Pathophysiology of Meningitis
Hematogenous spread
blood to subarachnoid
space
Mechanical disruption
Fracture of the base
of the skull
Direct extension from;
ear
mastoid air cells
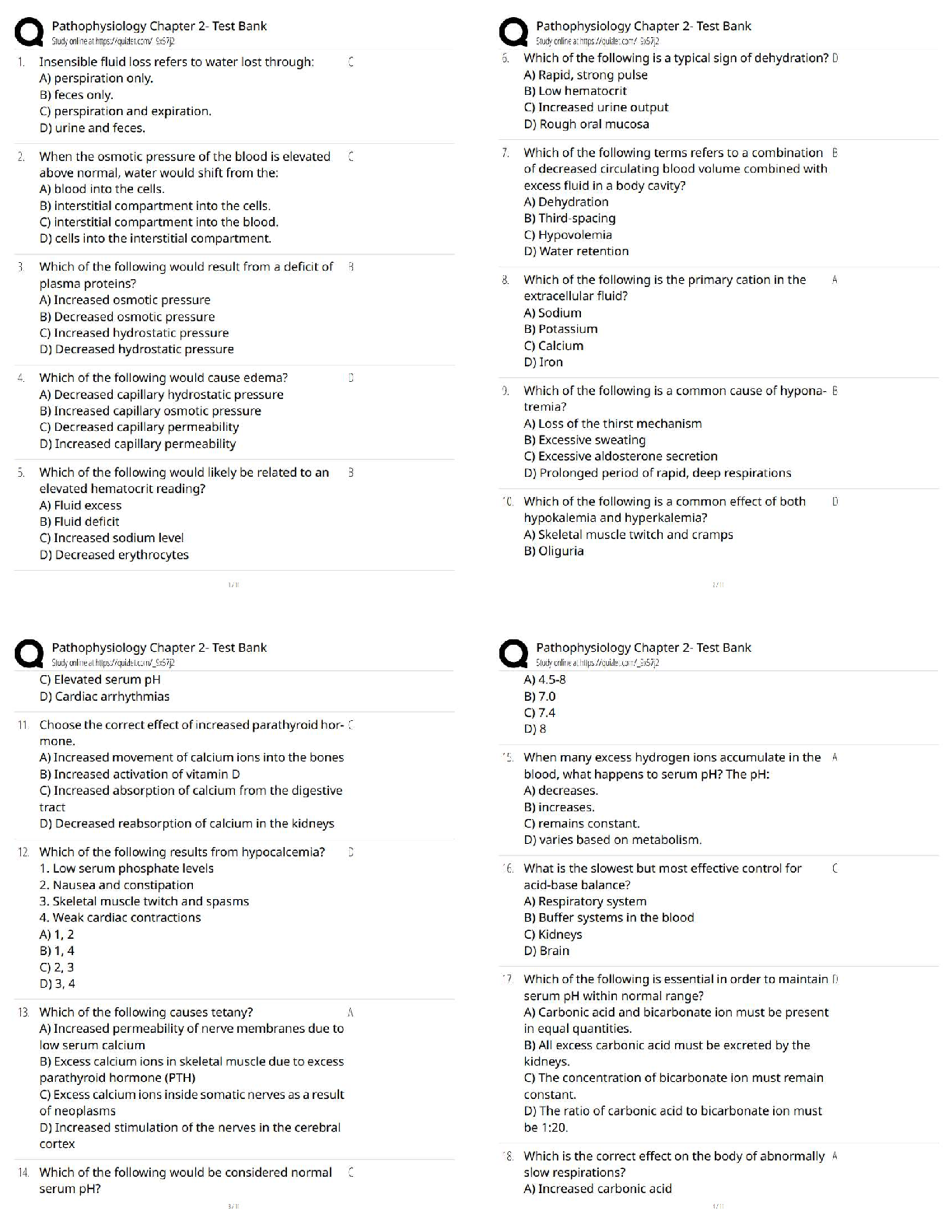
S/s of meningitis
Fever
A
...
Pathophysiology of Meningitis
Hematogenous spread
blood to subarachnoid
space
Mechanical disruption
Fracture of the base
of the skull
Direct extension from;
ear
mastoid air cells
S/s of meningitis
Fever
Altered consciousness
Irritability
Photophobia
Vomiting
Poor appetite
Seizure
Children with meningeal irritation often resist walking or being carried
Bulging fontanel
Stiff neck/nuchal rigidity
Meningismus
(stiff neck + Brudzinski + Kernig)
Absence does not rule out intracranial infection
00:02
01:26
Physical Exam of Meningitis
fever, tachypneic/irregular patterns, tachycardic/bradycardic
Integumentary
rashes
HEENT
Funduscopic exam - Papilledema
Neuro
2-12
Cerebellar
Meningeal specific testing
cushing's triad
Increased systolic BP, widened pulse pressure; bradycardia; irregular respirations- this is a late sign of ICP
Purpura Fulminans
What disease does N. Meningitis cause
Classic Triad for Meningitis
Fever, Headache and Stiff neck
With Fever what will have a corresponding rise
Heart rate usually 10 bpm for every degree of fever.
Age related confounding results
Young and Old have underdeveloped or weakened immune system may not present in classically way with a fever.
Nuchal Rigidity
Extreme stiffness of neck from inflamed meningeal membranes, meningitis.
- looks like they really don't want to move the neck
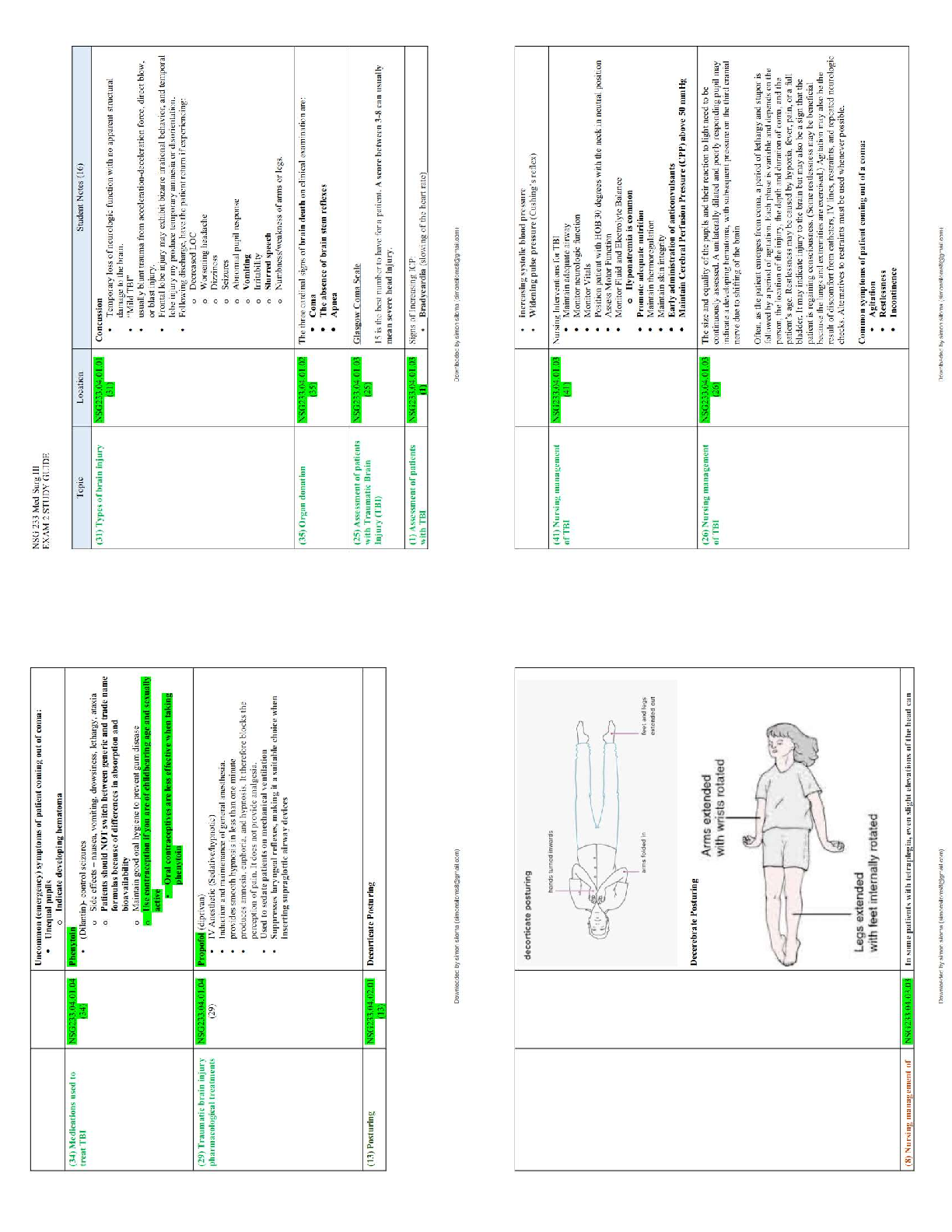
Brudzinski's sign
Sign of meningitis; positive when a patient's legs lift involuntarily when lifting a patient's head
Kernig sign
inability to fully extend the knees with hips flexed.
Key Difference btw Meningitis and Encephalitis
Encephalitis will have altered mental status.
DDx for Meningitis
-Encephalitis
-Influenza
-*Viral Syndrome- most lawsuits missed dx?
-Strep Pharyngitis
-Subarachnoid Hemorrhage- can develop a low grade temp, and stiff neck from the blood coagulation.
-Epidural Abscess
-Brain Abscess
-Meningococcemia- college dorms and military barracks
Diagnostic testing for Meningitis
Complete Blood Count
Serum Electrolytes
Blood Glucose
Renal Functions
Blood Culture
UA/Urine culture
LP:
Cytology
WBC
Protein
Glucose glucose will decreased in the CSF fluid
RBC
Gram Stain
Cultures
Viral
Bacterial
Fungal
other
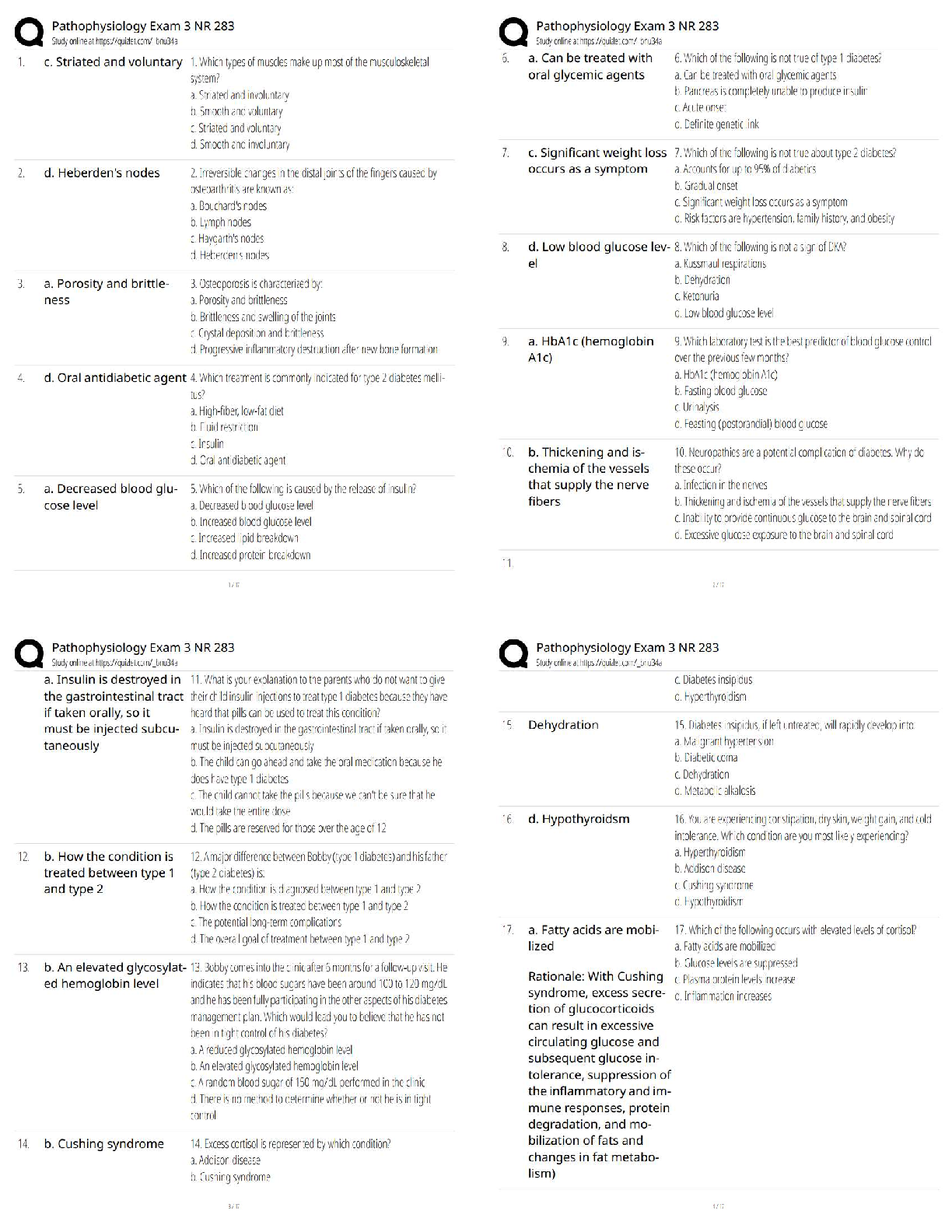
Differentials for different types of meningeal infections
CSF fluid analysis
Haemophilus INfluenza gram stain
Gram Neg CoccoBacill
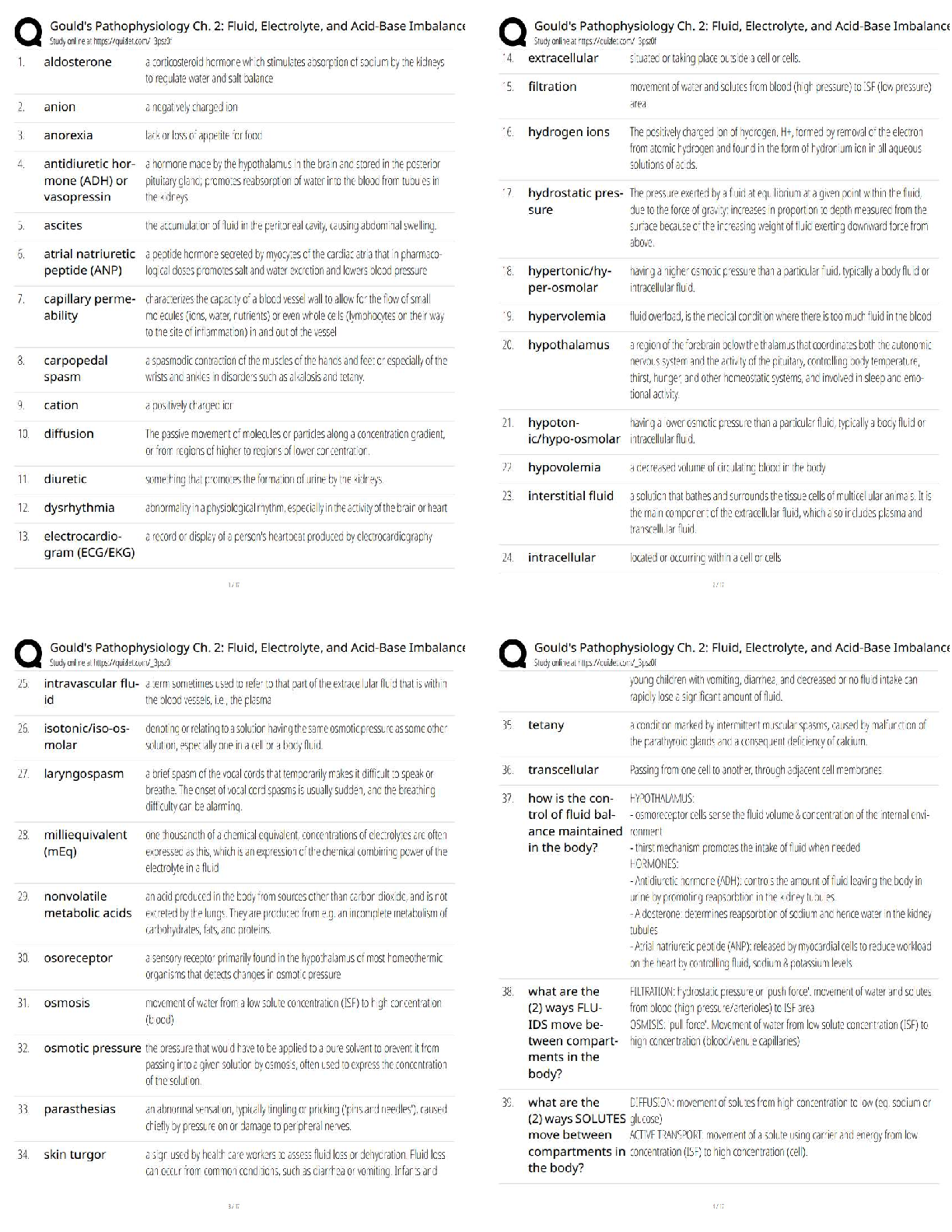
Treatment of Meningitis neonates
Ampicillin (covers Listeria), 100 mg/kg
AND
Cephalosporin active against gram negative bacilli may be used instead of an aminoglycoside because;
Much less toxic
No serum drug levels to follow
Not excreted in bile therefor not inhibit bowel flora
Cefotaxime, 50 mg/kg
or
Aminoglycoside
Gentamicin, 2.5 mg/kg (May cause heating loss-Ototoxicity)
Bacterial ABX with Infants and children
Ampicillin (covers Listeria), 100 mg/kg
AND
Cephalosporin active against gram negative bacilli may be used instead of an aminoglycoside because;
Much less toxic
No serum drug levels to follow
Not excreted in bile therefor not inhibit bowel flora
Cefotaxime, 50 mg/kg
or
Aminoglycoside
Gentamicin, 2.5 mg/kg (May cause heating loss-Ototoxicity)
Pneumococcal infection? Meningitis
Penicillin and cephalosporin resistance is possible
Vancomycin is the only antibiotic to which all strains of pneumococci are susceptible
Add Vancomycin, 15 mg/kg
Additional Corticosteroid tx with meningitis
Dexamethasone, 0.15 mg/kg IV administered prior to or along with the initial antibiotics has been shown to decrease ICP, cerebral edema & CSF lactate.
Treatment durations
Neonates: 14 - 21 days
Gram negative meningitis: 21 days
Pneumococcal, H flu: 10 days
Meningococcal: 7 days
Viral Meningitis
Summer, fall
Severe headache
Vomiting
Fever
Stiff neck
CSF results;
pleocytosis (monos), Normal protein, Normal glucose
Enteroviruses: most common - Oral fecal rout
Less common- Mumps, HIV and HSV-2
tx: Antiviral Rx-IV acyclovir
No antibiotics
Analgesia
Fever control
Often feel better after LP
Meningitis
Inflammation of the leptomeninges caused by infectious or noninfectious processes.
Infectious Causes = Bacterial, Viral, Tuberculous and Fungal
Acute Bacterial; Aseptic; and Subacute to chronic
Most common noninfectious causes are:
Subarachnoid hemorrhage, Cancer, and Sarcoidosis
Know Bacterial Presentation in different age groups
What is the most common age of patient presenting with bacterial meningitis
75% are under 15 years of age.
Neisseria meningitidis
( Gram negative Cocci) Adult bacterial meningitis commonly know as meningococcal meningitis. Humans are the natual host and bacteria remain int he upper respiratory tract of asymptomatic carriers. Droplet infection.Bacteria reaches the meninges via blood. Outbreaks are occur in area where large populations live together such as military barracks and in college dorms.Diagnosis: Gram negative cocci seen in CSF. Prevention: MENINGOCOCCAL VACCINE currently given to military personnel and dorm college students.
Haemophilus influenzae
an upper respiratory infection that does not cause influenza, but does affect the epiglottis. worst case scenario, it can cause an inflammation of the covering of the brain. type B causes most infections, a HIB vaccine is now available to be given at 3 mo of age. children are most succeptible to this virus when they are between 6 months and 5 years old.
Pneumococcal meningitis
Streptococcus pneumoniae most common cause of meningitis in adults, and the second most common cause of meningitis in children older than 6 years old, G(+)diplococci or in chains.Alpha Hemolytic. Optochin sensitive. Increased pressure in skull and spinal cord from swelling. Vaccine: Pneumovax (Adults) and Prevnar (Children)
becoming increasing resistant to penicillin
Frequency of bacterial meningitis
**Pneumococal = 40-55%
Meningococcal = 3-13%
Listerial = 10-13%
H. influenzae = 4-8%
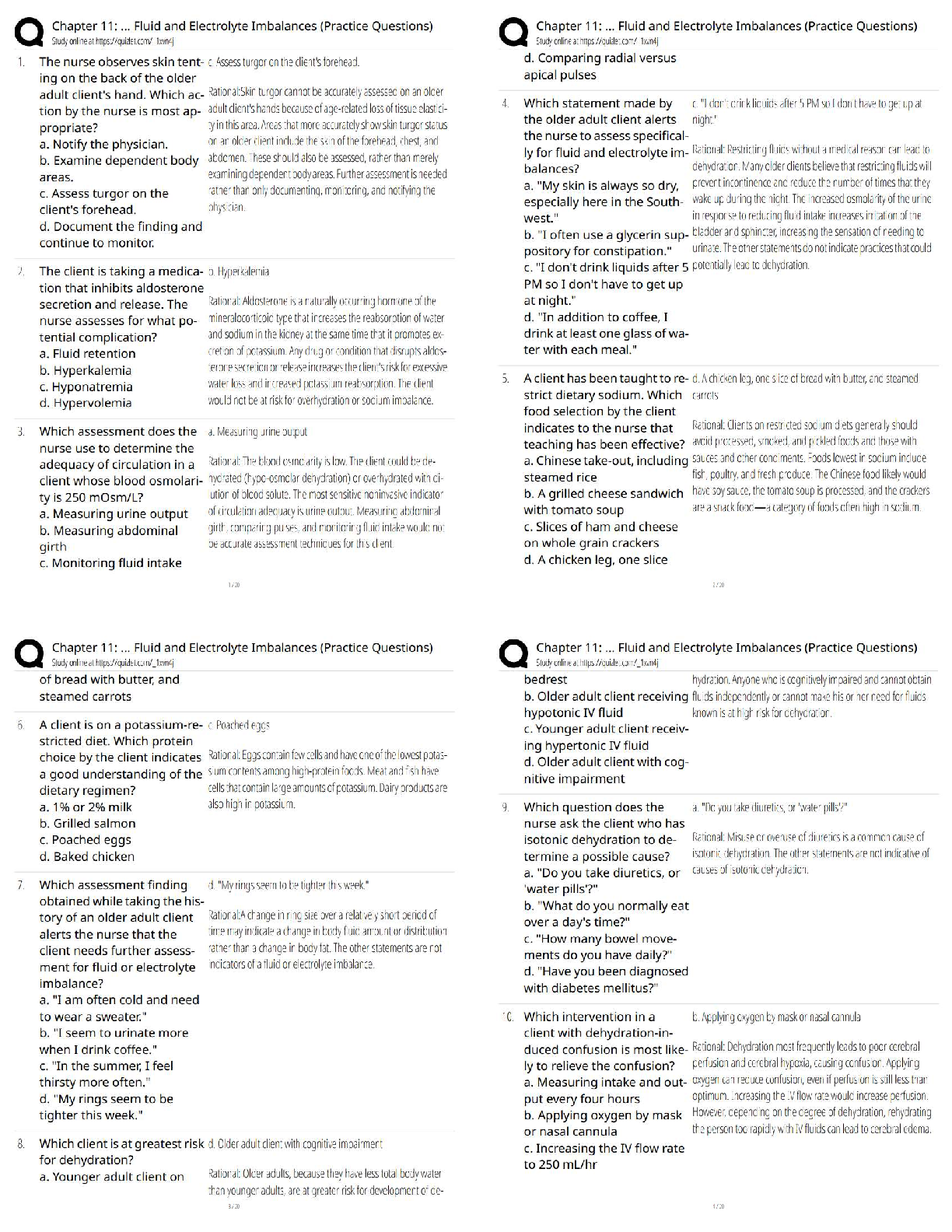
Pathology of Meningitis
Bacteria that cause most of the community-acquired meningitis transiently colonize the oro and nasopharynx of healthy individuals
Can occur after bacteremia from an upper respiratory site
Especially with N. meningitidis or H. influenzae)
Can occur from pneumonia or a sinus infection
Gram-negative bacterial meningitis occurs mainly in severely debilitated persons or those with damaged or breached meninges
Head trauma, neurosurgery, tumor
Clinical presentation: Meningitis
Bacterial: fever, confusion, headache, irritabilit, lethargy, and stiff neck
3 modes of onset:
-fulminant (high mortality)
-meningeal symptoms- 1-7 days
-May superimpose itself
*not always with stiff neck
*will have petechial or pupuric rash
*may have seizures
*may have focal neurological findings
Definitive test for Dx: Meningitis
evaluation of cerebrospinal fluid by lumbar puncture
-Have a low threshold for performing procedure in right clinical setting
-*For those patients with a high clinical suspicion, a lumbar puncture should be performed as soon as possible
In a situation where a patient is critical, empiric antibiotics should be administered as soon as possible.
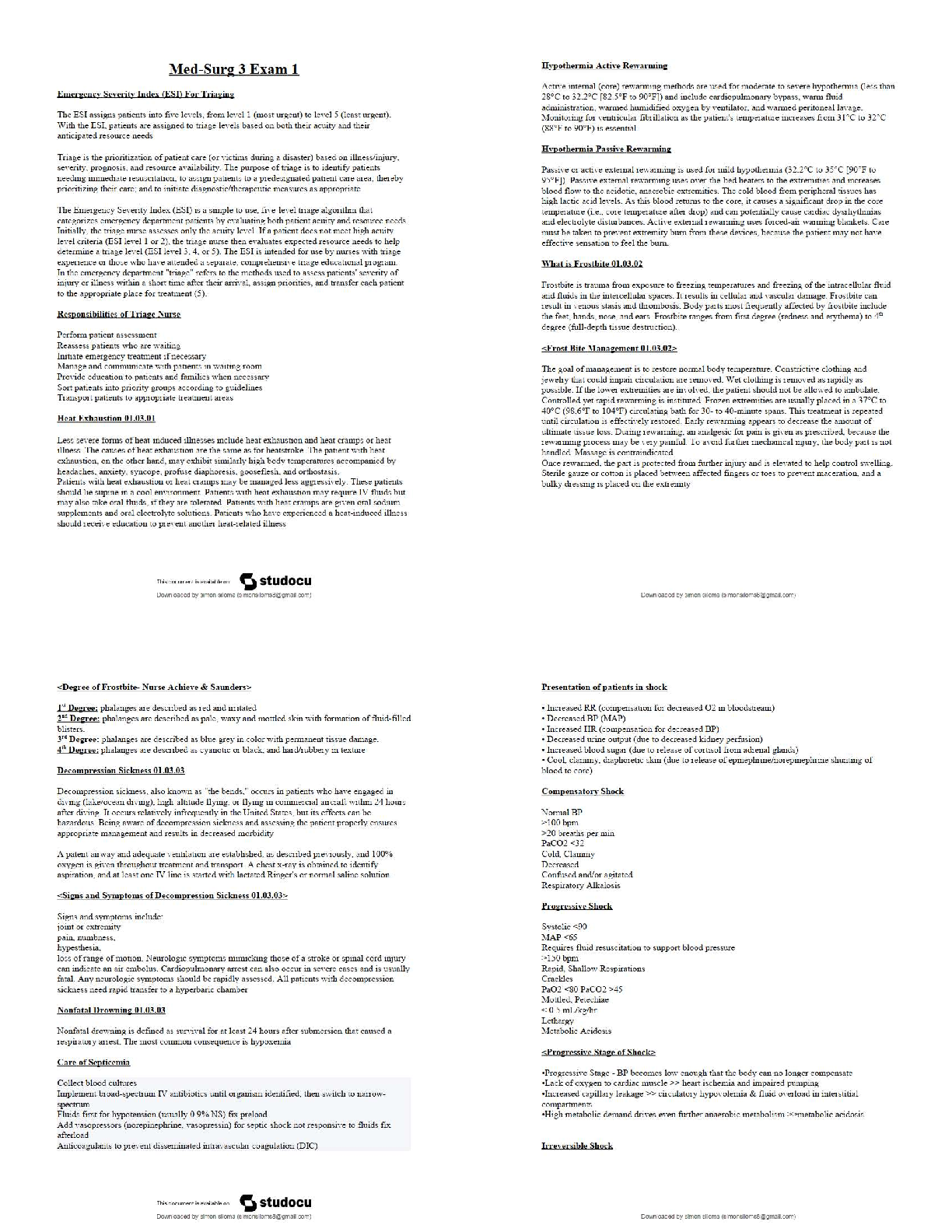
Normal Lumbar Puncture Ranges
Opening Press: 5-18 cm H2O in lateral neutral position;
Color: clear and colorless
Total Protein: 15-45 mg/100 ml
Glucose: 50-80 mg/100 ml or 2/3 serum glucose
WBC: 0-5 per HPF
RBC: 0 per HPF
Bacterial Antigens: Negative
Gram Stain: No WBCs or Organisms seen
Management of Increased Intracranial Pressure
Recognition: worsening mental status, papilledema, bulging fontanelle, widening of cranial sutures
Treatment
Elevate head of bed to 300
Controlled ventilation to keep end tidal PCO2 between 30 and 35 mmHg
Mannitol, 0.25 - 1 g/kg
Furosemide, 1 mg/kg
Aseptic Meningitis
meningitis that is associated with:
Negative gram stain and negative bacterial cultures
Viral infections are the most frequent cause of aseptic meningitis
-enteroviruses
-HSV
-Leptospira
Medication have also be implicated -
NSAIDs (Ibuprofen), Antimicrobials (Cipro/Bactrim), Ranitidine
S/S
Similar to that of bacterial meningitis with fever, headache, neck stiffness
With development of neurologic changes or findings the diagnosis shifts to encephalitis or meningoencephalitis
Diagnosis
Like bacterial meningitis, mainstay of diagnosis is lumbar puncture
Subacute / Chronic Meningitis
- A clinical syndrome that develops over a course of several weeks, clinically takes the form of meningitis or meningoencephalitis and is associated with a predominantly mononuclear pleocytosis in the CSF.
-usually immunosuppressed:
HIV, Mycobacterium tub, Cryptococcus neoformans
Dx: Clinical history
India ink preparation = Cryptococcus
VDRL = Syphillis
Borrelia burgdorferi = Lyme disease
Histoplasma antigen
Acute Bacterial Meningitis Tx:
1. Ceftriaxone 2gm IVPB and Vancomycin 1gm IVPB
-If there is a severe-PCN allergy than use Meropenem instead of Ceftriaxone
-Cefotaxime is the preferred alternate to Ceftriaxone for neonates under 4 weeks of age (Kernicterus)
2. Dexamethasone 10mg IVP should be given with the first dose of antibiotics to help decrease morbidity and mortality.
3.Ampicillin is good for Listeria monocytogenes infections as well as Group B streptococcus and Enterococcus
4. Ceftazidime is good for suspected Pseudomonas infections
Aseptic Meningitis
typically a self-limited disease which does not require a specific treatment or medication
Unless Herpes simplex virus is implicated with primary genital herpes infection. Then Acyclovir should be used
Subacute and Chronic Meningitis:
more than 50-100 cells/mcL than an infectious disease is likely and antimicrobial therapy should be started
If the pleocytosis is low-grade (less than 50 cells/mcL) than a non-infectious cause is likely and care is usually supportive or symptomatic
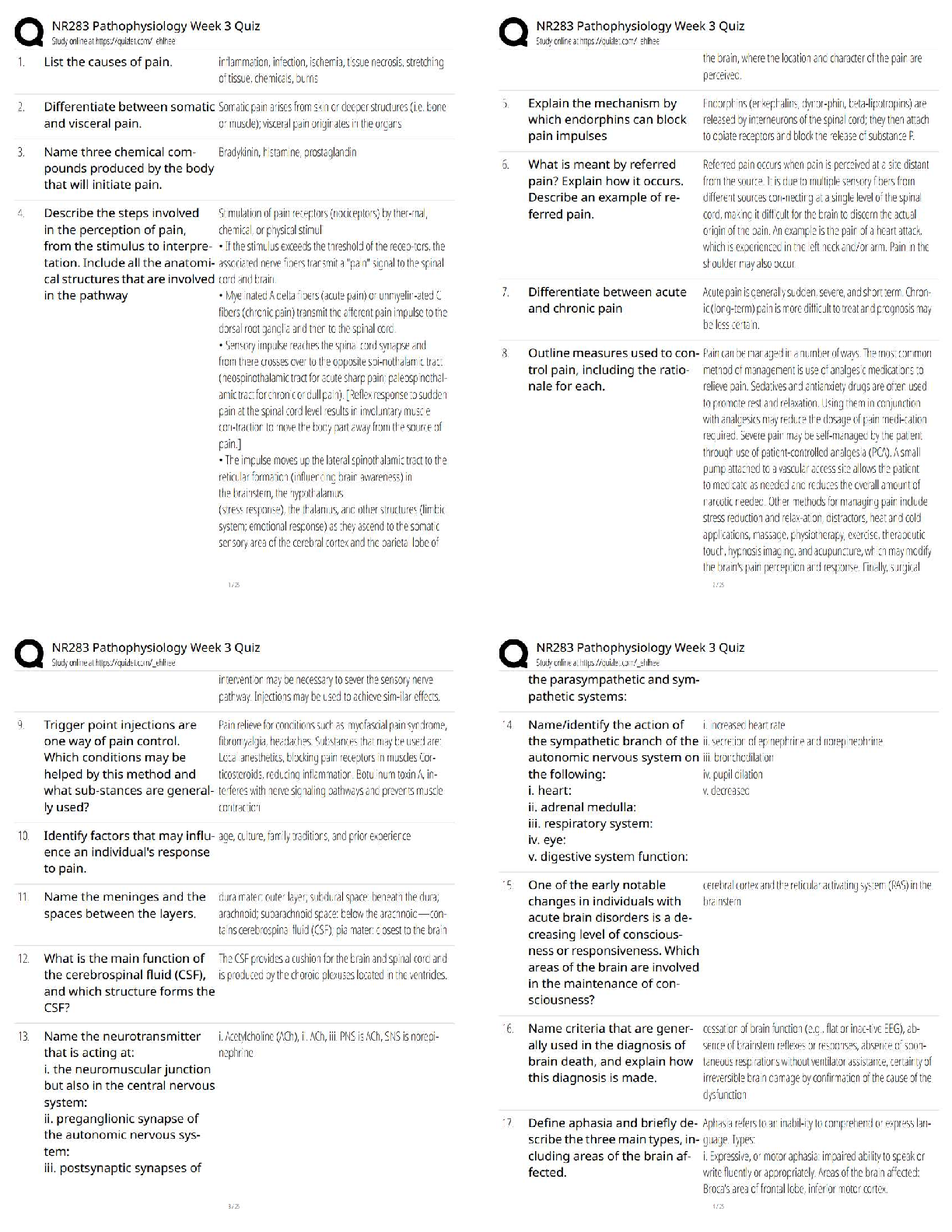
Encephalitis
Acute inflammatory process of the brain tissue. Causes include viral infections, vector -borne viral infections, and fungal infections.
Etiology of Encephalitis
Arthropod-borne viruses peak in summer and fall (West Nile, LaCrosse)
Western equine peaks in August and St. Louis encephalitis after that
Tick-borne infections (Rocky Mountain spotted fever) in early summer
Enterovirus infections in late summer and fall
Mumps virus in winter and spring
Herpes simplex virus is the most frequent, treatable and devastating cause of sporadic, severe focal encephalitis. - Usually 1-7 days of prodrome.
Implicated in 10% of all encephalitis cases in North America
Dx of Encephalitis
Lumbar puncture will help establish definitive diagnosis
Order a HSV DNA by Polymerase chain reaction
TX of Encephalitis
Timely treatment with IV Acyclovir is essential
Very little downside to starting treatment versus side effects
Untreated - mortality is approximately 70%
[Show More]