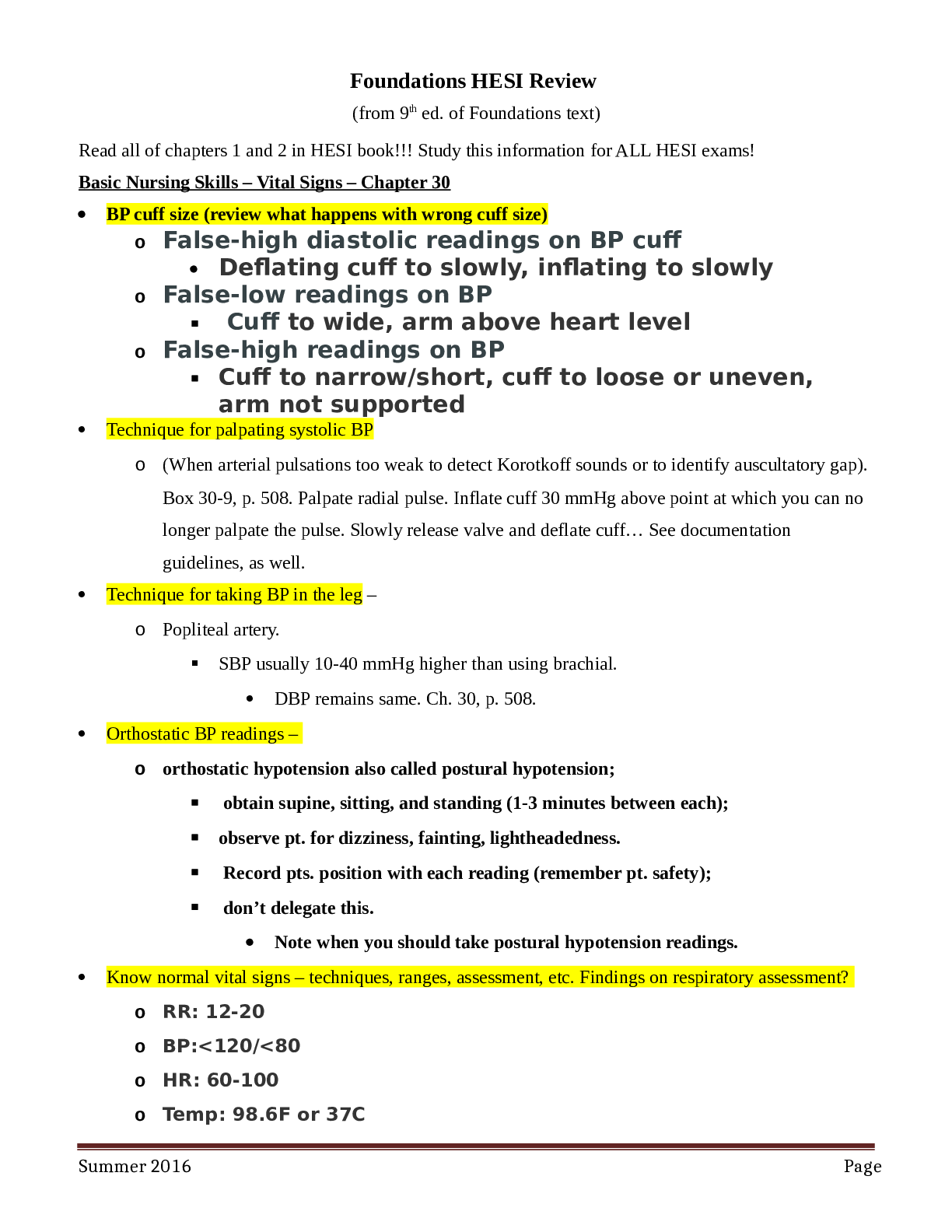
HESI Foundations Review (From 9th Edition of Foundations) Ultimate study guide for ALL HESI Exams. Good Luck!! Basic Nursing Skills – Vital Signs – Chapter 30 • BP cuff size (review what hap ... pens with wrong cuff size) False-high diastolic readings on BP cuff Deflating cuff to slowly, inflating to slowly False-low readings on BP Cuff to wide, arm above heart level False-high readings on BP Cuff to narrow/short, cuff to loose or uneven, arm not supported Technique for palpating systolic BP (When arterial pulsations too weak to detect Korotkoff sounds or to identify auscultatory gap). Box 30-9, p. 508. Palpate radial pulse. Inflate cuff 30 mmHg above point at which you can no longer palpate the pulse. Slowly release valve and deflate cuff… See documentation guidelines, as well. Technique for taking BP in the leg – Popliteal artery. ▪ SBP usually 10-40 mmHg higher than using brachial. • DBP remains same. Ch. 30, p. 508. Orthostatic BP readings – orthostatic hypotension also called postural hypotension; • obtain supine, sitting, and standing (1-3 minutes between each); • observe pt. for dizziness, fainting, lightheadedness. • Record pts. position with each reading (remember pt. safety); • don’t delegate this. • Note when you should take postural hypotension readings. Know normal vital signs – techniques, ranges, assessment, etc. Findings on respiratory assessment? o RR: 12-20 o BP:<120/<80 o HR: 60-100 o Temp: 98.6F or 37C o Pain 5th vital sign Vital Signs – Guidelines • Nurse ultimately responsible for vitals but can be delegated in stable patients, • RN to interpret their significance and make decision about interventions; • Determine equipment functional and appropriate; o Know pt normal vitals; • Know history, therapies and meds that could affect vitals; • Control environmental factor that could affect vitals; o Be organized and use systematic approach to ensure accuracy; o Use vitals to determine indications for med administration; • Analyze measurements; communicate changes to HCP; • Advise pt and or pt family of results. What is a pulse deficit? What do you do if you detect a pulse deficit during your assessment? See Clinical Decision (If pulse is irregular do an apical/radical pulse assessment to detect a pulse deficit. Count apical pulse help patient to supine position or sitting position move aside bed linen and gown to expose sternum and let side of chest. While a colleague counts radial pulse begin apical pulse count out load to simultaneously assess pulses. If pulse differs by more than 2 a pulse deficit exists which sometimes indicates alternation in cardiac output.). What if pulse deficit is in lower extremities? Pedal pulse weak on one side? ▪ Assess next pulse up, e.g., posterior tibial. ▪ If that pulse is weak, move up to popliteal, etc. ▪ Compare one extremity to the other. Apical pulse is taken for a full minute; PMI (point of maximal impulse) located at 4th or 5th intercostal space (ICS), just medial or left of the midclavicular line (MCL). Elevated BP? Pt c/o headache? What may this indicate? What do you do? Reassess using other arm. Do not keep taking BP on same extremity. Reassess May even need a manual cuff. Pain and Sleep [Show More]
Last updated: 3 years ago
Preview 1 out of 20 pages
Buy this document to get the full access instantly
Instant Download Access after purchase
Buy NowInstant download
We Accept:

Reviews( 0 )
$8.50
Can't find what you want? Try our AI powered Search
Document information
Connected school, study & course
About the document
Uploaded On
Apr 29, 2021
Number of pages
20
Written in
All
Additional information
This document has been written for:
Uploaded
Apr 29, 2021
Downloads
0
Views
98