1. Coumadin use, precautions, side effects, and labs
Oral anticoagulants inhibit hepatic synthesis of vitamin K. Warfarin is used mainly to prevent thromboembolic conditions such as thrombophlebitis, pulmonary emb
...
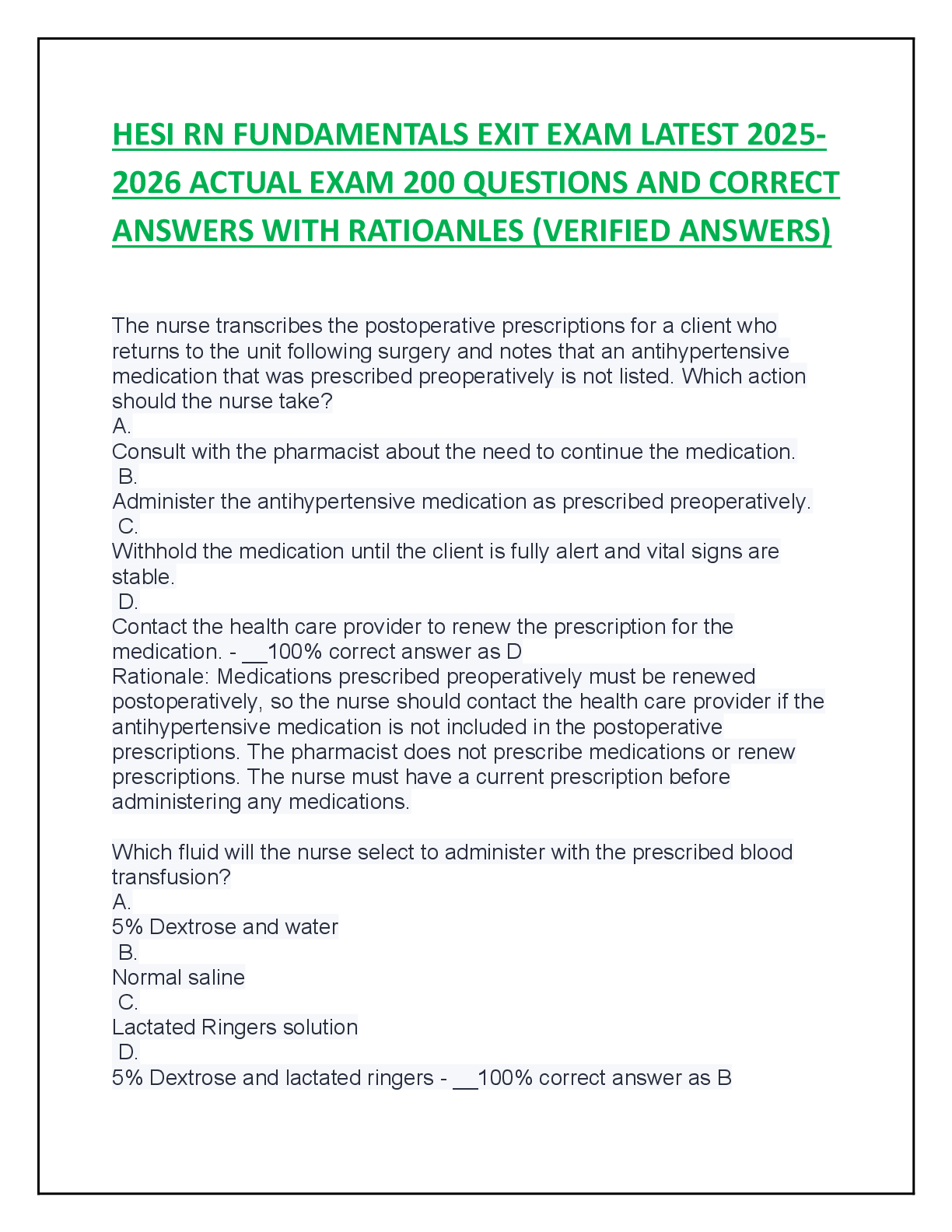
1. Coumadin use, precautions, side effects, and labs
Oral anticoagulants inhibit hepatic synthesis of vitamin K. Warfarin is used mainly to prevent thromboembolic conditions such as thrombophlebitis, pulmonary embolism, and embolism formation caused by atrial fibrillation, which can lead to stroke (CVA). Oral anticoagulants prolong clotting time and are monitored by the prothrombin time (PT), a laboratory test that measures the time it takes blood to clot in the presence of certain clotting factors. This laboratory test is usually performed immediately before administering the next drug dose until the therapeutic level has been reached. Today, international normalized ratio (INR) is the laboratory test most frequently used to report PT results. Normal INR is 1.3 to 2. Patients on warfarin therapy are maintained at an INR of 2 to 3. The desired INR for patients who have a mechanical heart valve or recurrent systemic embolism is 2.5 to 3.5, but the desired level could be as high as 4.5.
Monitoring INR at regular intervals is required for the duration of drug therapy. Drug accumulation can occur and lead to external or internal bleeding, so the nurse must observe for petechiae, ecchymosis, tarry stools, and hematemesis and teach the patient to do the same at home.
The antidote for warfarin overdose is Vitamin K, but it takes 24 to 48 hours to be effective. Usually a low dose of oral Vitamin K may be recommended for patients with an INR of 5.5. If excessive Vitamin K is given, it may take warfarin 1 to 2 weeks before it can be effective again. For acute bleeding, fresh frozen plasma is indicated.
Contraindications Drug-Lab-Food Interactions
Bleeding disorder, peptic ulcer, severe hepatic or renal disease, hemophilia
Blood dyscrasias, eclampsia, alcoholism, bleeding, head trauma
Caution: diabetes mellitus, leukemia
Pharmacodynamics
The PT level should be 1.5 to 2 times the reference value to be therapeutic, or INR should be 2.0 to 3.0. Higher INR levels (up to 3.5) are usually required for patients with prosthetic heart valves, cardiac valvular disease, and recurrent emboli. Heparin does not cross the placental barrier, unlike warfarin.
Side Effects and Adverse Reactions.
Bleeding (hemorrhage) is the major adverse effect of warfarin. Patients should be monitored closely for signs of bleeding (e.g., petechiae, ecchymosis, hematemesis).
Anticoagulant Antagonists
Bleeding occurs in about 10% of patients taking oral anticoagulants. Vitamin K1 (phytonadione), an antagonist of warfarin, is used for warfarin overdose or uncontrollable bleeding. Usually 1 to 10 mg of vitamin K1 is given at once, and if it fails to control bleeding, then fresh whole blood or fresh-frozen plasma or platelets are generally given.
Patient Teaching
General
• Aspirin should not be taken with warfarin, because aspirin intensifies its action and bleeding is apt to occur. Suggest that patient use acetaminophen.
•Teach patient to control external hemorrhage (bleeding) from accidents or injuries by applying firm, direct pressure for at least 5 to 10 minutes with a clean, dry, absorbent material.
Question:
1. A patient is being changed from an injectable anticoagulant to an oral anticoagulant. Which anticoagulant does the nurse realize is administered orally?
• a.enoxaparin sodium (Lovenox)
• b.warfarin (Coumadin)
• c.bivalirudin (Angiomax)
• d.lepirudin (Refludan)
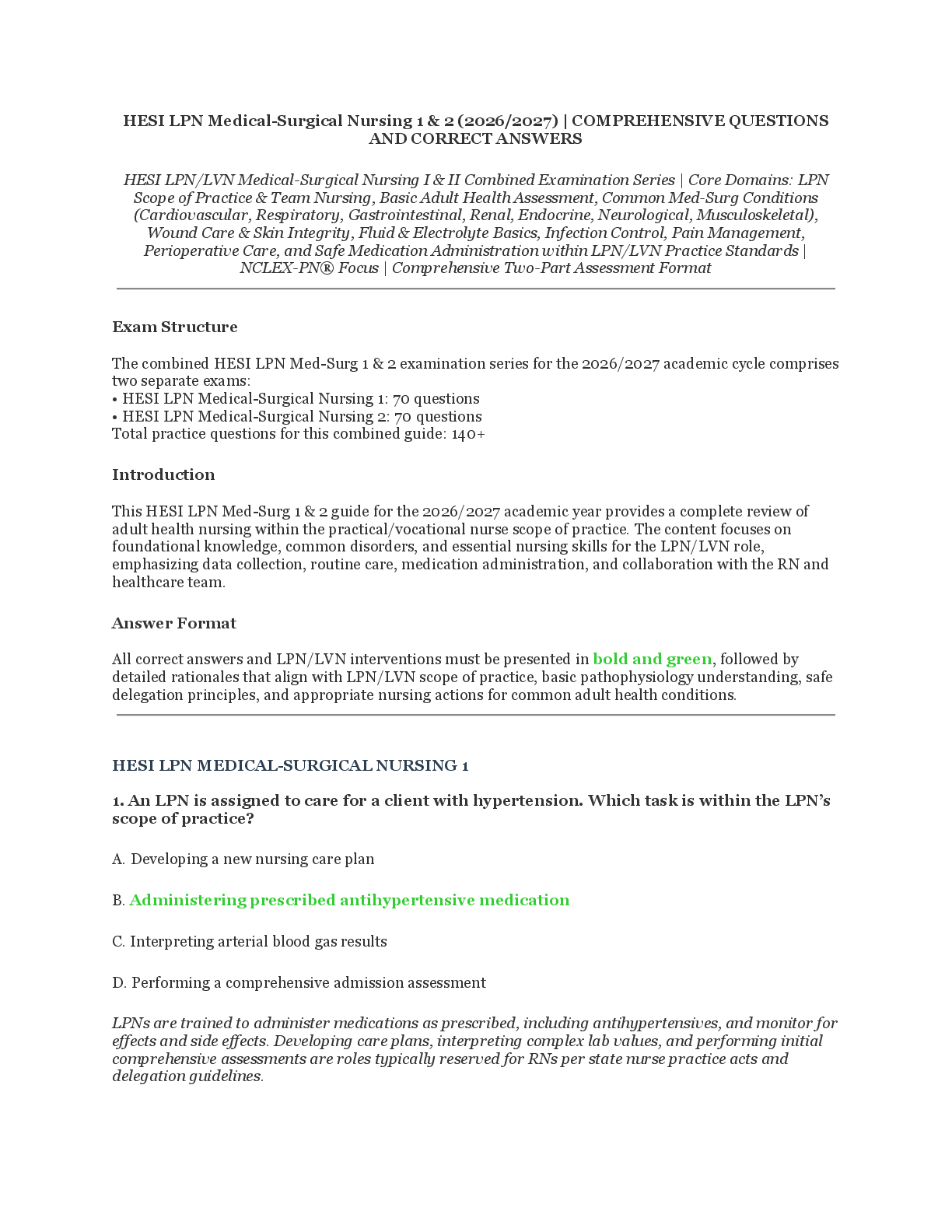
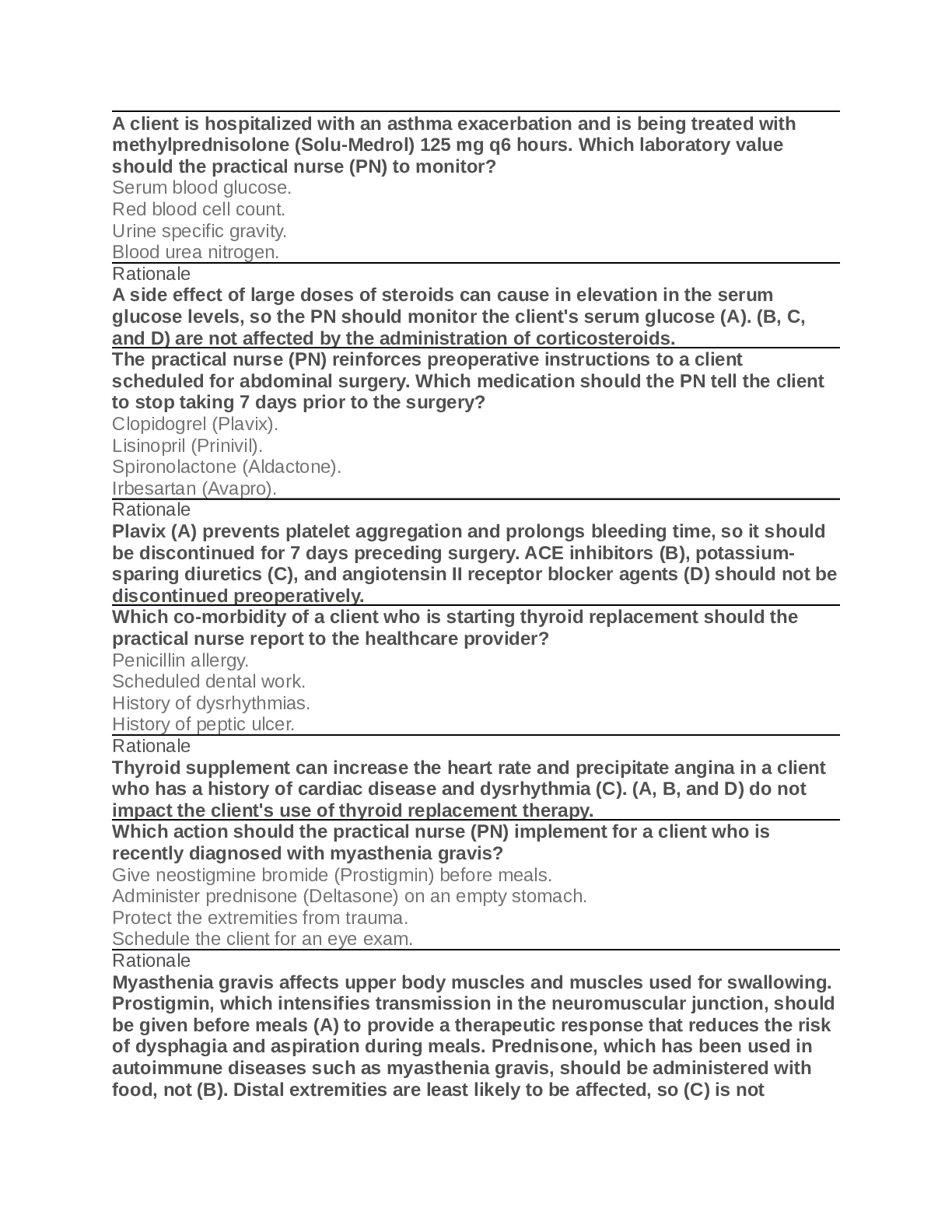
2. Steroid use, dc procedure
Glucocorticoids (Steroids): end in –sone or -lone
Glucocorticoids are used to treat respiratory disorders (COPD, etc.), particularly asthma. These drugs have an antiinflammatory action and are indicated if asthma is unresponsive to bronchodilator therapy or if the patient has an asthmatic attack while on maximum doses of theophylline or an adrenergic drug.
Inhaled glucocorticoids are not helpful in treating a severe asthmatic attack, because it may take 1 to 4 weeks for an inhaled steroid to reach its full effect. The use of an oral inhaler minimizes the risk for adrenal suppression associated with oral systemic glucocorticoid therapy. Inhaled glucocorticoids are preferred over oral preparations unless they fail to control the asthma.
Patients with acute asthma exacerbations are usually given systemic glucocorticoids (i.e., IV) for rapid effectiveness in large doses (20 to 40 mg prednisone for 5 days; 1 to 2 mg/kg/day for children for 3 to 5 days). An additional week with a reduced dose may be needed. With a single dose or short-term use, glucocorticoids may be discontinued abruptly after symptoms are controlled.
When severe asthma requires prolonged glucocorticoid therapy, weaning or tapering of the dose may be necessary to prevent an exacerbation of asthma symptoms and suppression of adrenal function. Previously, alternate-day therapy (ADT) with oral prednisone was used in some asthmatic patients.
Side Effects and Adverse Reactions.
When drug therapy is discontinued, the dose should be tapered to allow the adrenal cortex to produce cortisol and other corticosteroids. Abrupt withdrawal of the drug can result in severe adrenocortical insufficiency.
Patient Teaching
General
• ▪ Caution patient not to abruptly stop drug. When drug is discontinued, dose is tapered over 1 to 2 weeks.
• ▪ Prepare schedule for patient to decrease dose over 4 to 5 days. For short-term use (<10 days) of glucocorticoids such as prednisone or other cortisone preparations, drug dose still needs to be tapered. For example, day 1: 1 tab four times a day; day 2: 1 tab three times a day; day 3: 1 tab twice a day; day 4: 1 tab once a day.
• ▪ Teach patient to avoid persons with respiratory infections, because these drugs suppress immune system. This is especially important if patient is receiving high dose of glucocorticoids.
::::::::::::::::::::::::::::::::::::::::CONTENT CONTINUED IN THE ATTACHMENT:::::::::::::::::::::::::::::::::::::::::::::::::::
[Show More]


.png)

.png)