Shale Gas Development; the Creation and Extraction process
$ 3
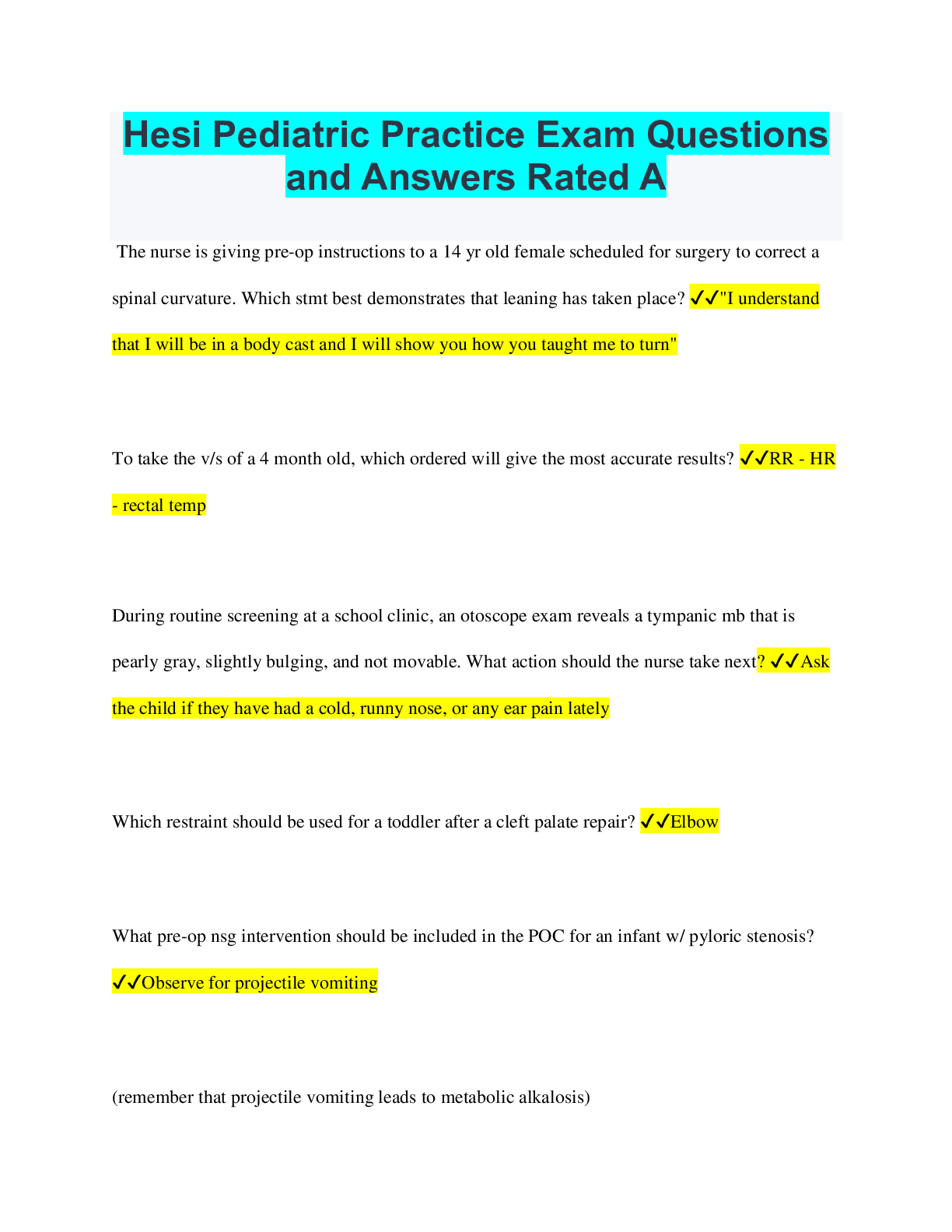
Hesi Pediatric Practice Exam Questions and Answers Rated A
$ 7.5
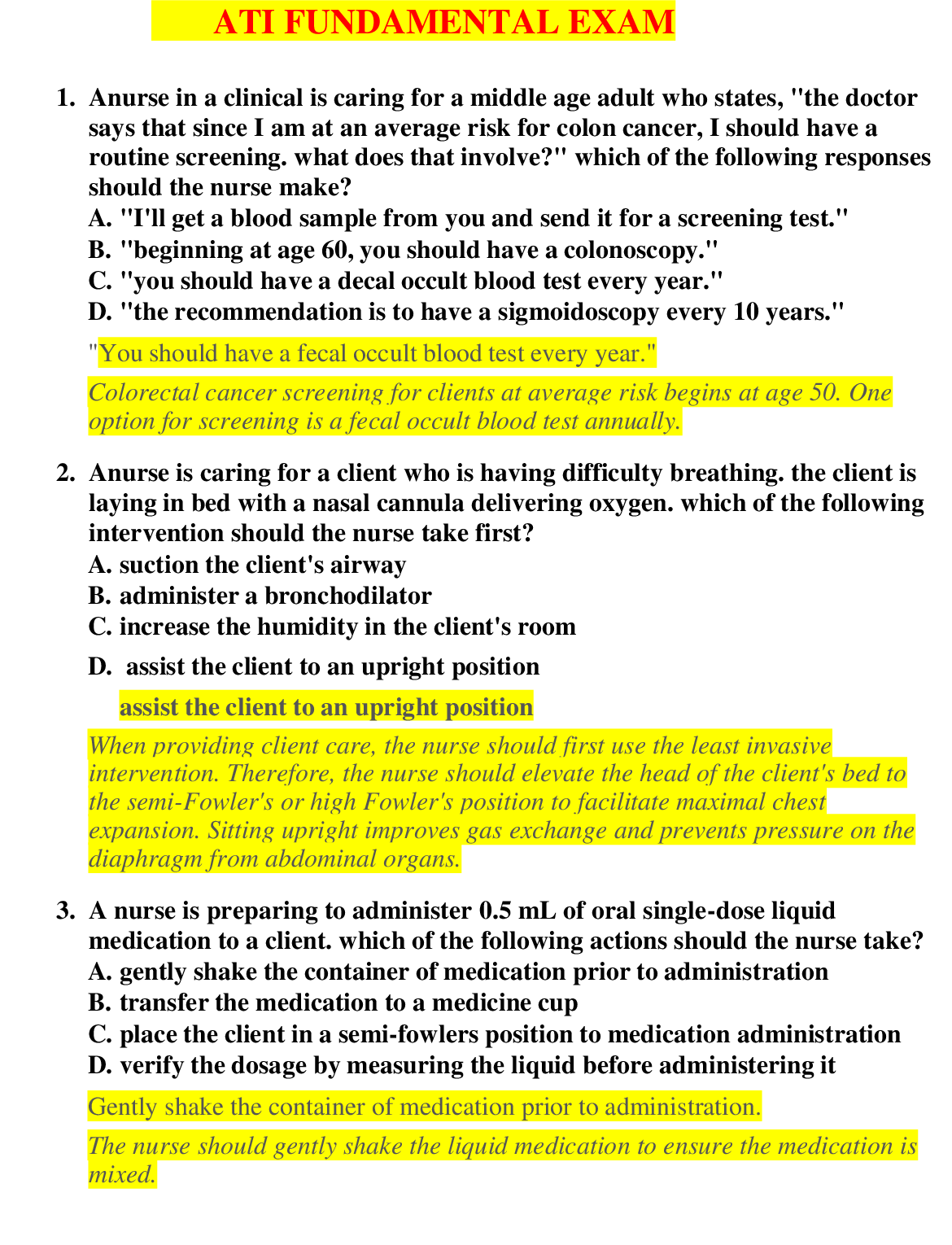
ATI / RN Fundamentals Exam |RN Fundamentals Online Practice A and B| 120 Questions and Answers | LATEST 2021 / 2022
$ 15

Sophia Intro to Stats Unit 1 Milestone 1, Latest Questions and Answers with Explanations, All Correct Study Guide, Download to Score A
$ 12
TNCC 2022 Study Guide With Solution
$ 5.5
Neck Pain Case Study: In-Depth iHuman Analysis of a 30-Year-Old Female Patient (Class 6512) | Week
$ 18
ATI CAP-MED SURG-ASSESSMENT 2 QUESTIONS AND ANSWERS 2023
$ 18
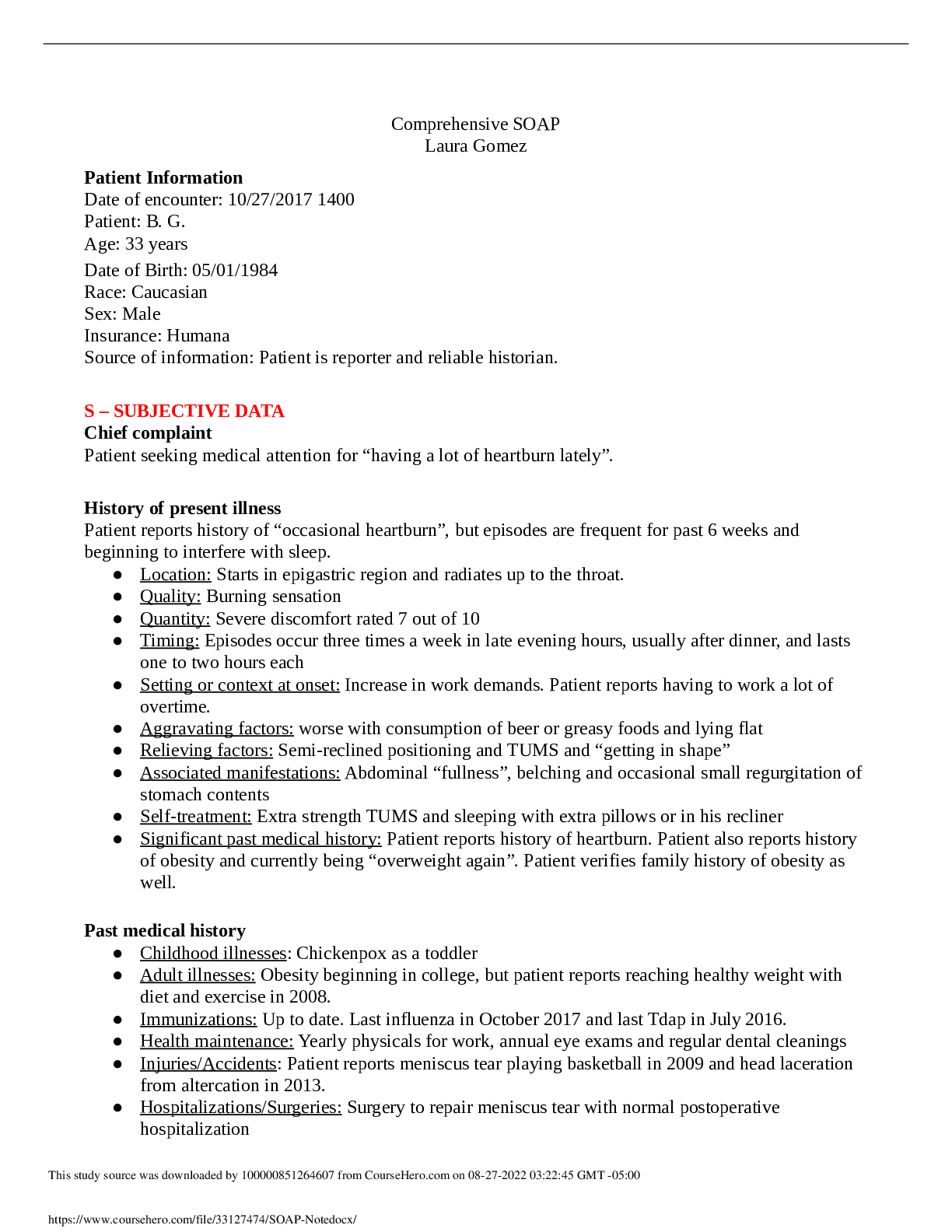
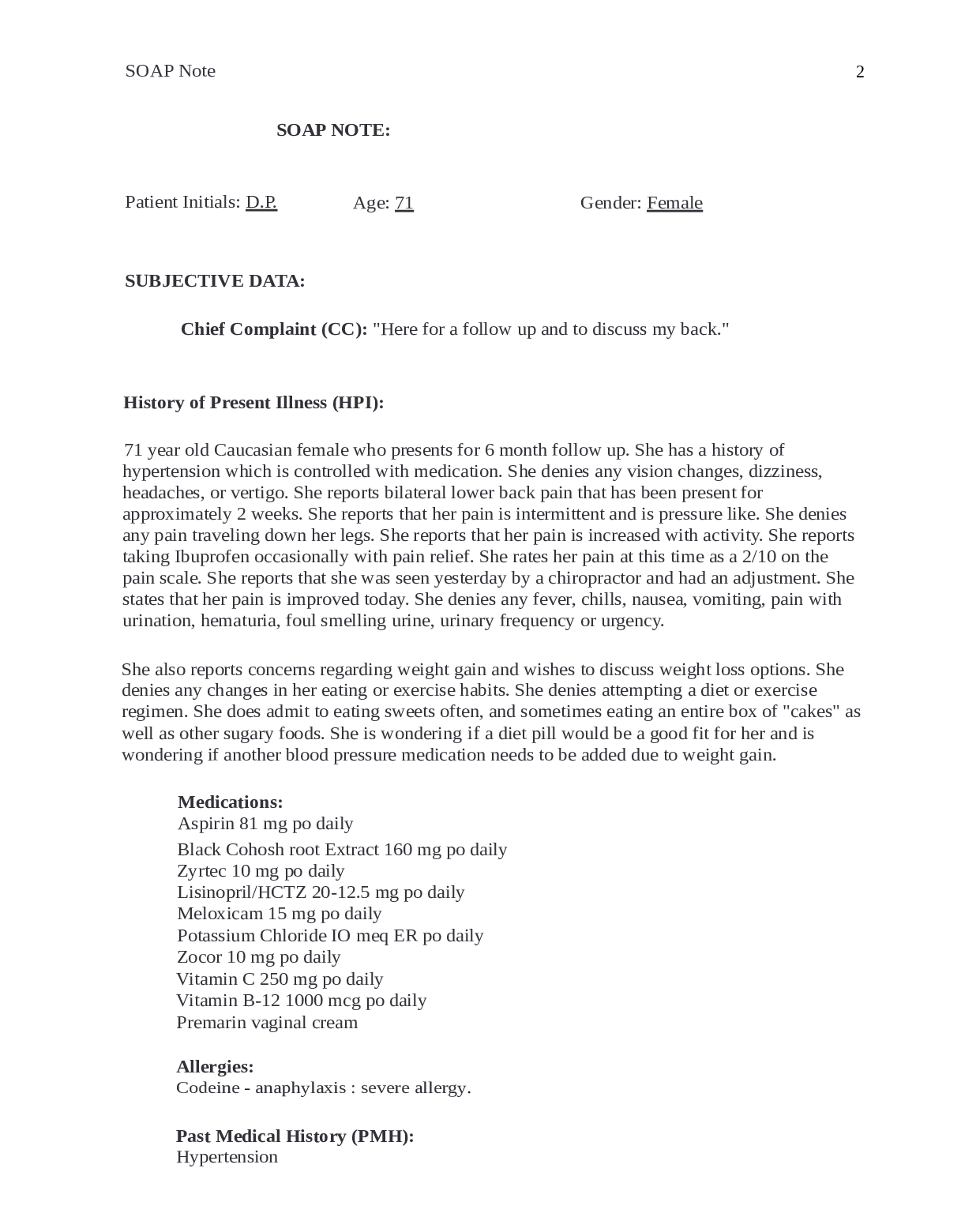
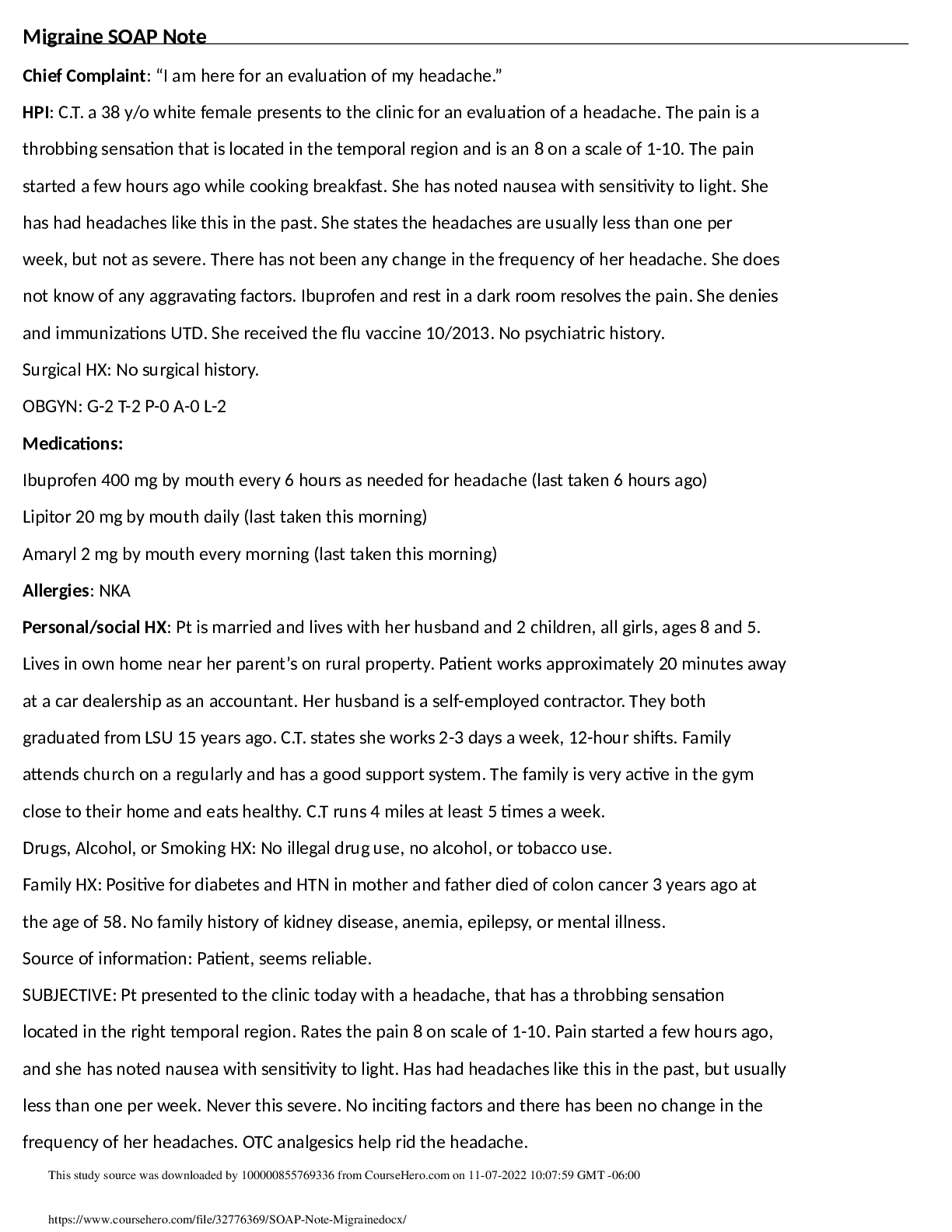
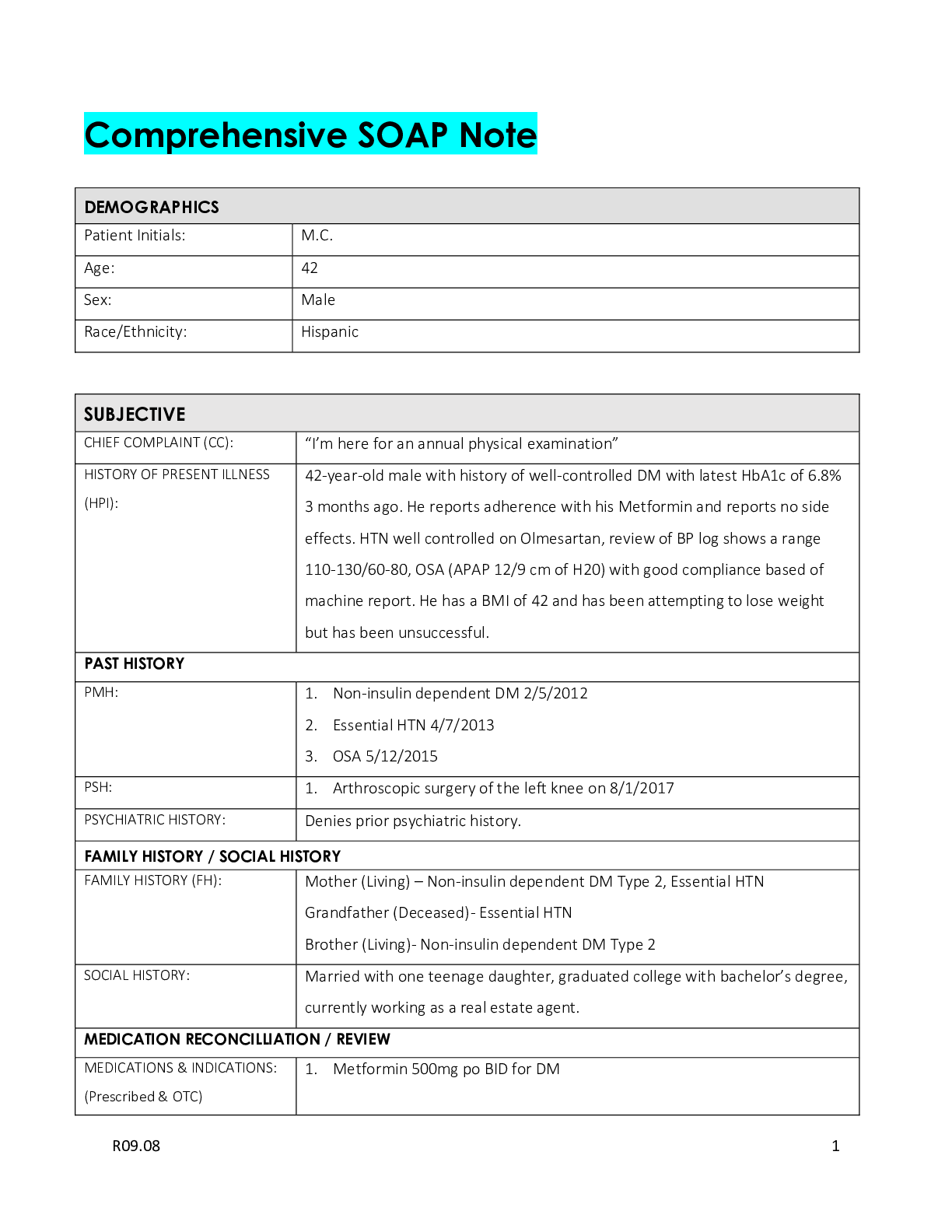
NURS 6531N-9 Advanced Practice Care of Adults Comprehensive SOAP Note
$ 13
C273 SOCG 1010 Introduction to Sociology (WGU) FA Review Qns & Ans 2025
$ 11
IPOE Exam Study Guide - Questions and Answers
$ 13
COP 1000 Module 7 Quiz - Questions and Answers
$ 12
Teaching Assistance Manual For Economics A Contemporary Introduction 10th Edition William A. McEachern
$ 19
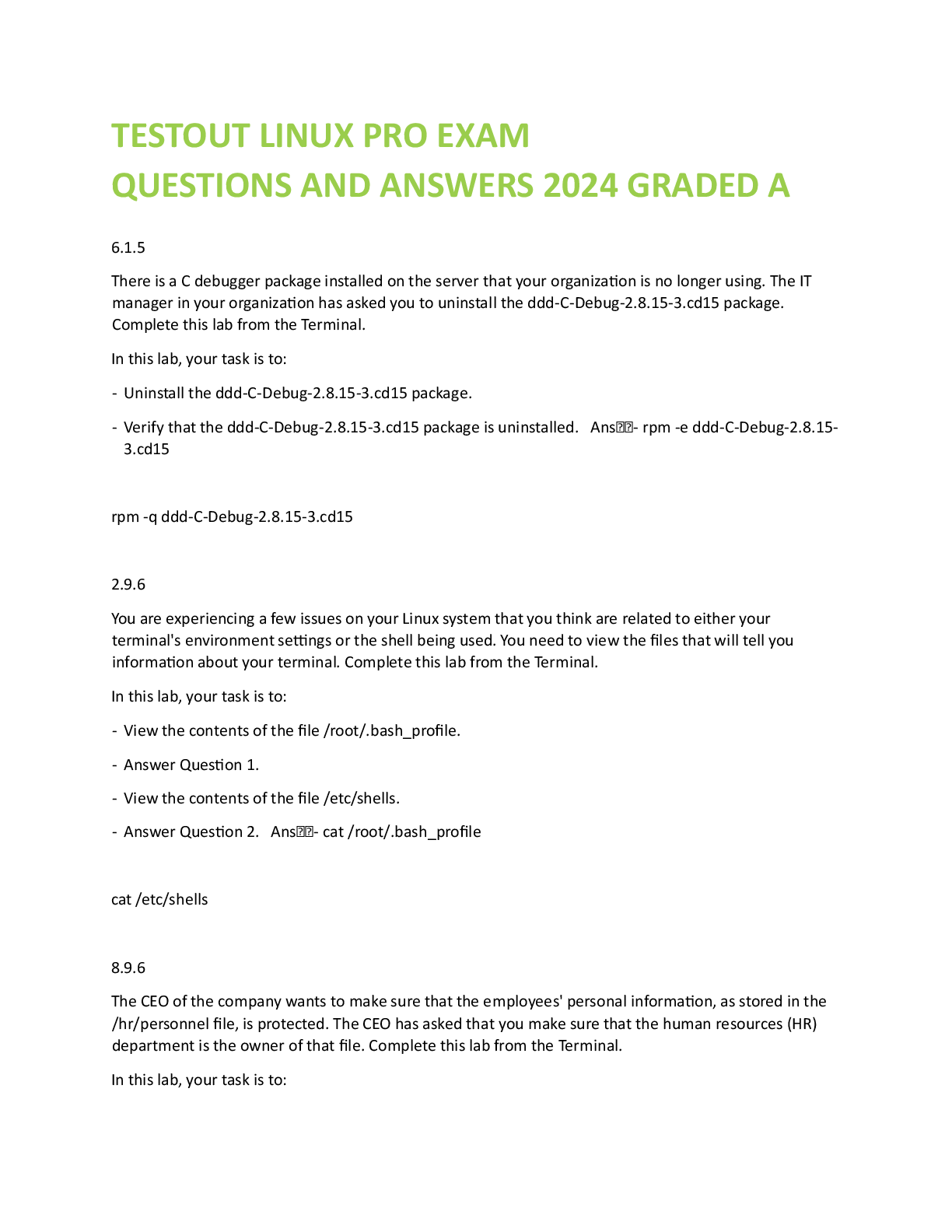
TESTOUT LINUX PRO EXAM QUESTIONS AND ANSWERS 2024 GRADED A
$ 18.5
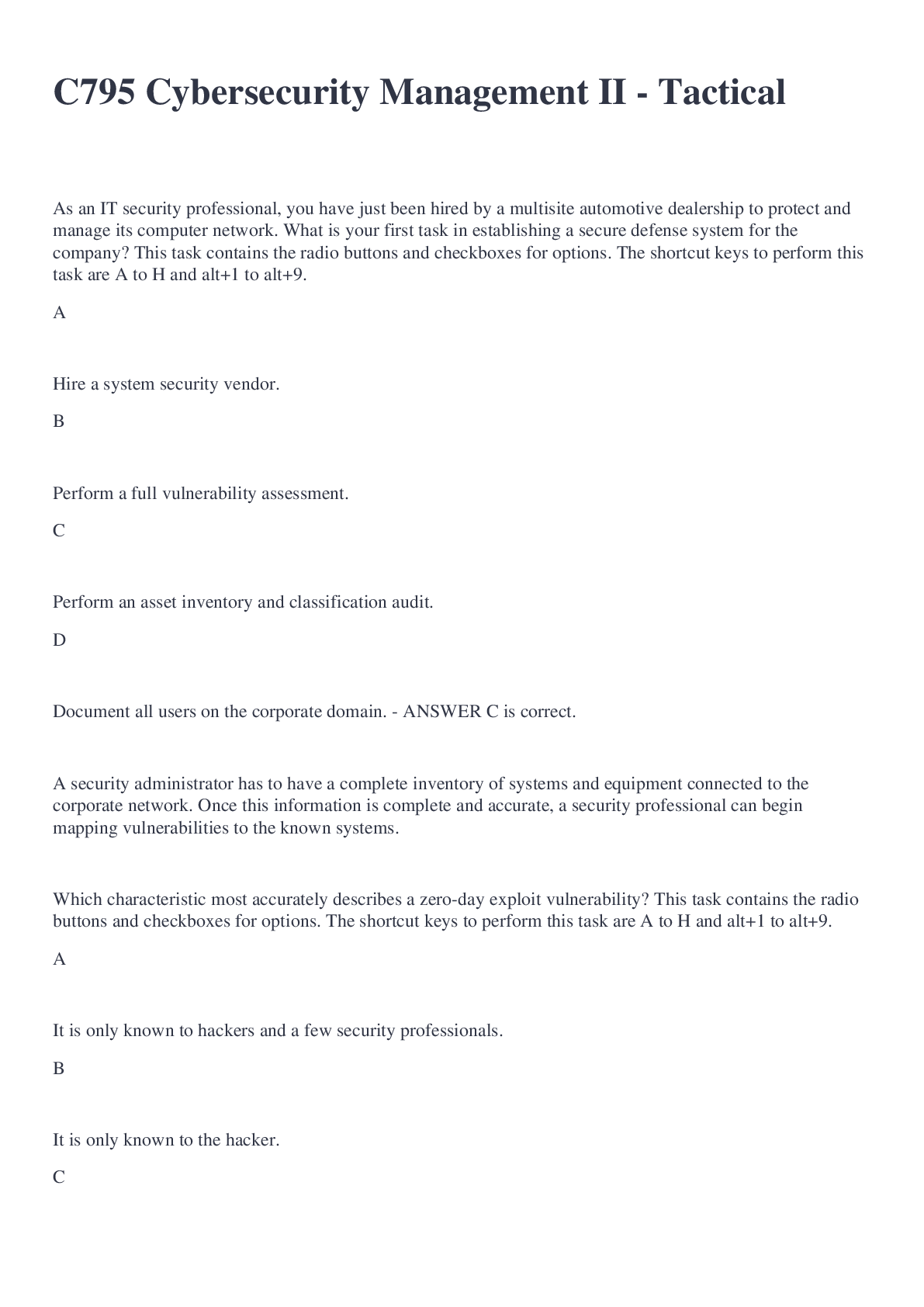
C795 Cybersecurity Management II - Tactical Questions and Answers 2022/2023 Graded A+
$ 11
Titration Gizmo Assessment Answers
$ 7
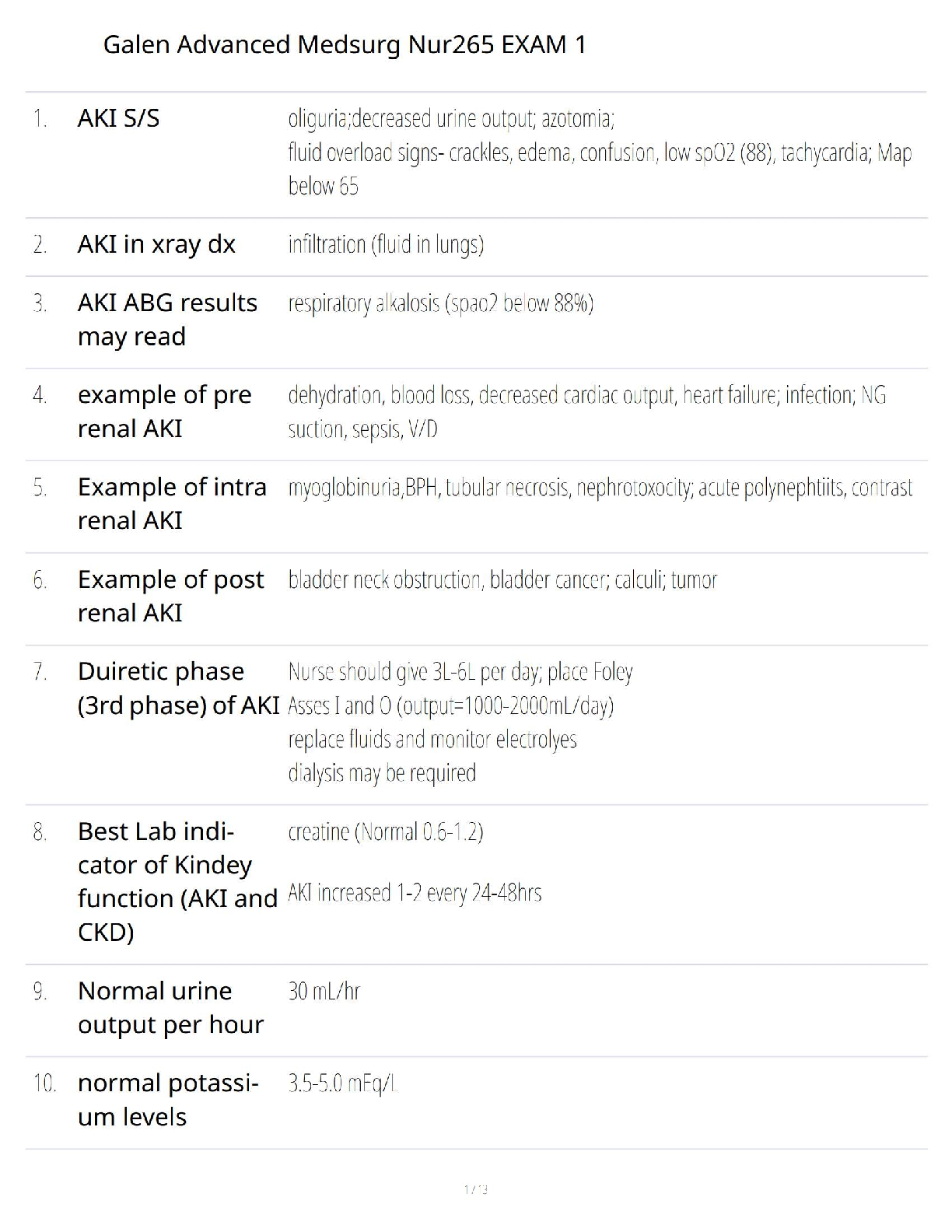
Galen NUR 265 Exam 1 Study Guide: Mastering Advanced Medical-Surgical Nursing Concepts
$ 14.5
eBook [PDF] Deconstructing Doctoral Discourses Stories and Strategies for Success 1st Edition By Deborah L. Mulligan, Naomi Ryan, Patrick Alan Danaher
$ 29
MATH 533 Week 2 Quiz – Questions For Revision
$ 8
OCR A LEVEL 2024 GCE New Business H031/02: The wider business environment A Level QUESTION PAPER AND MARK SCHEME MERGED
$ 7
wellchild.png)
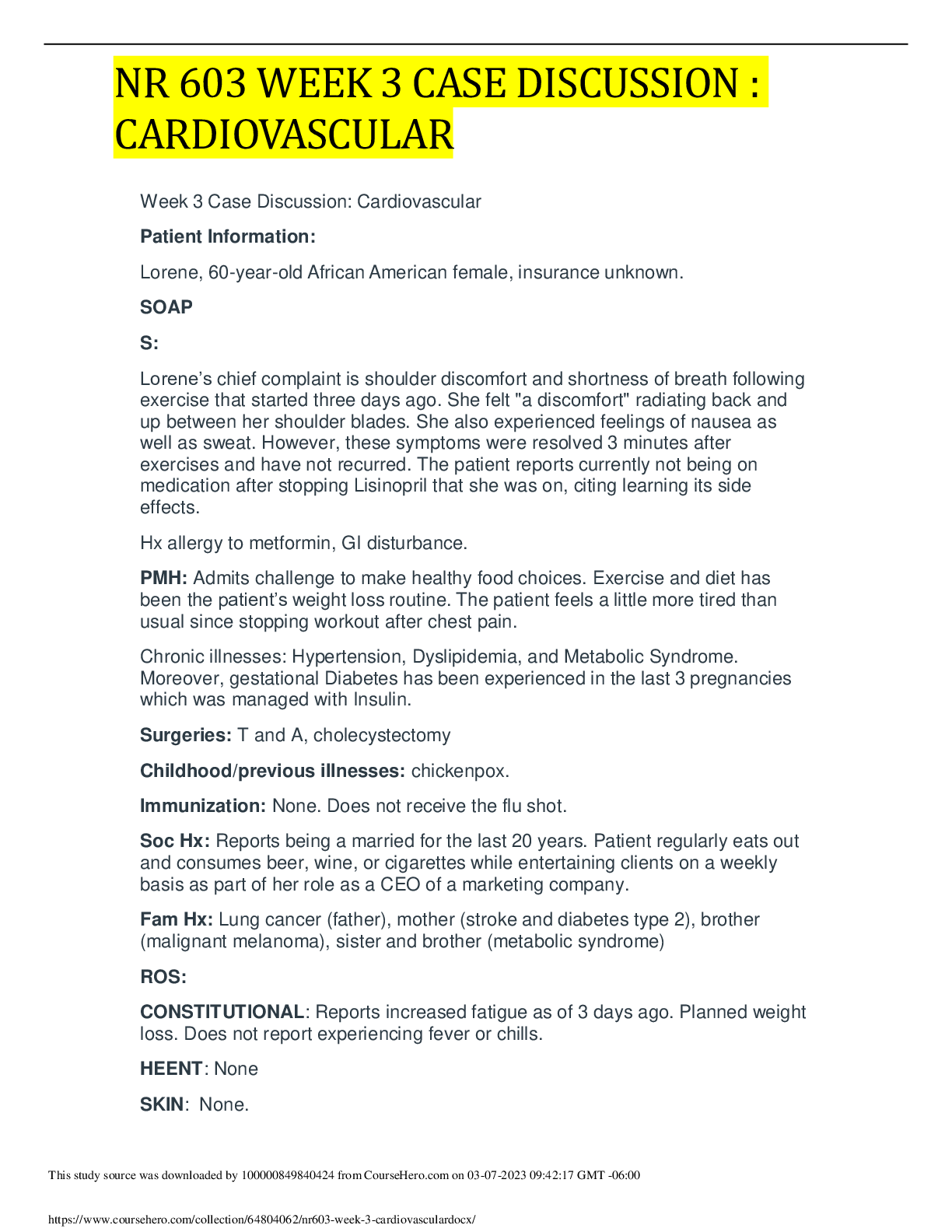
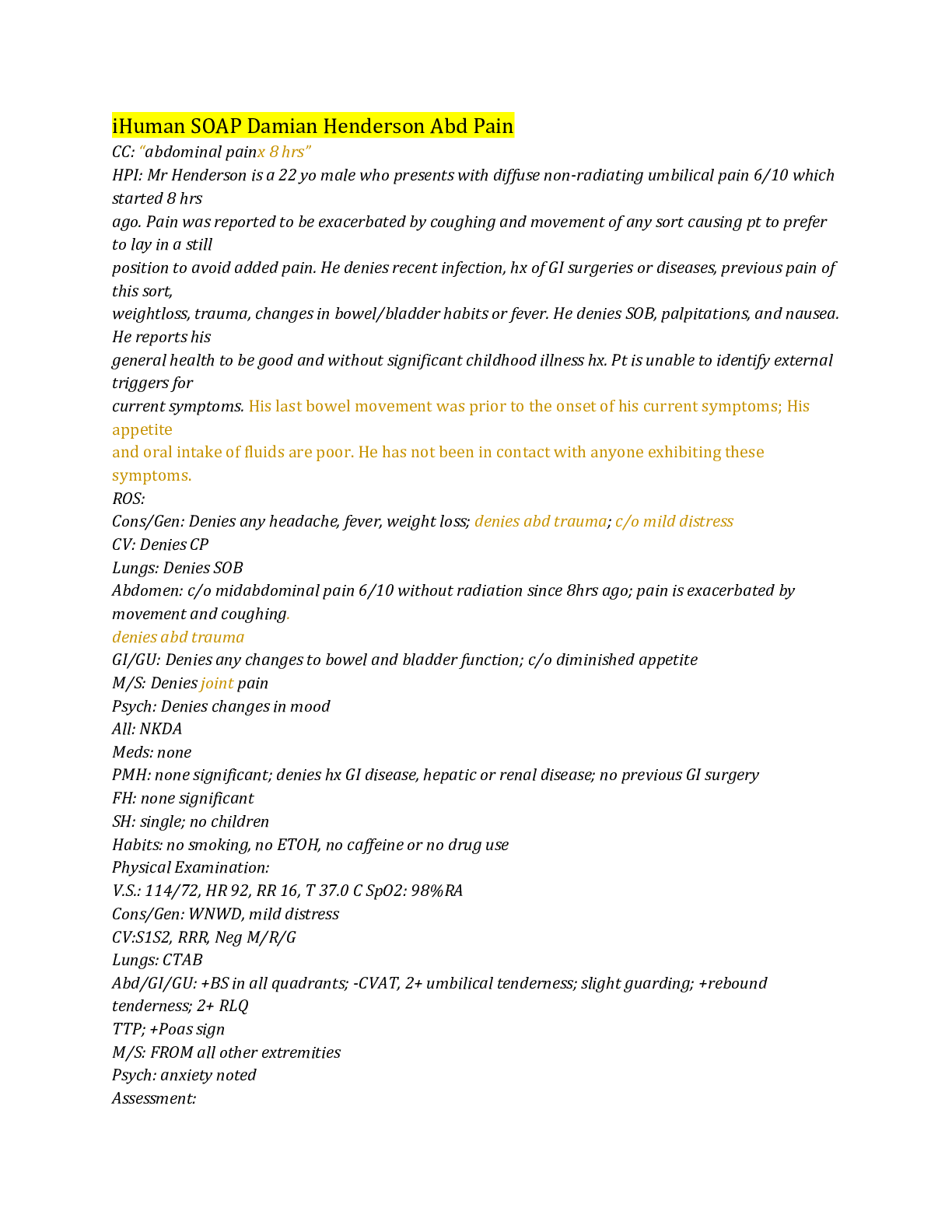
NURS 6541 Pediatric Soap Note/PRIMARY CARE OF ADOLESCENTS AND CHILDREN
$ 6
 (Q&A).png)
CSO-001 (CYSA+)
$ 50
eBook [PDF] Ethics in Health Administration A Practical Approach for Decision Makers 4th Edition By Eileen Morrison
$ 30

GCE Further Mathematics A Y541/01: Pure Core 2 Advanced GCE Mark Scheme for Autumn 2021
$ 6.5
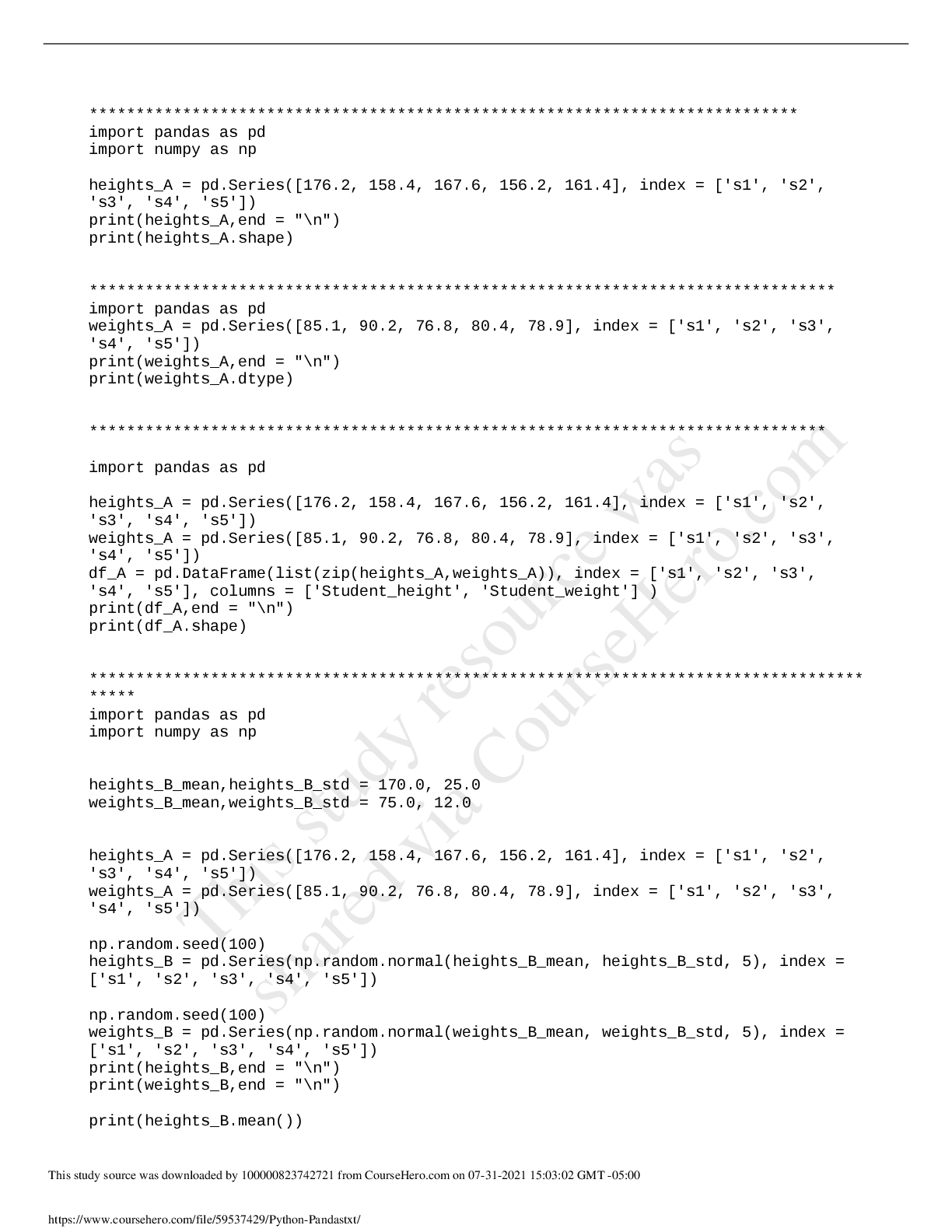
Python programming. Easier and understandable way
$ 10
NR-293 Week 7 Discussion: Unfolding Case Study (GRADED A)
$ 5
Beckmann and Ling’s Obstetrics and Gynecology ( PDFDrive )
$ 16
ATI Learning System RN 3.0-Medical-Surgical Immune and Infectious Practice Questions & Answers-Updated for 2023 Pass Medical-Surgical Immune and Infectious in First Attempt Guaranteed!Get 100% Latest Exam Questions, Accurate & Verified Answers to Pass the Actual Exam! Instant Download!
$ 15.5

ECET-105 Week 3 Lab Introduction to Digital Logic Gates (VERSION 2) With Latest Updated Solutions
$ 10

MGMT 404 Course Project: Getta Byte Software Project - Part 1
$ 55
ITM 215: Excel Introduction to Excel
$ 18
TESTOUT LINUX PRO EXAM QUESTIONS AND ANSWERS 2024 GRADED A
$ 18.5
A-level BIOLOGY 7402/2 Paper 2 Mark scheme June 2022 Version: 1.0 Final
$ 9
THE PURPOSE OF COLLEGE: JOB OR KNOWLEDGE University Canada West RSCH 600 complete research
$ 11
AQA AS PHYSICS 74071 PAPER 1 MARK SCHEME JUNE 2022 VERSION 1.0 FINAL