*NURSING > STUDY GUIDE > NURS 303 Med surg final exam study guide; A+ guide. (All)
NURS 303 Med surg final exam study guide; A+ guide.
Document Content and Description Below
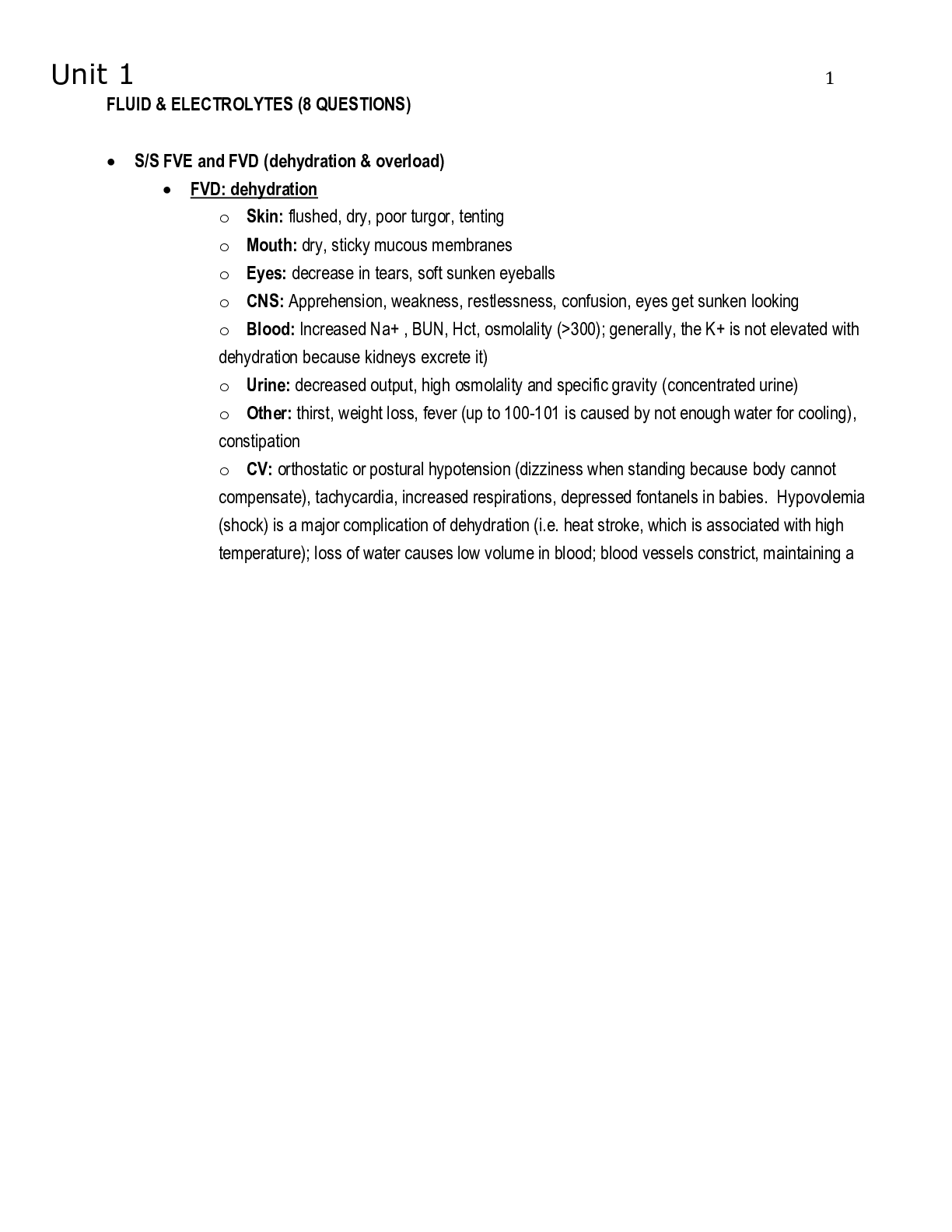
FLUID & ELECTROLYTES (8 QUESTIONS) • S/S FVE and FVD (dehydration & overload) • FVD: dehydration o Skin: flushed, dry, poor turgor, tenting o Mouth: dry, sticky mucous membranes o Eyes: dec ... rease in tears, soft sunken eyeballs o CNS: Apprehension, weakness, restlessness, confusion, eyes get sunken looking o Blood: Increased Na+ , BUN, Hct, osmolality (>300); generally, the K+ is not elevated with dehydration because kidneys excrete it) o Urine: decreased output, high osmolality and specific gravity (concentrated urine) o Other: thirst, weight loss, fever (up to 100-101 is caused by not enough water for cooling), constipation o CV: orthostatic or postural hypotension (dizziness when standing because body cannot compensate), tachycardia, increased respirations, depressed fontanels in babies. Hypovolemia (shock) is a major complication of dehydration (i.e. heat stroke, which is associated with high temperature); loss of water causes low volume in blood; blood vessels constrict, maintaining a low normal BP (controlled by baroreceptors); heart rate increases to make up for low volume. If a person is exposed to excess heat, maintaining a constant temperature is a good outcome. . o HYpovolemia; heart rate increases to make up for low volume – sx; tachycardia, low BP, increased respirations • FVE: o Lab - decreased: Na+ (dilutional), low Hematocrit, sp. gr., osmolality o Skin: Dependent edema (tight, cool, shiny, pale skin) o Respiratory- pulmonary edema, Shortness Of Breath (SOB), cough, crackles, increased respirations, frothy sputum o CNS: Lethargy, confusion, convulsions (due to increased ICP), coma o GI: anorexia, N/V o Blood: dec. Na+, Hct, low osmolality, dec. BUN o Urine: decreased in relation to intake, decreased osmolality and SG – the reason you become fluid overloaded so daily weights the best way to determine fluid balance o Other: sudden weight gain (>5% TBW = puffy); anasarca = generalized edema. Daily weights are the best way to determine fluid balance. Much better than I & • Identify s/s by category: Isotonic, Hypertonic, hypotonic • Isotonic Volume Deficit: same as above; lab work is normal • Hypotonic Volume Excess: what is listed above • Isotonic Volume Excess: Signs and symptoms- same; except lab values will be WNL – distended neck veins, increased BP, edema (pulmonary, peripheral, organ), hepatomegaly (enlarged liver) • Specific types of Edema: • Edema caused by increased hydrostatic pressure in blood that causes fluid to shift into tissues o Pitting edema aka ankle or dependent edema (CHF; in pregnancy caused by increased hydrostatic pressure of baby on venous return from legs); treatment with diuretics, fluid restriction, elevation of legs, sodium restriction, etc; everyone with CHF and hypertension should be on low sodium diet. Remove the water pitcher and salt shaker; having ankle edema after sleeping all night is a sign of CHF o Pulmonary edema aka CHF, crackles- lasix, oxygen, HOB up – not pushing out of left ventricle it backs up in right atrium o Ascites (cirrhosis, 3rd spacing)- scarring in liver prevents portal blood from going into liver, this increases the hydrostatic pressure in portal circulation and fluid collects; paracentesis is done to remove fluid – circulation that goes around intestines and into liver is portal transport – cirrhosis (liver all scarred up) the BV can’t enter the liver so they get backed up and water diffuses out o DVT and blockage of venous system can cause increased hydrostatic pressure and leg edema • Edema caused by: electrolyte imbalance o Cerebral edema caused by hyponatremia-(fluid shifts from blood into brain); treated with steroids, mannitol or 3% Saline, seizure precautions; a stroke causes inflammation and swelling and cerebral edema (from a clot); excessive use of D5W without sodium can cause hyponatremia and cerebral edema. Severe hyponatremia is usually seen with SIADH • Edema caused by: Low Protein o Non-pitting or brawny edema often caused by low albumin- same treatment, + increased protein in diet; seen in malnourished or burn victims; usually seen in the legs- can be anasarca (all over the body) • Edema caused by: lymphatic problems o Lymphedema caused by removal of lymphatics- elevate the body part; sometimes bed is elevated on blocks to keep from bending vessels o Primary lymphedema- congenitally missing lymphatic system o Edema from low protein malnourished patients aka brawny edema – can’t pull water back into his tissues • IVF Chart: what fluids belong in each category, patients that are appropriate or inappropriate for each category, what each fluid is typically used for • Hypertonic: o D51/2NS: (5% Dextrose and .45% NS): draws fluid into vasculature from interstitial and intracellular compartments, hypertonic when infusing but becomes hypo when dextrose is metabolized so commonly used for hydration o 3% NS: prevents seizures from severe hyponatremia, only used when risk of seizures from brain edema; monitor for pulmonary edema; Excess ADH production (SIADH) causes water retention, hyponatremia, and cerebral edema when serum sodium is <120, at risk for seizures o D5LR (5% Dextrose and Lactated Ringers): electrolyte formula used for patients with draining wounds o D5NS: provides calories to prevent catabolism when NPO o D10/W: persistent hypoglycemic episodes, used to taper off TPN o Dextrose 50%; tx single episode of hypoglycemia • Hypotonic: o .45% NS: treats cellular dehydration, promotes waste elimination by kidneys, for dehydration IF BP is adequate, monitor adults for confusion with administration • Isotonic: o Lactated Ringers; balanced electrolyte formula (commonly used for surgical patients), caution in use with renal patients bc contains potassium, lactated: helps reverse acidosis after surgery o 0.9% NS: used for vascular volume expansion and fluid resuscitation, stays in blood and is used for SHOCK, common in ER and for BP elevation o 5% Dextrose: D5W; becomes free water when dextrose metabolizes, expands intracellular and interstitial fluids, short term only!! – eventually cause low serum sodium b/c gets “washed out” and RBCs will lyse. Pt will get edema to brain and have seizures • Plasma expanders o Patho- Unlike crystalloids, colloids contain molecules too large to pass through semipermeable membranes, such as capillary walls. Because they remain in the intravascular compartment, they're also known as volume ex¬panders or plasma expanders; last longer than crystalloids. Ex¬amples include albumin, dextrans, and hydroxyethylstarches. Colloids expand intravascular vol¬ume by drawing fluid from the inter¬stitial spaces into the intravascular compartment through their higher oncotic pressure; have the same effect as hypertonic crystalloids of increasing intravascular volume, but require administration of less total volume compared with crystalloids. Colloids are indicated for patients exhibiting hypoproteinemia, and malnourished states, as well as for those who re¬quire plasma volume expansion but who can't tolerate large infusions of fluid. Interfere with platelet function. o Five percent albumin (Human albu¬min solution) is one of the most com¬monly utilized colloid solutions. It contains plasma protein fractions obtained from human plasma and works to rapidly expand the plasma volume; used for volume expan¬sion, moderate protein replacement, and achievement of hemodynamic stability in shock states. Albumin is also available in a 25% solution, which is much more hypertonic and can draw about four times its volume from the interstitial fluid into the vascular compartment within 15 minutes of administration. Albumin pulls fluid into intravascular space; low albumin in a patient causes decreased colloid osmotic pressure and fluid remains in the interstitial space as edema which can be pulmonary edema. Albumin is contraindicated in patients with the following conditions: severe anemia, heart failure, or a known sensitivity to albumin. o Synthetic colloid preparations are available for patient use to draw water into the intravascular space. LMWD (Low-molecular weight dextran) contains polysaccharide molecules that behave like colloids with an average molecular weight of 40,000 (dextran 40). It contains no electrolytes and is used for volume expansion and support. LMWD is used for early fluid replacement and to treat shock related to vascular vol¬ume loss, such as that produced by burns, hemorrhage, surgery, or trau¬ma. It's used to prevent venous thromboembolism during surgical procedures, because its mechanism of action is to prevent the sludging of blood. LMWD is contraindicated in patients with thrombocytopenia, hypofibrinogenemia, and hypersensitivity to dextran. HMWD contains polysaccharide molecules with an average molecular weight of 70,000 (available as dex¬tran 70) or 75,000 (available as dex¬tran 75). It also contains no electro¬lytes. HMWD shouldn't be given to patients in hemorrhagic shock. Hydroxyethalstarches, such as heta-starch (6%) and hespan, are another form of hypertonic synthetic colloids used for volume expansion. They contain 154 mEq/L of sodium and chloride and are used for hemody¬namic volume replacement following major surgery and to treat major burns. Synthetic colloid preparations are less expensive than albumin and their effects can last 24 to 36 hours. Hetastarch is contra-indicated in patients with liver dis¬ease and severe cardiac and renal disorders. It may also cause a severe anaphylactoid reaction. • TPN nursing actions • one large bag hung in the evening 6/7pm; hang at time ordered and discard extra solution in old bag • Patient must have blood sugar monitoring every 6 hours, even if not diabetic • Goal is weight gain of 2 lbs per week (nutrition gain; not fluid gain) and normal albumin level (3-5) • If for any reason the parenteral solution is not available, the nurse needs to hang D 10 W at the same rate as the ordered parenteral nutrition. This is because the patient’s body is producing lots of insulin to handle the sugar load from the TPN, and stopping the TPN suddenly may cause hypoglycemia. The physician MUST be contacted and made aware that the parenteral nutrition is not infusing for any reason. This includes electrolyte imbalances; loss of intravenous access site, orders not getting to the pharmacy on time. • 2 nurse check (PINCH drug), new tubing hung with each new bag • Two nurses MUST check the parenteral nutrition bag label against the current parenteral nutrition order comparing each additive with the reference values provided and the patient’s lab values. If the solution is correct, both nurses MUST sign the appropriate sections of the order form, the MAR, and initial the bag prior to beginning infusion. • Standard hang time is 1800 hours at most hospitals. It used to be delivered and hung at 0800, but then the MDs would make rounds and change the composition and the bag would be discarded (i.e because it had too much potassium and the patient’s level was high). Now it is ordered or adjusted in the morning and delivered in the afternoon and hung at 1800 or 1900. Any unused solution is discarded after 24 hours. Tubing for TPN must be changed daily with the new bag of solution). • Administration o Must give through central line because of osmolarity. The highest concentration that can be given peripherally is D10W. Higher than that causes sclerosis and vein damage; this stuff is at least 25% Dextrose • S/S of electrolytes; hyper and hypo • Hyponatremia: normal 135-145 o result when BP drops or fluid shifts to IC space; severe hyponatremia (<115) causes muscle twitching and tremors, focal weakness, seizures, signs of increasing ICP, coma) o a) Tissues= edema (brain edema= disorientation, coma, twitching, seizures) o b) CV- low Na+ = low vascular volume= hypotension • Hypernatremia: o dry & sticky mucous membranes and dry tongue o flushed appearance, weakness o thirst, oliguria o elevated temp o irritability, disorientation, seizures, stupor, coma • Hypokalemia (3.5-5) o N/V; anorexia from decreased muscle activity in smooth muscle (paralytic ileus), distention from accumulated gas o EKG changes, cardiac arrest; low K+ potentiates digoxin (heart picks up on digoxin); pulse may become irregular o muscle weakness (paresis), poor muscle tone, fatigue; leg pains (persons with leg cramps should have K+ checked- high or low can cause pain) o parathesia- numbness • Hyperkalemia o oliguria (this is a cause, not a symptom), if patients have oliguria, nurse should question orders for potassium in IV fluids because patient may have renal failure o intestinal colic (cramps), diarrhea o EKG changes (peaked T waves), cardiac irregularities or cardiac arrest o Muscle twitching, irritability • ** calcium phosphate (calcium levels are regulated by PTH and calcitonin) • calcitonin released when calcium is too high normal level of calcium is 8-10 mg and normal level of phosphate is 2.5% - 4. • Hypocalcemia/hyperphosphatemia o Sudden drops-overexcitability of NM= tingling of fingers and around the mouth, tetany, muscle spasms, respiratory arrest. Respiratory alkalosis (hyperventilation) can cause a sudden drop Trousseau's sign-(inflate BP cuff 2-3 minutes = hand flexes) * changes acid base balance when you put the cuff on Chvostek's sign- (tap facial nerve, lip contracts) * muscles are real twitchy when calcium is low o Tx-oral Ca++ and Vit D; calcium gluconate IV for tetany; seizure precautions o Long term – pathological fractures (can be caused by lack of weight-bearing on long bones – long term immobility • Hypercalcemia/hypophosphatemia o GI disturbances, mental confusion, stones – tend to have symptoms of dehydration SURGERY (8 QUESTIONS) • Normal Lab values and what would keep the patient from going to surgery • CBC: Hgb&Hct needs to be >10/30; WBC needs to be normal 5-10,000 (high=infection, low= increased risk for infection); platelets need to be >150,000 or there is risk of bleeding. • Coagulation studies or Liver Function Tests (measure clotting factors made by the liver); PT= Prothrombin Time and PTT is Partial Thromboplastin Time. Prolonged time = increased bleeding; *** • BUN (10-20) & creatinine (1.0) - 0.6 to 1.2 milligrams increases indicate kidney disease • Glucose (100) • Complications • Hypovolemia – loss of blood o Cause- loss of blood= Hypovolemia (decrease in circulating blood volume)= low BP (drop of 20% systolic). When volume drops, the vessels compensate with vasoconstriction which helps maintain a low normal for awhile. When vasoconstriction occurs, the diastolic pressure increases, so there is decreased pulse pressure (difference is systolic and diastolic readings). Example: 130/70 becomes 120/90. When the vessels are maximally vasoconstricted and the volume is too low to maintain low normal BP, the patient goes into irreversible shock (death). • Symptoms (usually bleeding is internal and not evident on dressing) o Increased pulse rate – weak, thready; Increased respirations; decreased BP o Oliguria- less blood goes to kidneys due to vasoconstriction, so output drops o Pale, cool moist skin- vasoconstriction causes pale color (cold, clammy) o Restlessness- caused by decreased oxygenation of tissues • TX; Trendlenburg position (first!) or supine with feet elevated, increase IV fluids, call doctor, give transfusion, give whole blood if massive hemorrhage. • Malignant hyperthermia (rapid rise in temp, may be fatal) – in PACU o Cause- triggered by anesthetic or NM paralytics; usually temperature is low in the OR so even a slight elevation is bothersome; can occur intraop or immediately postop; Genetic autosomal dominant trait that triggers muscle metabolism error; asking about relatives having surgery is part of pre-op assessment for this reason Rapid releases of calcium ions triggers elevated metabolic rate and hyperthermia o Symptoms Tachycardia is first; hyperthermia is later Muscle rigidity, respiratory and metabolic acidosis and cell death Hypercalcemia, hyperkalemia, hyperphosphatemia, and CPK rapid rise in temp (it can be as fast as 1 degree every 5 min) o Treatment - Goal is to correct acidosis, dysrhythmias, electrolyte imbalances C-V support (meds; monitoring) Surgery is stopped Dantrolene, skeletal muscle relaxant Sodium bicarb for lactic acidosis Chilled saline IV and NG lavage Ice packs or hypothermia blanket Insert Foley catheter Stat labs (electrolytes) • Dehiscence and evisceration o poor wound healing due to excess fat, especially if incision is very large i.e. colon resection. Ruptured bowel (from appendix or diverticuli) are more likely to abscess and get infected and have longer wound healing and dehiscence; patients having any kind of abdominal surgery (including hysterectomy) should not do any lifting for several months. o Sx; (protrusion of subcutaneous fat) or evisceration (protrusion of viscera or intestines); patient may sneeze and feel something pop o Tx; Place patient on bedrest, Cover site with sterile saline dressing (exposure to air causes drying and adhesions later), Take VS- risk of shock, Call Surgeon, OR • Ileus o Cause: intestines stop peristalsis, exposure of intestines to air,manipulation, anesthesia paralysis; narcotics o SX; no bowel sounds, N/V, no gas, abdominal discomfort, pain o Tx; ambulate, Mylicon, no straws, NG tube (will be removed when bowel sounds are present, patient is passing gas, patient has no N/V, drainage is minimal- less than 100/shift). The most important of these is active bowel sounds. Patient will have to get IV fluids to keep pt hydrated while he has the NG tube. An ileus is different from a small bowel obstruction. When someone has a SBO, an NG tube is inserted and removed when patient is passing gas or has a BM. Most surgery patients don’t have BMs because they have been prepped before surgery with enemas, etc. o NGT and when it would be indicated to be put in or come out will be removed when bowel sounds are present, patient is passing gas, patient has no N/V, drainage is minimal- less than 100/shift o Nursing care of an NGT Check position- make sure that only 1 or 2 of the black marking lines are showing- otherwise it needs to be untaped and pushed in further (but only for colon surgery, not gastric surgery) and re-taped. If no drainage, irrigate with NS only and aspirate it out if possible; never push NS or water down the blue air port Feeding tubes are very flexible and sometimes get in the wrong place and need to have their position checked (by aspirating contents and checking pH or pushing in air and listening for gurgle)- NG tubes are too big and stiff to get coiled up in the lung so this is not really necessary o Patient teaching in prevention Early ambulation Fluid intake of 2500-3500 mL • Consent • Who can and can’t give consent o Person must be mentally and physically competent (may need legal hearing to be declared incompetent); psychiatric patients are not automatically incompetent (if a patient can understand what is going to be done, then he/she is competent to sign); not legal if patient is confused, in a great deal of pain, sedated (alcohol or pain medication within 4 hours) o Must be of age (18) or be an emancipated minor (married, earning own living; this is awarded by court). A 16 year old girl with a baby is legally permitted to give consent for treatment of her child and her pregnancy, but the girl’s parent would have to give consent for her to have other surgery. o An adolescent is emancipated when married after getting a court order. However: A minor cannot get married without parental consent. A minor under 16 years old cannot get married even with parental consent. A court can allow marriage with parental consent if the couple is under 16 years old but have (or are expecting) a child together. o Be legal next of kin or surrogate designated by the client • When can we not get consent from a patient? o In emergency, MD may act to save life, BUT every effort must be made to contact person by telephone, telegram, fax or other electronic means; if pt is unconscious and no one is available the MD may operate without consent. DIABETES (5 Questions) • Risk factors and causes of Type 1 & 2 • Type 2 Risk factors; o a positive family hx, obesity (90%) and physical inactivity, race/ethnicity, HTN, high cholesterol, high triglycerides. Obesity decreases sensitivity of tissues to insulin, and as a Continues.>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>> [Show More]
Last updated: 3 years ago
Preview 1 out of 47 pages
Buy this document to get the full access instantly
Instant Download Access after purchase
Buy NowInstant download
We Accept:

Reviews( 0 )
$15.00
Can't find what you want? Try our AI powered Search
Document information
Connected school, study & course
About the document
Uploaded On
Feb 22, 2021
Number of pages
47
Written in
All
Additional information
This document has been written for:
Uploaded
Feb 22, 2021
Downloads
0
Views
89