. The child with seizure disorder is being treated with Dilantin
(phenytoin). Which of the following statements by the patient’s mother
indicates to the nurse that the patient is experiencing a side effect of Dilantin
...
. The child with seizure disorder is being treated with Dilantin
(phenytoin). Which of the following statements by the patient’s mother
indicates to the nurse that the patient is experiencing a side effect of Dilantin
therapy?
A. “She is very irritable lately.”
B. “She sleeps quite a bit of the time.”
C. “Her gums look too big for her teeth.”
D. “She has gained about 10 pounds in the last 6 months.”
2. A 5-year-old is admitted to the unit following a tonsillectomy. Which of
the following would indicate a complication of the surgery?
A. Decreased appetite
B. A low-grade fever
C. Chest congestion
D. Constant swallowing
3. A 6-year-old with cerebral palsy functions at the level of an 18-monthold. Which finding would support that assessment?
A. She dresses herself.
B. She pulls a toy behind her.
C. She can build a tower of eight blocks.
D. She can copy a horizontal or vertical line.
4. Which information obtained from the mother of a child with cerebral
palsy most likely correlates to the diagnosis?
A. She was born at 42 weeks gestation.
B. She had meningitis when she was 6 months old.
C. She had physiologic jaundice after delivery.
D. She has frequent sore throats.
5. A 10-year-old is being treated for asthma. Before administering
Theodur, the nurse should check the:
A. Urinary output
B. Blood pressure
C. Pulse
D. Temperature
A. Discard the solution and order a new bag
B. Warm the solution
C. Continue the infusion and document the finding
D. Discontinue the medication
7. The client is diagnosed with multiple myoloma. The doctor has ordered
cyclophosphamide (Cytoxan). Which instruction should be given to the
client?
A. “Walk about a mile a day to prevent calcium loss.”
B. “Increase the fiber in your diet.”
C. “Report nausea to the doctor immediately.”
D. “Drink at least eight large glasses of water a day.”
8. The client is taking rifampin 600mg po daily to treat his tuberculosis.
Which action by the nurse indicates understanding of the medication?
A. Telling the client that the medication will need to be taken with juice
B. Telling the client that the medication will change the color of the urine
C. Telling the client to take the medication before going to bed at night
D. Telling the client to take the medication if night sweats occur
9. The client is taking prednisone 7.5mg po each morning to treat his
systemic lupus errythymatosis. Which statement best explains the reason for
taking the prednisone in the morning?
A. There is less chance of forgetting the medication if taken in the morning.
B. There will be less fluid retention if taken in the morning.
C. Prednisone is absorbed best with the breakfast meal.
D. Morning administration mimics the body’s natural secretion of
corticosteroid.
10. A 20-year-old female has a prescription for tetracycline. While teaching
the client how to take her medicine, the nurse learns that the client is also
taking Ortho-Novum oral contraceptive pills. Which instructions should be
included in the teaching plan?
A. The oral contraceptives will decrease the effectiveness of the tetracycline.
B. Nausea often results from taking oral contraceptives and antibiotics.
C. Toxicity can result when taking these two medications together.
D. Antibiotics can decrease the effectiveness of oral contraceptives, so the
client should use an alternate method of birth control.
11. A 60-year-old diabetic is taking glyburide (Diabeta) 1.25mg daily to
treat Type II diabetes mellitus. Which statement indicates the need for further
teaching?
A. “I will keep candy with me just in case my blood sugar drops.”
B. “I need to stay out of the sun as much as possible.”
C. “I often skip dinner because I don’t feel hungry.”
D. “I always wear my medical identification.”
12. The physician prescribes regular insulin, 5 units subcutaneous. Regular
insulin begins to exert an effect:
A. In 5–10 minutes
B. In 10–20 minutes
C. In 30–60 minutes
D. In 60–120 minutes
Answer C: The time of onset for regular insulin is 30–60 minutes; therefore,
answers A, B, and D are incorrect.
13. The client is admitted from the emergency room with multiple injuries
sustained from an auto accident. His doctor prescribes a histamine blocker.
The reason for this order is:
A. To treat general discomfort
B. To correct electrolyte imbalances
C. To prevent stress ulcers
D. To treat nausea
14. The client with a recent liver transplant asks the nurse how long he will
have to take cyclosporine (Sandimmune). Which response is correct?
A. 1 year
B. 5 years
C. 10 years
D. The rest of his life
15. Shortly after the client was admitted to the postpartum unit, the nurse
notes heavy lochia rubra with large clots. The nurse should anticipate an
order for:
A. Methergine
B. Stadol
C. Magnesium sulfate
D. Phenergan
16. The client is scheduled to have an intravenous cholangiogram. Before
the procedure, the nurse should assess the patient for:
A. Shellfish allergies
B. Reactions to blood transfusions
C. Gallbladder disease
D. Egg allergies
17. A new diabetic is learning to administer his insulin. He receives 10U of
NPH and 12U of regular insulin each morning. Which of the following
statements reflects understanding of the nurse’s teaching?
A. “When drawing up my insulin, I should draw up the regular insulin first.”
B. “When drawing up my insulin, I should draw up the NPH insulin first.”
C. “It doesn’t matter which insulin I draw up first.”
D. “I cannot mix the insulin, so I will need two shots.”
18. A client with osteomylitis has an order for a trough level to be done
because he is taking Gentamycin. When should the nurse call the lab to
obtain the trough level?
A. Before the first dose
B. 30 minutes before the fourth dose
C. 30 minutes after the first dose
D. 30 minutes after the fourth dose
19. A 4-year-old with cystic fibrosis has a prescription for Viokase
pancreatic enzymes to prevent malabsorption. The correct time to give
pancreatic enzyme is:
A. 1 hour before meals
B. 2 hours after meals
C. With each meal and snack
D. On an empty stomach
20. Isoniazid (INH) has been prescribed for a family member exposed to
tuberculosis. The nurse is aware that the length of time that the medication
will be taken is:
A. 6 months
B. 3 months
C. 18 months
D. 24 months.
21. The client is admitted to the postpartum unit with an order to continue
the infusion of Pitocin. Which finding indicates that the Pitocin is having the
desired effect?
A. The fundus is deviated to the left.
B. The fundus is firm and in the midline.
C. The fundus is boggy.
D. The fundus is two finger breadths below the umbilicus.
22. The nurse is teaching a group of new graduates about the safety needs of
the client receiving chemotherapy. Before administering chemotherapy, the
nurse should:
A. Administer a bolus of IV fluid
B. Administer pain medication
C. Administer an antiemetic
D. Allow the patient a chance to eat
23. Before administering Methytrexate orally to the client with cancer, the
nurse should check the:
A. IV site
B. Electrolytes
C. Blood gases
D. Vital signs
24. Vitamin K (aquamephyton) is administered to a newborn shortly after
birth for which of the following reasons?
A. To prevent dehydration
B. To treat infection
C. To replace electrolytes
D. To facilitate clotting
25. The client with an ileostomy is being discharged. Which teaching should
be included in the plan of care?
A. Use Karaya powder to seal the bag.
B. Irrigate the ileostomy daily.
C. Stomahesive is the best skin protector.
D. Neosporin ointment can be used to protect the skin.
126. The client has an order for FeSo4 liquid. Which method of
administration would be best?
A. Administer the medication with milk
B. Administer the medication with a meal
C. Administer the medication with orange juice
D. Administer the medication undiluted
27. The client arrives in the emergency room with a hyphema. Which action
by the nurse would be best?
A. Elevate the head of the bed and apply ice to the eye
B. Place the client in a supine position and apply heat to the knee
C. Insert a Foley catheter and measure the intake and output
D. Perform a vaginal exam and check for a discharge
28. The nurse is making assignments for the day. Which client should be
assigned to the nursing assistant?
A. The 18-year-old with a fracture to two cervical vertebrae
B. The infant with meningitis
C. The elderly client with a thyroidectomy 4 days ago
D. The client with a thoracotomy 2 days ago
29. The client arrives in the emergency room with a “bull’s eye” rash.
Which question would be most appropriate for the nurse to ask the client?
A. “Have you found any ticks on your body?”
B. “Have you had any nausea in the last 24 hours?”
C. “Have you been outside the country in the last 6 months?”
D. “Have you had any fever for the past few days?”
30. Which of the following is the best indicator of the diagnosis of HIV?
A. White blood cell count
B. ELISA
C. Western Blot
D. Complete blood count
31. The client has an order for gentamycin to be administered. Which lab
results should be reported to the doctor before beginning the medication?
A. Hematocrit
B. Creatinine
C. White blood cell count
D. Erythrocyte count
32. The nurse is caring for the client with a mastectomy. Which action
would be contraindicated?
A. Taking the blood pressure in the side of the mastectomy
B. Elevating the arm on the side of the mastectomy
C. Positioning the client on the unaffected side
D. Performing a dextrostix on the unaffected side
33. The charge nurse is making assignments for the day. After accepting the
assignment to a client with leukemia, the nurse tells the charge nurse that her
child has chickenpox. Which action should the charge nurse take?
A. Change the nurse’s assignment to another client
B. Explain to the nurse that there is no risk to the client
C. Ask the nurse if the chickenpox have scabbed
D. Ask the nurse if she has ever had the chickenpox
34. The client with brain cancer refuses to care for herself. Which action by
the nurse would be best?
A. Alternate nurses caring for the client so that the staff will not get tired of
caring for this client
B. Talk to the client and explain the need for self-care
C. Explore the reason for the lack of motivation seen in the client
D. Talk to the doctor about the client’s lack of motivation
35. The nurse is caring for the client who has been in a coma for 2 months.
He has signed a donor card, but the wife is opposed to the idea of organ
donation. How should the nurse handle the topic of organ donation with the
wife?
A. Contact organ retrieval to come talk to the wife
B. Tell her that because her husband signed a donor card, the hospital has the
right to take the organs upon the death of her husband
C. Drop the subject until a later time
D. Refrain from talking about the subject until after the death of her husband
36. The nurse is assessing the abdomen. The nurse knows the best sequence
to perform the assessment is:
A. Inspection, auscultation, palpation
B. Auscultation, palpation, inspection
C. Palpation, inspection, auscultation
D. Inspection, palpation, auscultation
37. The nurse is assisting in the assessment of the patient admitted with
abdominal pain. Why should the nurse ask about medications that the client is
taking?
A. Interactions between medications can be identified.
B. Various medications taken by mouth can affect the alimentary tract.
C. This will provide an opportunity to educate the patient regarding the
medications used.
D. The types of medications might be attributable to an abdominal pathology
not already identified.
38. The nurse is asked by the nurse aide, “Are peptic ulcers really caused by
stress?” The nurse would be correct in replying with which of the following:
A. “Peptic ulcers result from overeating fatty foods.”
B. “Peptic ulcers are always caused from exposure to continual stress.”
C. “Peptic ulcers are like all other ulcers, which all result from stress.”
D. “Peptic ulcers are associated with H. pylori, although there are other ulcers
that are associated with stress.”
139. The client is newly diagnosed with juvenile onset diabetes. Which of the
following nursing diagnoses is a priority?
A. Anxiety
B. Pain
C. Knowledge deficit
D. Altered thought process
40. The nurse understands that the diagnosis of oral cancer is confirmed
with:
A. Biopsy
B. Gram Stain
C. Scrape cytology
D. Oral washings for cytology
41. The nurse is assisting in the care of a patient who is 2 days postoperative from a hemorroidectomy. The nurse would be correct in instructing
the patient to:
A. Avoid a high-fiber diet because this can hasten the healing time
B. Continue to use ice packs until discharge and then when at home
C. Take 200mg of Colace bid to prevent constipation
D. Use a sitz bath after each bowel movement to promote cleanliness and
comfort
42. The nurse is caring for a patient with a colostomy. The patient asks,
“Will I ever be able to swim again?” The nurse’s best response would be:
A. “Yes, you should be able to swim again, even with the colostomy.”
B. “You should avoid immersing the colostomy in water.”
C. “No, you should avoid getting the colostomy wet.”
D. “Don’t worry about that. You will be able to live just like you did before.”
43. Which is true regarding the administration of antacids?
A. Antacids should be administered without regard to mealtimes.
B. Antacids should be administered with each meal and snack of the day.
C. Antacids should be administered within 1–2 hours of all other
medications.
D. Antacids should be administered with all other medications, for maximal
absorption.
44. The nurse is preparing to administer a feeding via a nasogastric tube.
The nurse would perform which of the following before initiating the
feeding?
A. Assess for tube placement by aspirating stomach content
B. Place the patient in a left-lying position
C. Administer feeding with 50% H20 concentration
D. Ensure that the feeding solution has been warmed in a microwave for 2
minutes
45. The patient is prescribed metronidazole (Flagyl) for adjunct treatment
for a duodenal ulcer. When teaching about this medication, the nurse would
say:
A. “This medication should be taken only until you begin to feel better.”
B. “This medication should be taken on an empty stomach to increase
absorption.”
C. “While taking this medication, you do not have to be concerned about
being in the sun.”
D. “While taking this medication, alcoholic beverages and products
containing alcohol should be avoided.”
46. In planning care for the patient with ulcerative colitis, the nurse
identifies which nursing diagnoses as a priority?
A. Anxiety
B. Impaired skin integrity
C. Fluid volume deficit
D. Nutrition altered, less than body requirements
47. The nurse is teaching about irritable bowel syndrome (IBS). Which of
the following would be most important?
A. Reinforcing the need for a balanced diet
B. Encouraging the client to drink 16 ounces of fluid with each meal
C. Telling the client to eat a diet low in fiber
D. Instructing the client to limit his intake of fruits and vegetables
148. The nurse is planning care for the patient with celiac disease. In teaching
about the diet, the nurse should instruct the patient to avoid which of the
following for breakfast?
A. Cream of wheat
B. Banana
C. Puffed rice
D. Cornflakes
49. The nurse is caring for a patient with suspected diverticulitis. The nurse
would be most prudent in questioning which of the following diagnostic tests
ordered?
A. Colonoscopy
B. Barium enema
C. Complete blood count
D. Computed tomography (CT) scan
50. When the nurse is gathering information for the assessment, the patient
states, “My stomach hurts about 2 hours after I eat.” Based upon this
information, the nurse knows the patient likely has a:
A. Gastric ulcer
B. Duodenal ulcer
C. Peptic ulcer
D. Curling’s ulcer
51. The registered nurse is conducting an in-service for colleagues about
peptic ulcers. The nurse would be correct in identifying which of the
following as a causative factor?
A. N. gonorrhea
B. H. influenza
C. H. pylori
D. E. coli
.
52. The nurse is caring for the patient’s post-surgical removal of a 6mm oral
cancerous lesion. The priority nursing measure would be to:
A. Maintain a patent airway
B. Perform meticulous oral care every 2 hours
C. Ensure that the incisional area is kept as dry as possible
D. Assess the client frequently for pain using the visual analogue scale.
53. The nurse is assisting in the care of a patient with diverticulosis. Which
of the following assessment findings would necessitate a report to the doctor?
A. Bowel sounds of 5–20 seconds
B. Intermittent left lower-quadrant pain
C. Constipation alternating with diarrhea
D. Hemoglobin 26% and hematocrit 32
.
54. The nurse is assessing the client admitted for possible oral cancer. The
nurse identifies which of the following as a late-occurring symptom of oral
cancer?
A. Warmth
B. Odor
C. Pain
D. Ulcer with flat edges
55. An obstetrical client decides to have an epidural anesthetic to relieve
pain during labor. Following administration of the anesthesia, the nurse
should:
A. Monitor the client for seizures
B. Monitor the client for orthostatic hypotension
C. Monitor the client for respiratory depression
D. Monitor the client for hematuria
56. The nurse is performing an assessment of an elderly client with a total
hip repair. Based on this assessment, the nurse decides to medicate the client
with an analgesic. Which finding most likely prompted the nurse to decide to
administer the analgesic?
A. The client’s blood pressure is 130/86.
B. The client is unable to concentrate.
C. The client’s pupils are dilated.
D. The client grimaces during care.
57. A client who has chosen to breastfeed complains to the nurse that her
nipples became very sore while she was breastfeeding her older child. Which
measure will help her to avoid soreness of the nipples?
A. Feeding the baby during the first 48 hours after delivery
B. Breaking suction by placing a finger between the baby’s mouth and the
breast when she terminates the feeding
C. Applying warm, moist soaks to the breast several times per day
D. Wearing a support bra
58. The nurse asked the client if he has an advance directive. The reason for
asking the client this question is:
A. She is curious about his plans regarding funeral arrangements.
B. Much confusion can occur with the client’s family if he does not have an
advanced directive.
C. An advanced directive allows the medical personnel to make all decisions
for the client.
D. An advanced directive allows active euthanasia.
.
59. The doctor has ordered a Transcutaneous Electrical Nerve Stimulation
(TENS) unit for the client with chronic back pain. The nurse teaching the
client with a TENS unit should tell the client:
A. “You may be electrocuted if you use water with this unit.”
B. “Please report skin irritation to the doctor.”
C. “The unit may be used anywhere on the body without fear of adverse
reactions.”
D. “A cream should be applied to the skin before applying the unit.”
60. The doctor has ordered a patient-controlled analgesia (PCA) pump for
the client with chronic pain. The client asks the nurse if he can become
overdosed with pain medication using this machine. The nurse demonstrates
understanding of the PCA if she states:
A. “The machine will administer only the amount that you need to control
your pain without your taking any action.”
B. “The machine has a locking device that prevents overdosing to occur.”
C. “The machine will administer one large dose every 4 hours to relieve your
pain.”
D. “The machine is set to deliver medication only if you need it.”
61. The 84-year-old male has returned from the recovery room following a
total hip repair. He complains of pain and is medicated by morphine sulfate
and promethazine. Which medication should be kept available for the client
being treated with opoid analgesics?
A. Nalozone (Narcan)
B. Ketorolac (Toradol)
C. Acetylsalicylic acid (aspirin)
D. Atropine sulfate (Atropine)
62. The nurse is taking the vital signs of the client admitted with cancer of
the pancreas. The nurse is aware that the fifth vital sign is:
A. Anorexia
B. Pain
C. Insomnia
D. Fatigue
63. The client with AIDS tells the nurse that he has been using acupuncture
to help with his pain. The nurse should question the client regarding this
treatment because acupuncture:
A. Uses pressure from the fingers and hands to stimulate the energy points in
the body
B. Uses oils extracted from plants and herbs
C. Uses needles to stimulate certain points on the body to treat pain
D. Uses manipulation of the skeletal muscles to relieve stress and pain
64. The client has an order for heparin to prevent post-surgical thrombi.
Immediately following a heparin injection, the nurse should:
A. Aspirate for blood
B. Check the pulse rate
C. Massage the site
D. Check the site for bleeding
65. Which of the following lab studies should be done periodically if the
client is taking sodium warfarin (Coumadin)?
A. Stool specimen for occult blood
B. White blood cell count
C. Blood glucose
D. Erthyrocyte count
66. The doctor has ordered 80mg of furosemide (Lasix) two times per day.
The nurse notes the patient’s potassium level to be 2.5meq/L. The nurse
should:
A. Administer the Lasix as ordered
B. Administer half the dose
C. Offer the patient a potassium-rich food
D. Withhold the drug and call the doctor
67. The doctor is preparing to remove chest tubes from the client’s left
chest. In preparation for the removal, the nurse should instruct the client to:
A. Breathe normally
B. Hold his breath and bear down
C. Take a deep breath
D. Sneeze on command
68. The nurse identifies ventricular tachycardia on the heart monitor. Which
action should the nurse prepare to take?
A. Administer atropine sulfate
B. Check the potassium level
C. Administer an antiarrythmic medication such as Lidocaine
D. Defibrillate at 360 joules
69. A client is being monitored using a central venous pressure monitor. If
the pressure is 2cm of water, the nurse should:
A. Call the doctor immediately
B. Slow the intravenous infusion
C. Listen to the lungs for rales
D. Administer a diuretic
70. The nurse is evaluating the client’s pulmonary artery pressure. The nurse
is aware that this test will evaluate:
A. Pressure in the left ventricle
B. The systolic, diastolic, and mean pressure of the pulmonary artery
C. The pressure in the pulmonary veins
D. The pressure in the right ventricle
71. The physician has ordered atropine sulfate 0.4mg IM before surgery.
The medication is supplied in 0.8mg per milliliter. The nurse should
administer how many milliliters of the medication?
A. 0.25mL
B. 0.5mL
C. 1mL
D. 1.25mL
72. If the nurse is unable to illicit the deep tendon reflexes of the patella, the
nurse should ask the client to:
A. Pull against the palms
B. Grimace the facial muscles
C. Cross the legs at the ankles
D. Perform Valsalva maneuver
73. A client with an abdominal aortic aneurysm is admitted in preparation
for surgery. Which of the following should be reported to the doctor?
A. An elevated white blood cell count
B. An abdominal bruit
C. A negative Babinski reflex
D. Pupils that are equal and reactive to light
.
74. A 4-year-old male is admitted to the unit with nephotic syndrome. He is
extremely edematous. To decrease the discomfort associated with scrotal
edema, the nurse should:
A. Apply ice to the scrotum
B. Elevate the scrotum on a small pillow
C. Apply heat to the abdominal area
D. Administer a diuretic
75. The nurse is taking the blood pressure of an obese client. If the blood
pressure cuff is too small, the results will be:
A. A false elevation
B. A false low reading
C. A blood pressure reading that is correct
D. A subnormal finding
76. The client is admitted with thrombophlebitis and an order for heparin.
The medication should be administered using:
A. Buretrol
B. A tuberculin syringe
C. Intravenous controller
D. Three-way stop-cock
77. The client is admitted to the hospital in chronic renal failure. A diet low
in protein is ordered. The rationale for a low-protein diet is:
A. Protein breaks down into blood urea nitrogen and metabolic waste.
B. High protein increases the sodium and potassium levels.
C. A high-protein diet decreases albumin production.
D. A high-protein diet depletes calcium and phosphorous.
78. The client is admitted to the unit after a motor vehicle accident with a
temperature of 102°F rectally. The nurse is aware that the most likely
explanation for the elevated temperature is:
A. There was damage to the hypothalamus.
B. He has an infection from the abrasions to the head and face.
C. He will require a cooling blanket to decrease the temperature.
D. There was damage to the frontal lobe of the brain.
79. The nurse is caring for the client following a cerebral vascular accident.
Which portion of the brain is responsible for taste, smell, and hearing?
A. Occipital
B. Frontal
C. Temporal
D. Parietal
80. A 20-year-old is admitted to the rehabilitation unit following a
motorcycle accident. Which would be the appropriate method for measuring
the client for crutches?
A. Measuring five finger breaths under the axilla
B. Measuring 3 inches under the axilla
C. Measuring the client with the elbows flexed 10°
D. Measuring the client with the crutches 20 inches from the side of the foot
81. The nurse is doing bowel and bladder retraining for the client with
paraplegia. Which of the following is not a factor for the nurse to consider?
A. Dietary patterns
B. Mobility
C. Fluid intake
D. Sexual function
82. The client returns to the recovery room following repair of an
intrathoracic aneurysm. Which finding would require further investigation?
A. Pedal pulses bounding and regular
B. Urinary output 20mL in the past hour
C. Blood pressure 108/50
D. Oxygen saturation 97%
83. The nurse is teaching the client regarding use of sodium warfarin.
Which statement made by the client would require further teaching?
A. “I will have blood drawn every month.”
B. “I will assess my skin for a rash.”
C. “I take aspirin for a headache.”
D. “I will use an electric razor to shave.”
84. A client with a femoral popliteal bypass graft is assigned to a
semiprivate room. The most suitable roommate for this client is the client
with:
A. Hypothyroidism
B. Diabetic ulcers
C. Ulcerative colitis
D. Pneumonia
85. The nurse has just received shift report and is preparing to make rounds.
Which client should be seen first?
A. The client who has a history of a cerebral aneurysm with an oxygen
saturation rate of 99%
B. The client who is three days post–coronary artery bypass graft with a
temperature of 100.2°F
C. The client who was admitted 1 hour ago with shortness of breath
D. The client who is being prepared for discharge following a femoral
popliteal bypass graft
86. The doctor has ordered antithrombolic stockings to be applied to the legs
of the client with peripheral vascular disease. The nurse knows that the
proper method of applying the stockings is:
A. Before rising in the morning
B. With the client in a standing position
C. After bathing and applying powder
D. Before retiring in the evening
87. The nurse is preparing a client with an axillo-popliteal bypass graft for
discharge. The client should be taught to avoid:
A. Using a recliner to rest
B. Resting in supine position
C. Sitting in a straight chair
D. Sleeping in right Sim’s position
88. While caring for a client with hypertension, the nurse notes the
following vital signs: BP of 140/20, pulse 120, respirations 36, temperature
100.8°F. The nurse’s initial action should be to:
A. Call the doctor
B. Recheck the vital signs
C. Obtain arterial blood gases
D. Obtain an ECG
89. The nurse is caring for a client with peripheral vascular disease. To
correctly assess the oxygen saturation level, the monitor may be placed on
the:
A. Abdomen
B. Ankle
C. Earlobe
D. Chin
90. Dalteparin (Fragmin) has been ordered for a client with pulmonary
embolis. Which statement made by the graduate nurse indicates inadequate
understanding of the medication?
A. “I will administer the medication before meals.”
B. “I will administer the medication in the abdomen.”
C. “I will check the PTT before administering the medication.”
D. “I will not need to aspirate when I give Dalteparin.”
91. The client has a prescription for a calcium carbonate compound to
neutralize stomach acid. The nurse should assess the client for:
A. Constipation
B. Hyperphosphatemia
C. Hypomagnesemia
D. Diarrhea
92. A client who has been receiving urokinase has a large bloody bowel
movement. What nursing action would be best for the nurse to take
immediately?
A. Administer vitamin K IM
B. Discontinue the urokinase
C. Reduce the urokinase and administer heparin
D. Stop the urokinase, notify the physician, and prepare to administer amicar
93. Which of the following best describes the language of a 24-month-old?
A. Doesn’t understand yes and no
B. Understands the meaning of words
C. Able to verbalize needs
D. Continually asks “Why?” to most topics.
94. In terms of cognitive development, a 2-year-old would be expected to:
A. Think abstractly
B. Use magical thinking
C. Understand conservation of matter
D. See things from the perspective of others
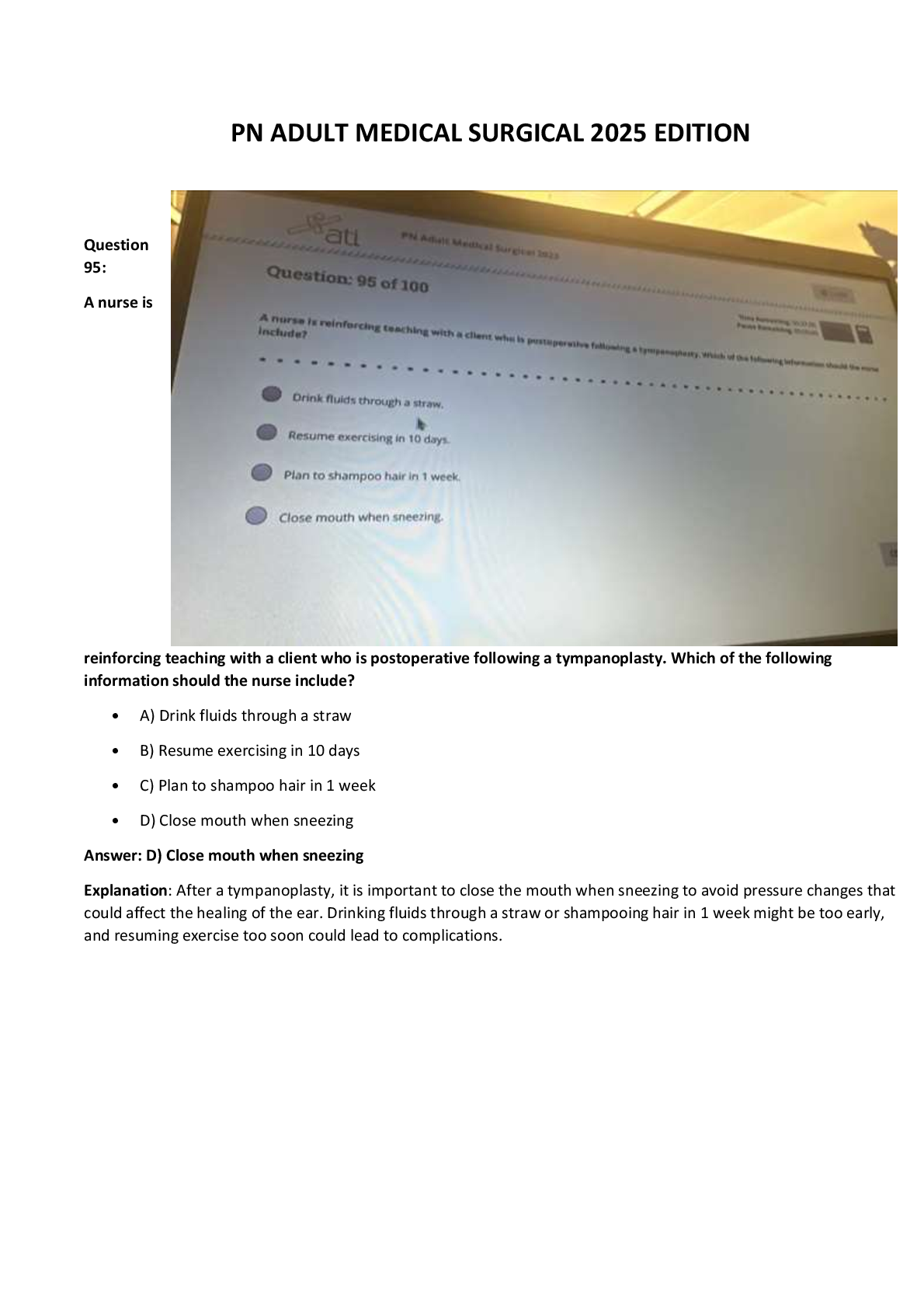
95. The nurse is ready to begin an exam on a 9-month-old infant. The child
is sitting in his mother’s lap. What should the nurse do first?
A. Check the Babinski reflex
B. Listen to the heart and lung sounds
C. Palpate the abdomen
D. Check tympanic membranes
96. Which of the following examples represents parallel play?
A. Jenny and Tommy share their toys.
B. Jimmy plays with his car beside Mary, who is playing with her doll.
C. Kevin plays a game of Scrabble with Kathy and Sue.
D. Mary plays with a handheld game while sitting in her mother’s lap.
97. Assuming that all have achieved normal cognitive and emotional
development, which of the following children is at greatest risk for accidental
poisoning?
A. A 6-month-old
B. A 4-year-old
C. A 10-year-old
D. A 13-year-old
98. An important intervention in monitoring the dietary compliance of a
client with bulimia is:
A. Allowing the client privacy during mealtimes
B. Praising her for eating all her meals
C. Observing her for 1–2 hours after meals
D. Encouraging her to choose foods she likes and to eat in moderation
99. The client is admitted for evaluation of aggressive behavior and
diagnosed with antisocial personality disorder. A key part of the care of such
a client is:
A. Setting realistic limits
B. Encouraging the client to express remorse for behavior
C. Minimizing interactions with other clients
D. Encouraging the client to act out feelings of rage
100. A client with a diagnosis of passive-aggressive personality disorder is
seen at the local mental health clinic. A common characteristic of persons
with passive-aggressive personality disorder is:
A. Superior intelligence
B. Underlying hostility
C. Dependence on others
D. Ability to share feelings
[Show More]











 2ND EDITION JUDITH C.png)
 2ND EDITION JUDITH C.png)
.png)

