Chapter 24: The Child with Hematologic or Immunologic Dysfunction Hockenberry: Wong’s Essentials of Pediatric Nursing, 10th Edition
MULTIPLE CHOICE
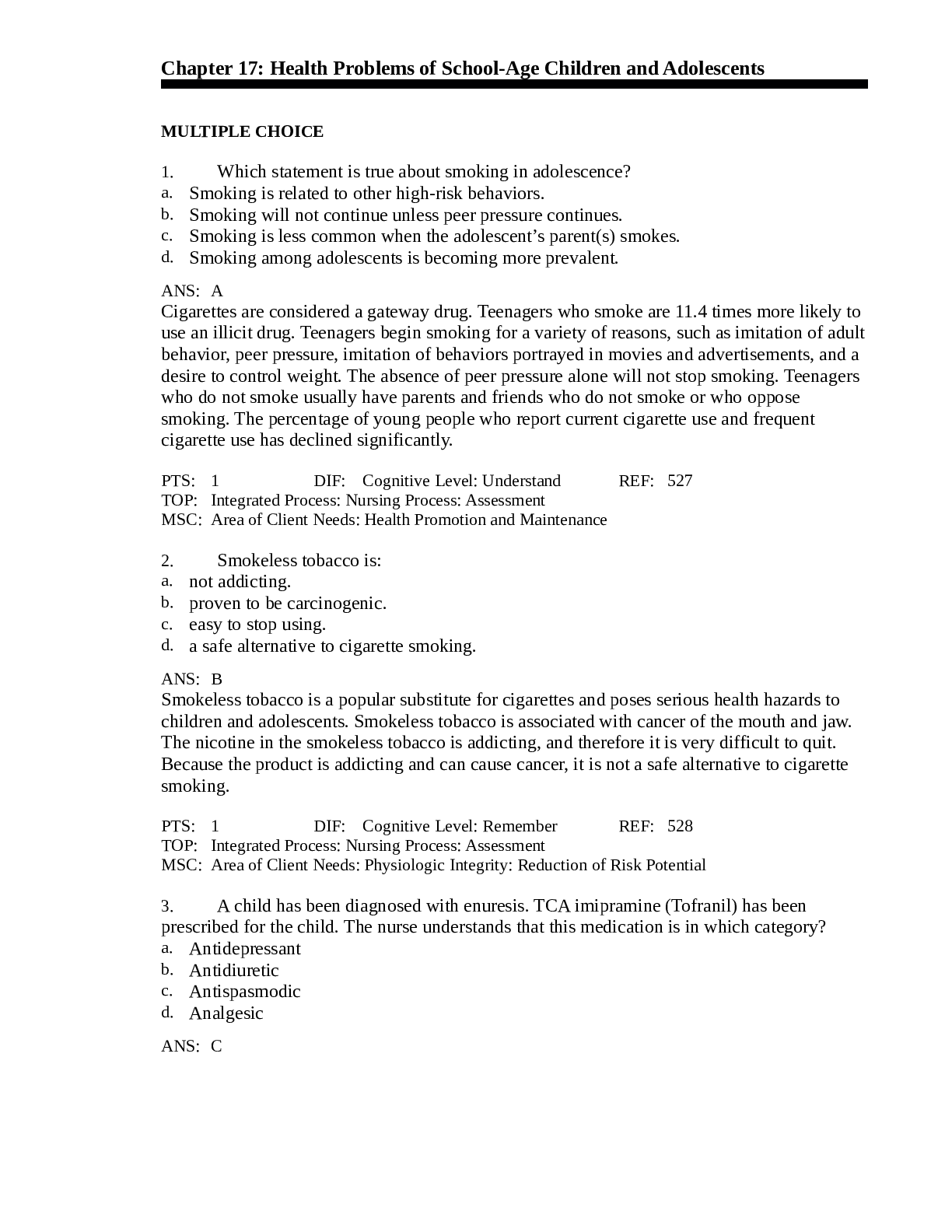
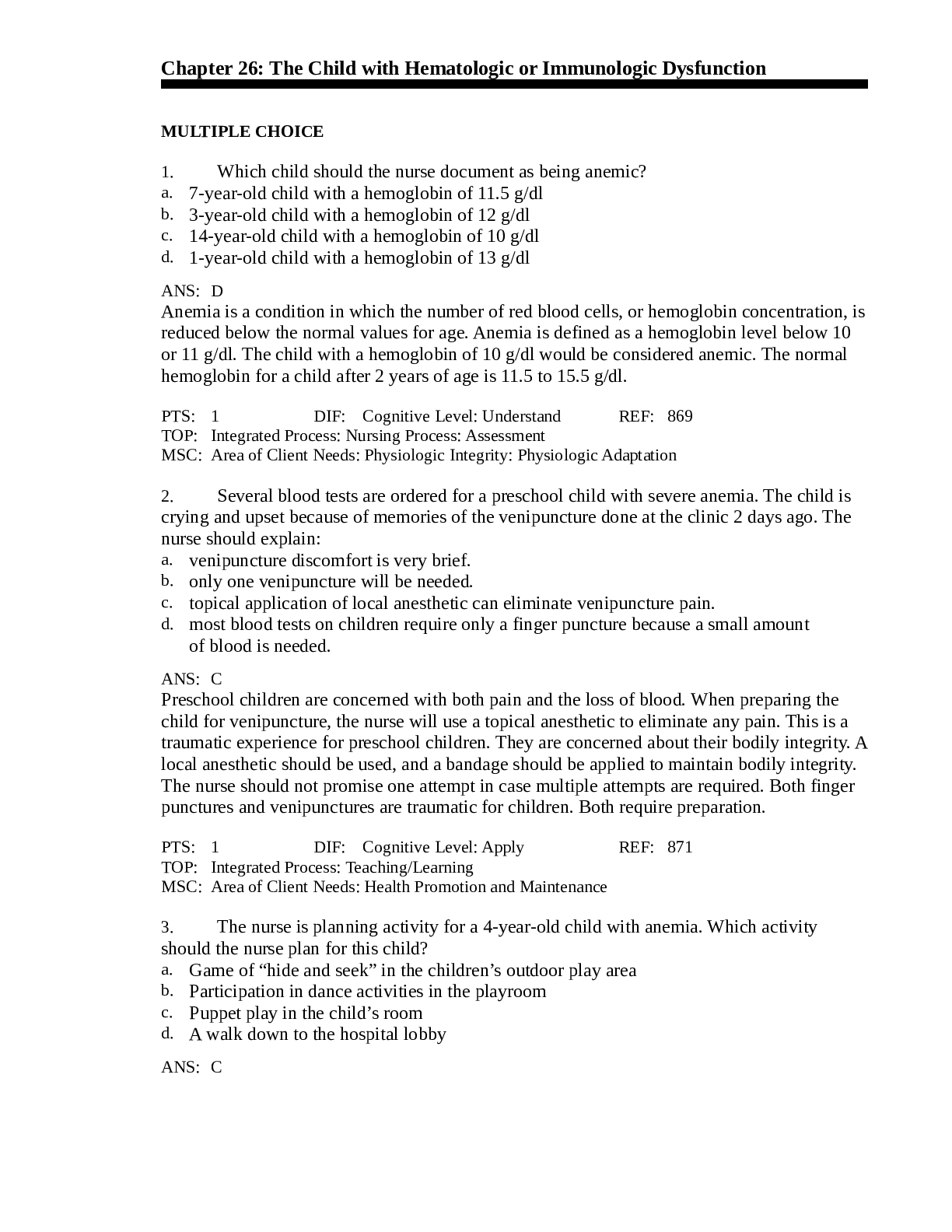
1. Which child should the nurse document as being anemic? a.
7-year-o
...
Chapter 24: The Child with Hematologic or Immunologic Dysfunction Hockenberry: Wong’s Essentials of Pediatric Nursing, 10th Edition
MULTIPLE CHOICE
1. Which child should the nurse document as being anemic? a.
7-year-old child with a hemoglobin of 11.5 g/dl
b. c. d.
3-year-old child with a hemoglobin of 12 g/dl 14-year-old child with a hemoglobin of 10 g/dl 1-year-old child with a hemoglobin of 13 g/dl
ANS: D Anemia is a condition in which the number of red blood cells, or hemoglobin concentration, is reduced below the normal values for age. Anemia is defined as a hemoglobin level below 10 or 11 g/dl. The child with a hemoglobin of 10 g/dl would be considered anemic. The normal hemoglobin for a child after 2 years of age is 11.5 to 15.5 g/dl.
DIF: Cognitive Level: Understand REF: p. 789
TOP: Integrated Process: Nursing Process: Assessment MSC: Area of Client Needs: Physiologic Integrity: Physiologic Adaptation
2. Several blood tests are ordered for a preschool child with severe anemia. The child is crying and upset because of memories of the venipuncture done at the clinic 2 days ago. What should the nurse explain?
a. The venipuncture discomfort is very brief b. Only one venipuncture will be needed
c. A topical application of local anesthetic can eliminate venipuncture pain
d. Most blood tests on children require only a finger puncture because a small amount of blood is needed
ANS: C Preschool children are concerned with both pain and the loss of blood. When preparing the child for venipuncture, the nurse will use a topical anesthetic to eliminate any pain. This is a traumatic experience for preschool children. They are concerned about their bodily integrity. A local anesthetic should be used, and a bandage should be applied to maintain bodily integrity. The nurse should not promise one attempt in case multiple attempts are required. Both finger punctures and venipunctures are traumatic for children. Both require preparation.
DIF: Cognitive Level: Apply REF: p. 789
TOP: Integrated Process: Teaching/Learning MSC: Area of Client Needs: Health Promotion and Maintenance
3. The nurse is planning activity for a 4-year-old child with anemia. Which activity should the nurse plan for this child?
a. Game of “hide and seek” in the children’s outdoor play area b. Participation in dance activities in the playroom Puppet play in the child’s room
c.
d. A walk down to the hospital lobby ANS: CBecause the basic pathologic process in anemia is a decrease in oxygen-carrying capacity, an
important nursing responsibility is to assess the child’s energy level and minimize excess
demands. The child’s level of tolerance for activities of daily living and play is assessed, and
adjustments are made to allow as much self-care as possible without undue exertion. Puppet
play in the child’s room would not be overly tiring. Hide and seek, dancing, and walking to
the lobby would not conserve the anemic child’s energy.
DIF: Cognitive Level: Apply
REF: p. 789
TOP: Integrated Process: Nursing Process: Implementation
MSC: Area of Client Needs: Physiologic Integrity: Physiologic Adaptation
4. The nurse is teaching parents about the importance of iron in a toddler’s diet. Which explains
why iron-deficiency anemia is common during toddlerhood?
a. Milk is a poor source of iron.
b.
Iron cannot be stored during fetal development.
c.
Fetal iron stores are depleted by age 1 month.
d. Dietary iron cannot be started until age 12 months.
ANS: A
Children between the ages of 12 and 36 months are at risk for anemia because cow’s milk is a
major component of their diet and it is a poor source of iron. Iron is stored during fetal
development, but the amount stored depends on maternal iron stores. Fetal iron stores are
usually depleted by age 5 to 6 months. Dietary iron can be introduced by breastfeeding, iron-
fortified formula, and cereals during the first 12 months of life.
DIF: Cognitive Level: Understand
REF: p. 789
TOP: Integrated Process: Teaching/Learning
MSC: Area of Client Needs: Physiologic Integrity: Physiologic Adaptation
5. The nurse is teaching parents of an infant about the causes of iron-deficiency anemia. Which
statement best describes iron-deficiency anemia in infants?
It is caused by depression of the hematopoietic system.
a.
b.
c.
d.
It is easily diagnosed because of an infant’s emaciated appearance.
Clinical manifestations are similar regardless of the cause of the anemia.
Clinical manifestations result from a decreased intake of milk and the preterm
addition of solid foods.
ANS: C
In iron-deficiency anemia, the child’s clinical appearance is a result of the anemia, not the
underlying cause. Usually the hematopoietic system is not depressed in iron-deficiency
anemia. The bone marrow produces red cells that are smaller and contain less hemoglobin
than normal red cells. Children who are iron deficient from drinking excessive quantities of
milk are usually pale and overweight. They are receiving sufficient calories, but are deficient
in essential nutrients. The clinical manifestations result from decreased intake of iron-fortified
solid foods and an excessive intake of milk.
DIF: Cognitive Level: Apply
REF: p. 789
TOP: Integrated Process: Teaching/Learning
MSC: Area of Client Needs: Physiologic Integrity: Physiologic Adaptation6. Which should the nurse include when teaching the mother of a 9-month-old infant about
administering liquid iron preparations?
a. They should be given with meals.
b. They should be stopped immediately if nausea and vomiting occur.
c. Adequate dosage will turn the stools a tarry green color.
d. Allow preparation to mix with saliva and bathe the teeth before swallowing.
ANS: C
The nurse should prepare the mother for the anticipated change in the child’s stools. If the iron
dose is adequate, the stools will become a tarry green color. The lack of the color change may
indicate insufficient iron. The iron should be given in two divided doses between meals when
the presence of free hydrochloric acid is greatest. Iron is absorbed best in an acidic
environment. Vomiting and diarrhea may occur with iron administration. If these occur, the
iron should be given with meals, and the dosage reduced, then gradually increased as the child
develops tolerance. Liquid preparations of iron stain the teeth. They should be administered
through a straw and the mouth rinsed after administration.
DIF: Cognitive Level: Apply
REF: p. 789
TOP: Integrated Process: Teaching/Learning
MSC: Area of Client Needs: Physiologic Integrity: Pharmacologic and Parenteral Therapies
7. Iron dextran is ordered for a young child with severe iron-deficiency anemia. What nursing
considerations should be included?
a. Administer with meals
b. Administer between meals
c.
Inject deeply into a large muscle
d. Massage injection site for 5 minutes after administration of drug
ANS: C
Iron dextran is a parenteral form of iron. When administered intramuscularly, it must be
injected into a large muscle. Iron dextran is for intramuscular or intravenous (IV)
administration. The site should not be massaged to prevent leakage, potential irritation, and
staining of the skin.
DIF: Cognitive Level: Apply
REF: p. 790
TOP: Integrated Process: Nursing Process: Implementation
MSC: Area of Client Needs: Physiologic Integrity: Pharmacologic and Parenteral Therapies
8. The nurse is recommending how to prevent iron-deficiency anemia in a healthy, term,
breastfed infant. Which should be suggested?
Iron (ferrous sulfate) drops after age 1 month
a.
b.
c.
d.
Iron-fortified commercial formula by age 4 to 6 months
Iron-fortified infant cereal by age 2 months
Iron-fortified infant cereal by age 4 to 6 months
ANS: D
Breast milk supplies inadequate iron for growth and development after age 5 months.
Supplementation is necessary at this time. The mother can supplement the breastfeeding with
iron-fortified infant cereal. Iron supplementation or the introduction of solid foods in a
breastfed baby is not indicated. Providing iron-fortified commercial formula by age 4 to 6
months should be done only if the mother is choosing to discontinue breastfeeding.DIF: Cognitive Level: Apply
REF: p. 789
TOP: Integrated Process: Teaching/Learning
MSC: Area of Client Needs: Physiologic Integrity: Basic Care and Comfort
9. Parents of a child with sickle cell anemia ask the nurse, “What happens to the hemoglobin in
sickle cell anemia?” Which statement by the nurse explains the disease process?
a. Normal adult hemoglobin is replaced by abnormal hemoglobin.
b. There is a lack of cellular hemoglobin being produced.
c. There is a deficiency in the production of globulin chains.
d. The size and depth of the hemoglobin are affected.
ANS: A
Sickle cell anemia is one of a group of diseases collectively called hemoglobinopathies, in
which normal adult hemoglobin is replaced by abnormal hemoglobin. Aplastic anemia is a
lack of cellular elements being produced. Thalassemia major refers to a variety of inherited
disorders characterized by deficiencies in production of certain globulin chains. Iron-
deficiency anemia affects the size, depth, and color of hemoglobin.
DIF: Cognitive Level: Apply
REF: p. 791
TOP: Integrated Process: Teaching/Learning
MSC: Area of Client Needs: Physiologic Integrity: Physiologic Adaptation
10. When both parents have sickle cell trait, which is the chance their children will have sickle
cell anemia?
a. 25%
b. 50%
c. 75%
d. 100%
ANS: A
Sickle cell anemia is inherited in an autosomal recessive pattern. If both parents have sickle
cell trait (one copy of the sickle cell gene), then for each pregnancy, a 25% chance exists that
their child will be affected with sickle cell disease. With each pregnancy, a 50% chance exists
that the child will have sickle cell trait. Percentages of 75% and 100% are too high for the
children of parents who have sickle cell trait.
DIF: Cognitive Level: Analyze
REF: p. 791
TOP: Integrated Process: Nursing Process: Assessment
MSC: Area of Client Needs: Physiologic Integrity: Reduction of Risk Potential
11. The nurse is conducting a staff in-service on sickle cell anemia. Which describes the
pathologic changes of sickle cell anemia?
Sickle-shaped cells carry excess oxygen.
a.
b. Sickle-shaped cells decrease blood viscosity.
Increased red blood cell destruction occurs.
c.
d. Decreased adhesion of sickle-shaped cells occurs.
ANS: CThe clinical features of sickle cell anemia are primarily the result of increased red blood cell
destruction and obstruction caused by the sickle-shaped red blood cells. Sickled red cells have
decreased oxygen-carrying capacity and transform into the sickle shape in conditions of low
oxygen tension. When the sickle cells change shape, they increase the viscosity in the area
where they are involved in the microcirculation. Increased adhesion and entanglement of cells
occurs.
DIF: Cognitive Level: Apply
REF: p. 791
TOP: Integrated Process: Teaching/Learning
MSC: Area of Client Needs: Physiologic Integrity: Physiologic Adaptation
12. Which clinical manifestation should the nurse expect when a child with sickle cell anemia
experiences an acute vasoocclusive crisis?
Circulatory collapse
a.
b. Cardiomegaly, systolic murmurs
c. Hepatomegaly, intrahepatic cholestasis
d. Painful swelling of hands and feet; painful joints
ANS: D
A vasoocclusive crisis is characterized by severe pain in the area of involvement. If in the
extremities, painful swelling of the hands and feet is seen; if in the abdomen, severe pain
resembles that of acute surgical abdomen; and if in the head, stroke and visual disturbances
occur. Circulatory collapse results from sequestration crises. Cardiomegaly, systolic murmurs,
hepatomegaly, and intrahepatic cholestasis result from chronic vasoocclusive phenomena.
DIF: Cognitive Level: Understand
REF: p. 791
TOP: Integrated Process: Nursing Process: Assessment
MSC: Area of Client Needs: Physiologic Integrity: Physiologic Adaptation
13. Why is meperidine (Demerol) not recommended for children in sickle cell crisis?
a. May induce seizures
b.
Is easily addictive
c. Not adequate for pain relief
d. Given by intramuscular injection
ANS: A
A metabolite of meperidine, normeperidine, is a central nervous system stimulant that
produces anxiety, tremors, myoclonus, and generalized seizures when it accumulates with
repetitive dosing. Patients with sickle cell disease are particularly at risk for normeperidine-
induced seizures. Meperidine is no more addictive than other narcotic agents. Meperidine is
adequate for pain relief. It is available for IV infusion.
DIF: Cognitive Level: Understand
REF: p. 795
TOP: Integrated Process: Nursing Process: Planning
MSC: Area of Client Needs: Physiologic Integrity: Pharmacologic and Parenteral Therapies
14. A school-age child is admitted in vasoocclusive sickle cell crisis. What should be included in
the child’s care?
a.
Correction of acidosis
b. Adequate hydration and pain management
Pain management and administration of heparin
c.d. Adequate oxygenation and replacement of factor VIII
ANS: B The management of crises includes adequate hydration, minimization of energy expenditures, pain management, electrolyte replacement, and blood component therapy if indicated. Hydration and pain control are two of the major goals of therapy. The acidosis will be corrected as the crisis is treated. Heparin and factor VIII are not indicated in the treatment of vasoocclusive sickle cell crisis. Oxygen may prevent further sickling, but it is not effective in reversing sickling because it cannot reach the clogged blood vessels.
DIF: Cognitive Level: Apply REF: p. 796
TOP: Integrated Process: Nursing Process: Implementation MSC: Area of Client Needs: Physiologic Integrity: Physiologic Adaptation
[Show More]
.png)


.png)