NR 601 Week 8 exam Study guide
Week Topics
Concept: endocrine
5 Glucose metabolism disorders
Types of diabetes (prediabetes, type 1 and type 2)
risk factors: most common ethnicity- caucasian, native american, Alaska
...
NR 601 Week 8 exam Study guide
Week Topics
Concept: endocrine
5 Glucose metabolism disorders
Types of diabetes (prediabetes, type 1 and type 2)
risk factors: most common ethnicity- caucasian, native american, Alaskan native men
and women.
Diagnostic criteria- FPG ≥126 mg/dL (7.0 mmol/L). Fasting is defined as no caloric
intake for at least 8 h.*
2-h PG ≥200 mg/dL (11.1 mmol/L) during OGTT. The test should be performed
as described by the WHO, using a glucose load containing the equivalent of 75-g
anhydrous glucose dissolved in water.*
A1C ≥6.5% (48 mmol/mol). The test should be performed in a laboratory using a
method that is NGSP certified and standardized to the DCCT assay.*
In a patient with classic symptoms of hyperglycemia or hyperglycemic crisis, a
random plasma glucose ≥200 mg/dL (11.1 mmol/L).
Initial treatment recommendations- first line treatment for each type
Type 1- insulin
Type 2- 1st line-lifestyle change, metformin
o common medication side effects- n/v/d/abd pain/anorexia/taste disturbancv
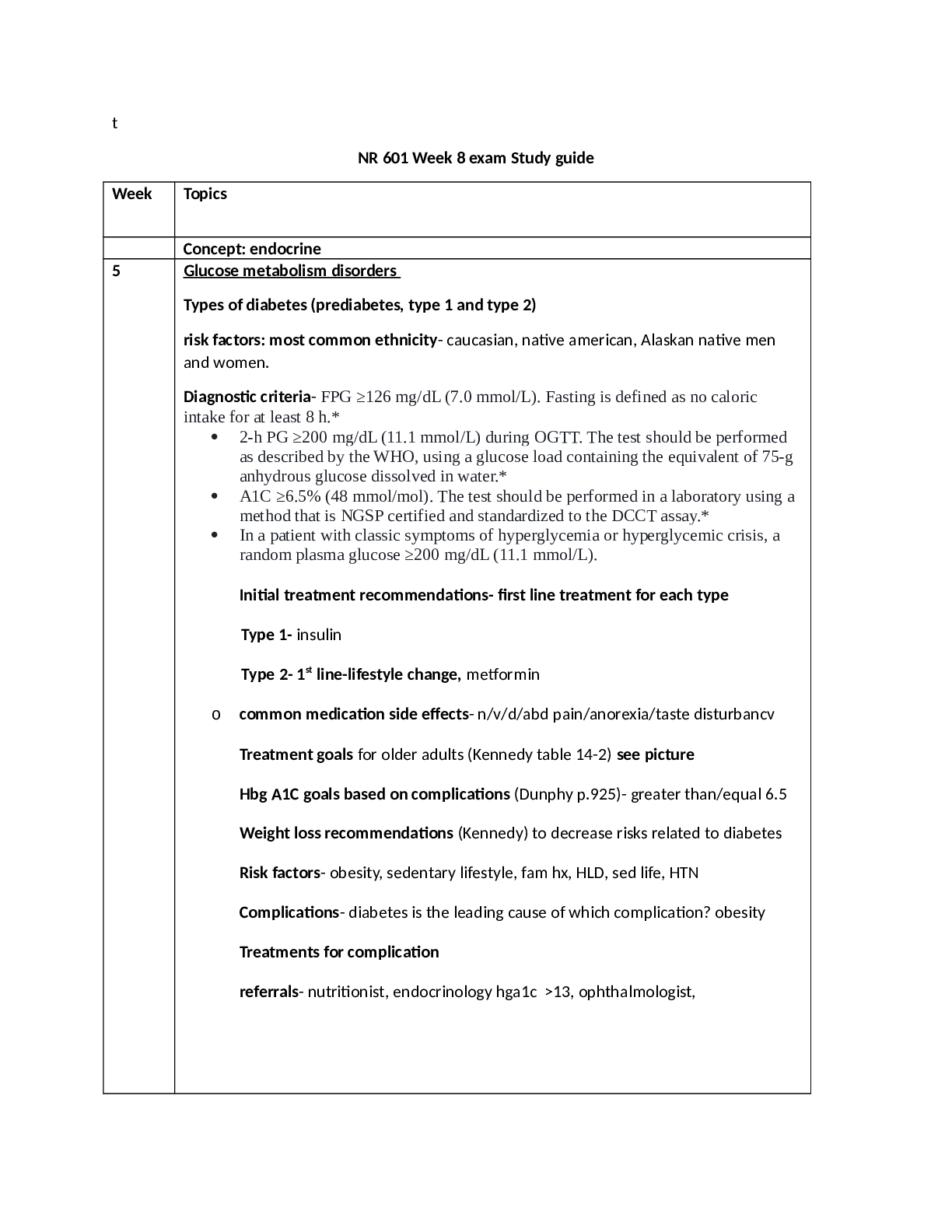
Treatment goals for older adults (Kennedy table 14-2) see picture
Hbg A1C goals based on complications (Dunphy p.925)- greater than/equal 6.5
Weight loss recommendations (Kennedy) to decrease risks related to diabetes
Risk factors- obesity, sedentary lifestyle, fam hx, HLD, sed life, HTN
Complications- diabetes is the leading cause of which complication? obesity
Treatments for complication
referrals- nutritionist, endocrinology hga1c >13, ophthalmologist,Obesity
Comorbidities related to obesity- CAD, HTN, HLD, DM, CVA, central obesity
(abd), metabolic syndrome,osa, osteo, breast/colon/endometrial ca, kidney, liver,
esophagus, gastric, pancreatic, gallbladder, leukemia, dementia, ckd
o BMI classifications (Kennedy) see picture
6 Urology and aging (Kennedy)
Urinary incontinenceInvoluntary loss of urine from the bladder
▪ So common in women many consider it normal
▪ Common in older men w/ enlarged prostate
o Can affect quality of life
o Significance-One of the most common complains w/ older adults, Distress &
embarrassment, Cost burden to pt & society as a whole, Not life-threatening, may effect
QOL, PCP essential to educating individuals
o Epidemiology- Increased prevalence w/ age in men & women, Nursing home
population – 40-70%, Often a factor in placement
▪ URGENCY UI is greater in men
▪ STRESS UI is greater in women
o Terminology
▪ UI- Unintentional voiding, loss or leakage of urine
▪ Continuous incontinence-Continuous loss or leak of urine
▪ Increased daytime frequency-More frequent during day than considered normal
▪ Nocturia-Interruption of sleep one or more times due to the need to urinate – increases in
frequency after age 50
▪ Urgency-Sudden, compelling desire to pass urine that’s difficult to prevent
▪ Overactive bladder syndrome- Urgency, frequency, nocturia w/ or w/o incontinence
o Risk Factors-Aging,Obesity,Smoking, Caffeine,Uncontrolled DM, Constipation,Use of
diuretics
o Risk Factors by gender-Women:Aging, obesity, smoking, caffeine intake, DM,
pregnancy, multiparity, estrogen deficiency, hx of pelvic surgery, diuretics
Men:Aging, obesity, smoking, caffeine, DM, prostate dx, hx of prostate surgery, hx of
UTIs, diureticso Physical changes w/ aging that contribute to UI
▪ Lower urinary tract-Detrusor muscle over activity,Decrease in detrusor contractility,
Increase in post void residual,Decrease in urethral blood flow
▪ Women – decrease in urethral closure pressure,Low estrogen following menopause -
leads to atrophy of ureteral mucosal epithelium & increase in urethral sensation
▪ Men can experience constriction of urethra due to BPH which may result in bladder
outlet obstructing symptoms
- Initial clinical workup for UI in Men
o PMH, PE, UA, DRE: Eval of prostate, PSA w/ new onset in men
- UI workup in women: Exclude underlying causes, PMH, PE, UA, Pelvic exam, vaginal
exam, perineal, Identify estrogen status of pt, Pelvic prolapse, fistula,
-Cough test, Integrity of pelvic musculature, leaking of urine
▪ Full bladder
▪ Standing position
▪ Asked to cough
▪ If urine leak is observed, stress incontinence is confirmed
- Red flags in males
o Higher level of suspicion for serious diseases, Refer to urology if Previous pelvic
surgery, Pelvic radiation, Pelvic pain, Severe incontinence, Severe UTI symptoms,
Recurrent urologic infection,Abnl Prostate exam,Elevated PSA
o Be alert to these with NEW ONSET UI- Hematuria,Pelvic pain,Abdominal mass,
Dysuria, Proteinuria, Glucosuria, CVA tenderness,Nodular prostate,Any new neuro
symptoms
- Goals of treatment: Reduce symptoms, Improve QOL, Increase social activity, Reduce
leakage volumes, increase dryness, use less protection; Increase independence in
incontinence management; Decrease caregiver burden
lower urinary tract symptomso frequency, pain on urination or pain increasing with uriuiation.
Acute bacterial prostatitiso presence of more than 10 WBC per high power field on mid stream urine
collection.
If acutely ill, hospitalization.
o Treat with Cipro 500mg BID x 10 days or Levaquin 500mg daily x 10
days.
o Choose a fluoquinolone - it penetrates prostate tissue well.
Education
o May need a stool softener. Repeat UA is recommended. Avoid anal
intercourse. Use condom to prevent reintroduction of bacteria intourethra.
- 1st line management guidelines
o AHRQ guidelines for management of UI in women
▪ Behavioral therapy
▪ Lifestyle modification
▪ Try for 3 months before pharm management
o Weight loss, Smoking cessation(Tobacco is a bladder irritant),Less coughing
o Dietary changes-Alcohol, soda, coffee with or without caffeine, acidic foods and spicy
foods
o Maintain adequate fluid balance to reduce constipation, provide adequate flow to
kidneys
- Behavioral strategies:Bladder training, Bladder control strategies,Timed voiding,Kegels,
Pelvic floor training
- 2nd line management - Medication
o Antimuscarinic medication: 1st line for women
▪ Block the parasympathetic muscarinic receptors
▪ Inhibit involuntary detrusor contractions
▪ Side effects due to the effects on other muscarinic receptors
o Outcomes unpredictable and side effects common
o Common s/e: Dry mouth**, Blurred vision, Constipation,Nausea,Dizziness, Headache
o AntimuscarinicsMechanism of action
● Blocks acetylcholine at muscarinic receptors, relaxes bladder smooth muscle, inhibits
involuntary detrusor contractions (anticholinergic)
● CYP3A4 substrates
▪ Indications: UI and OAB
▪ Contraindications: Untreated/uncontrolled narrow angle glaucoma,Gastric retention,
Urinary retention
▪ Precautions:CNS depression,Caution in elderly
● Renal dosing
o CrCl <30
o Beta 3 Adrenergic Agonist – Mirabegron (Myrbetriq)
▪ Also approved for UI and OAB▪ Clinical trials – significant reduction in incontinence and micturations
● No anticholinergic s/e
▪ Mech of action
● Selectively stimulates beta-3 adrenergic receptors
● Relaxes smooth muscle – bladder
▪ Contraindications/caution: HTN- Do not use if SBP >180, DBP >100
▪ Avoid severe renal/liver disease
▪ Dose – 25-50mg PO QD
▪ CrCl <30 – max 25mg
- 2nd line of UI in Males – Alpha 1 blockers
o Men, not women!
o Alpha 1 blockers antagonize peripheral alpha 1 adrenergic receptors
o Used in men d/t high incidence of BPH in aging men
o Alpha antagonists
▪ Alpha 1A – prostatic smooth muscle relaxation
▪ 1B – vascular smooth muscle contraction
▪ 1D – bladder muscle contraction and sacral spinal cord innervation
o Meds
▪ Doxazosin SE: Dizziness, dyspnea, edema, fatigue, somnolence
▪ Terazosin SE: Asthenia, dizziness, postural hypotension
▪ Tamsulosin SE:Abnormal ejaculation, asthenia, back pain, dizziness, increased cough
▪ Alfuzosin- CrCl <30 use with caution, SE: Dizziness, URI
▪ Silodosin SE- Retrograde ejaculationUTI risk factors, differences based on gender -
Aging,Obesity,Smoking, Caffeine,Uncontrolled DM, Constipation,Use of diuretics
female- bacteria in urethra, bladder, chronic inflammation (interstitial cystitis), age, sex,
suppressed immune system, pregnancy, urinary obstruction, neurogenic bladder, DM,
f/c, urethral obstruct, obesity, smoking, caffeine intake, DM, pregnancy, multiparity,
estrogen deficiency, hx of pelvic surgery, diuretics, decrease in urethral closure
pressure,Low estrogen following menopause - leads to atrophy of ureteral mucosal
epithelium & increase in urethral sensation
Men- prostate issues, prostatitis, f/c, uti, unprotected anal sex, Men:Aging, obesity,
smoking, caffeine, DM, prostate dx, hx of prostate surgery, hx of UTIs, diuretics, obesity,UTI pathophysiology- common bacterial causes – women- 1st cause gram neg
rod (e-coli), 2nd cause- gram pos coccus-staph saprophyticus, proteus mirabilis,
klebsiella, Enterobacter, serratia, pseuomonas, staph aureus, fungi (candida)
o UTI diagnostic criteria and when to treat (review week 6 discussion and know
criteria for treatment based on symptomatic and asymptomatic bacteriuria
o medications
o complications of untreated urinary tract infection
o Incontinence – involuntary loss of urine from bladder, common in women,
older men with enlarged prostate
risk factors- infection, delirium, meds, DM, fecal impaction,
restricted mobility
types of incontinence -stress, urge, overflow (not empty
bladder), functional (delirium, fecal impact, dec mobility, meds)
o Causes of hematuria and proteinuriahematuria- food, caffeine, spices, tomatoes, chocolate, alcohol, citrus, soy sauce,
herbal med, beta-lacam abx, sulfonamides, nsaids, warfarin, heparin, aspirin,
Dilantin, cipro, allopurinol, Tagamet, urolithiasis, menses. For men >50 needs
workup
Proteinuria- illness, stress, exercise, fever, chf, acute pulm eema, cva, head
injury, mult myeloma, lymphosarcoma, leukemia, hodgkins, albumin transfusion,
o urologic changes in the male and female
[Show More]