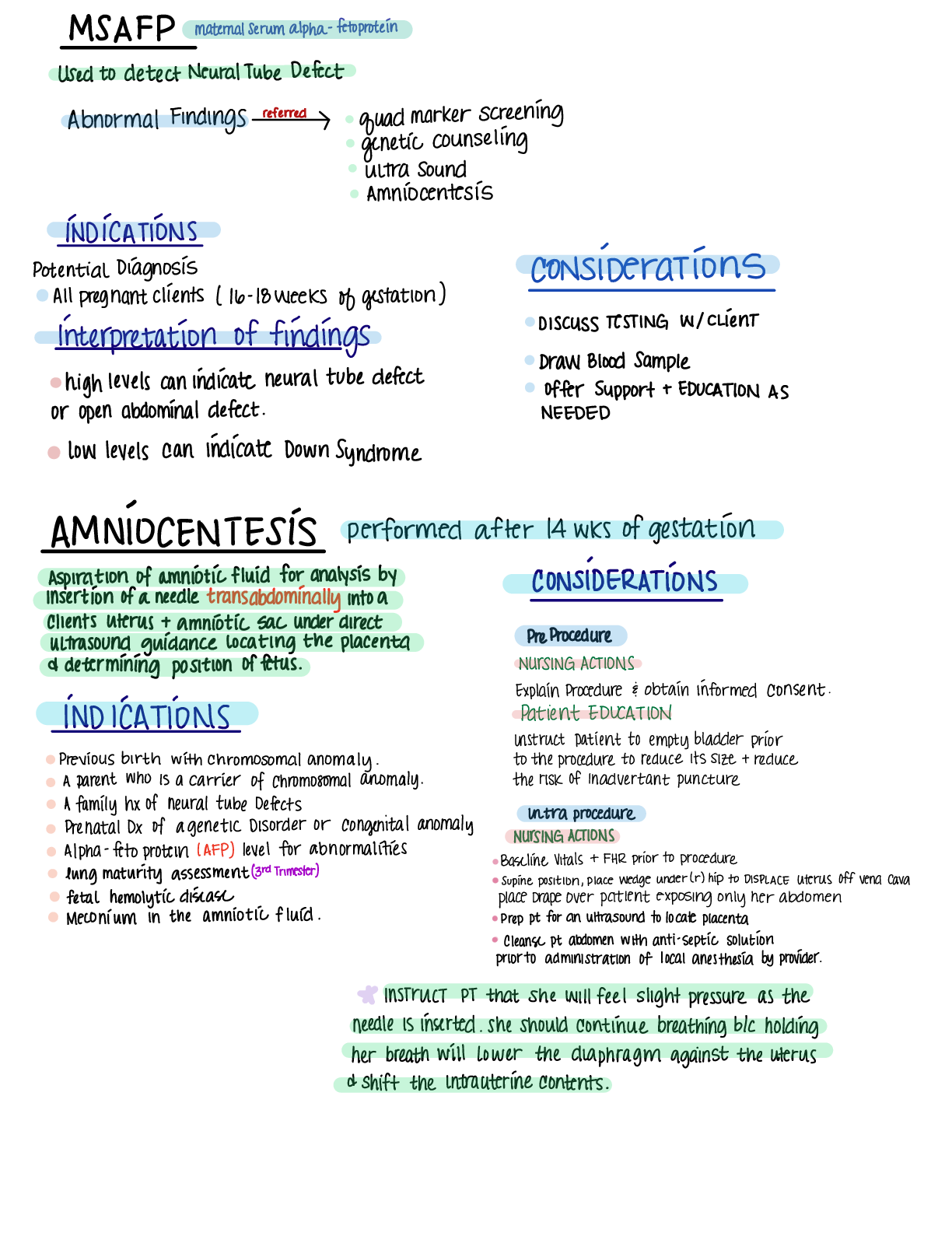
M 13 maternal serumalphaGto protein
UsedtodetectNeural TubeDefect
AbnormalFindings referre dy quadmarkerscreening
geneticcounseling
ultrasound
Amniocentesis
INDICATIONS
potential Diagnosis CONSIDERATIONS
Allpregn
...
M 13 maternal serumalphaGto protein
UsedtodetectNeural TubeDefect
AbnormalFindings referre dy quadmarkerscreening
geneticcounseling
ultrasound
Amniocentesis
INDICATIONS
potential Diagnosis CONSIDERATIONS
Allpregnantclients11618Weeksofgestation
Interpretatings DISCUSSITSTINGINlaient
highlevelscanindicateneural tubedefect Draw Offer Blood Support Sample 1 EDUCATIONAS
oropenabdominaldefect NEEDED
101Nlevels canindicateDownSyndrome
AMNIOCENTESIS performed after 14wksofgestation
insertion Aspiration of of aneedle amniotic trans fluid abdominally foranalysis intoby a CONSIDERATIONS
Clientsuterus amnioticsacunderdirect
Ultrasoundguidancelocatingtheplacenta PreProcedure
ddeterminingpositionof fetus NURSINGACTIONS
ExplainProcedure obtaininformedconsent
INDICATIONS PatientEDUCATION
instructpatienttoemptybladderprior
Previousbirthwithchromosomalanomaly totheproceduretoreduceitssize reduce
Aparentwhoisacarrierofchromosomalanomaly theriskofInadvertantpuncture
Afamilyhxofneural tubeDefects intraprocedure
prenatal DXof ageneticDisorderor congenitalAnomaly NursingActions
Alphafetoprotein AFPlevelforabnormalities Baselinevitals EHRprior toprocedure
lungmaturityassessment 3rdtrimester supinepositionplacewedge underahiptoDisplaceuterusoff venacava
fetalhemolyticdisease place Drape overpatientexposingonlyherabdomen
Meconiumintheamnioticfluid prepptforanultrasoundtolocateplacenta
cleanseptabdomenwithanti septicsolution
prior toadministrationoflocal anesthesiabyprovider
INSTRUCTPTthatshe114111 feelslightpressureasthe
needleisinsertedSheshouldcontinuebreathingbcholding
herbreathwilllowerthediaphragmagainsttheuterus
toshifttheIntrauterinecontentsNI NONStressTest
MOSTWidelyusedtechniqueforanti partumevaluation
of fetal Well beingperformedduring3rdtrimester
NONINVASIVEProcedurethatmonitorsresponseofFHR
toFetalmovement
Patientpushesbuttonattachedtothemonitorwhenever
shefeelsfetal movementwhichisthennotedontracing
AllowsNursetoASSESStheFHRInrelationtofetal
movement
INDICATIONI
DISADVANTAGESOFNSI Assessforintactfetal CNSduring
Highrateoffalsenonreactiveresultswfetal movement the3rdTrimester
responsebluntedbysleepcyclesofthefetusfetal Rulingouttheriskforfetaldeath
immaturity maternalmedicationsenicotineuseDisorder 1hClientsWhohaveDMUsedtwiceaweekstarting
at28Weeksto32Weeksofgestation
PATIENTPresentation CONSIDERATIONS
Decreased fetal movement patient Preparation
intrauterinegrowthrestrictions seatpatientinarecliningchairor placeinasemi fowler'sleftlateral
position
Post maturity
Apply CONDUCTIONgeltopatientsabdomen
GestationalDM Applytwobeltstopatientsabdomen attach the
Fitranduterinecontractionmonitors
GestationalHTN
MaternalChronicHypertension ONGOINGCARE
Hxofprevious fetal demise INstructPTtopressthebutton
AdvanceMaternal Age onhandheldeventeachtimeshe
sicklecell Disease feelsthefetusmove
150 immunization
IFthereareNofetal mumtfetussleeping
vibroacousticstimulationsoundsourceusually
laryngealstimulatorcanbeactivatedfor3
interpretationofFindings secondsonthematernal abdomenoverthe
theMSTisinterpretedasreactiveifthe fetal headtoawakenthesleepingfetus
Fitris anormal baselineratewith
moderatevariabilityaccelerates least
151mm 101 minprior to32weeksFor least
bseconds 10secondspriorto32weeks
occurstwoormoretimesduringa20minperiod
NonreactivelustisatestthatDoesnotDemonstrate
leasttwoqualifyingaccelerationsina20min
Window Ifthisisso afurtherassessmentsuch
asacontractionstresstestCstorBPPisindicatedr
BiophysicalProfite BPP INDICATIONI
usesrealtimeultrasoundtoVISUALIZE potential Diagnosis
physical physiologicalcharacteristics nonreactivestresstest
ofthefetusEObserveforfetalbiophysical suspectedoligonydramniosorpolyhydramnios
responsestostimuli ItcombinesFHR supectedFetalhypoxemiaorhypoxia
monitoringnonstress test 5fetalultrasound
clinical manifestations considerations
prematureruptureofmembranes preparethepatientfollowingthe
maternal infections samenursingmanagement
Decreasedfetal movement Principles Asthoscusedforanultrasound
intrauterinegrowthrestriction
interpretations Variables
Bppassesses fetal wellbeingbymeasuring Far
gvariableswithascoreotzforeachnormalfindings reactiveinonstresstest z
eOforeachabnormalfindinggoreachvariable nonreactive 0
Fetal breathingmovements
Total ScoreFindings insomin atteastiepisodeotgrealerthanzosecauration 2
Absentorlessthanzosecauration 0
81010 Normallowriskofchronic arossbodymovements
fetal asphyxia atleast totlexionm3ominez 3bodyorlimbextensions withreturn
lessthan3episodes 0
4 6 tb suspect chronic Fetaltone
fetalasphyxia atleast episode extension unthreturntoflexion2
lowexiensionistexiomlackofflexiomorabsentmovement a
Qualitativeamniotic Fluid volume
Less 4Ab stronglysuspect leastipocketoffiniathatmeasuresatieastuminzperpindicularplanes 2
chronicfetal asphyxia pockets absentorlessthanum0
CSI contrationStressTest
INDICATIONST
NippleStimulation
lightlybrushpalmacrossnippleforzmin High postterm Risk pregnancy Pregnancy gestational Diabetes
whichcausespituitaryglandstoreleaseendogenousoxytocinthen NONreactivestressTest
stoppingnipple stimulationwhenacontractionbegins
Sameprocess repealedaftera5minrest period
OxytocinstimulatedcontractionTest
AKAOxytocinChallengeTest OCT
usedifnipplestimulationdoesntwork
Nadministrationofoxytocintoinduceuterinecontractions
contractionsstartedw oxytocinDifficulttostop
contraindication
placentapreviaVasapreviapretermlabormultiplegestationpreviousclassicalincisionfromcsection1
reducedcervical competencePatientPresentation Nursingconsiderations
DecreasedFetalMovement obtainbaselinevitalsofEHRfetalmovement
IUGR
Post Maturity contractions10to20Min
GestationalDM
Explainproceduretopatient obtaininformedconsent
Gestational HTN
MaternalchronicHTN Complete anassessmentintoartificial stimulation if contractions
HxofFetal Demise
AdvanceMaternal Age ONGOINGCARE
Sicklecell Disease
initiatenipplestimulationifnocontractions
rollanipplebetweenthumb fingers
INTERVENTIONS monitor provideadequaterest periods
forthepatienttoavoidhyperstimulation
Initiate111Oxytocin oftheuterus
ifhyper stimulationoftheuterus
orpretermlaborsoccursDothefollowing Interpretations
monitor forcontractionslastinglonger than90seeor
occurringmorefrequentlyevery2mm NegativeCST1Normal findings
AdministerToco's
asprescribed IndicateIfwithina 10minperiod
Maintainbedrest Duringprocedures IN13uterinecontractionsthereare
observeptfor30mmafterwardtosee thatcontractions nolateDecelerationsoftheFHR
haveceasedEpretermlabor doesnot begin
PositiveCST abnormal findings
consistent persistentlatedecelerations
Huth501ormorecontractions
tM8 suggestiveofuteroplacentalinsufficiency
PotentialforDretermlabor VariableDcel cordcompression
EarlyDcel FetalheadCompression
Basedonthesefindingsthe
provider
Laboror may perform determine acesarian toinduce birthChromosomal Testing
Pages34 35 ATIlookover
Abruptioplacentaepremature
separationofplacentafromtheuterus separationoccurswinksofgestation
usually 3rdtrimester
partial Detacment Leadingcauseofmaternal death1fetal mortality
Complete Detachment
Assessment ExpectedFindings
MaternalHTNchronicorgestational
sudden onset oflocalizeduterine pain
BluntExternalAbdominalTrauma MVAmaternalbattering withDarkredvaginal Bleeding
cocaineHasoconstriction areaofuterinetenderness canbelocalized
Previousabrupt toplacental Ordiffusedover uterus boardlike
CigaretteSmoking contractionswithhypertonicity
prematureruptureofMembranes Fetal Distress
Multifetalpregnancies ClinicalFindingsofhypovolemicShock
Labs Diagnostic Procedure
Hgb Hot Ultrasoundforfetal Wellbeing
coagfactors eplacental assessment
CLOTTINGFactorsInseminatedintravascular coagulation
crossETypematchfor possiblebloodTransfusion Bpptoascertainfetalwellbeing
KleihauerBetketstlusedtodetect fetal blood
inmaternal circulation
patientcenteredcare patientEducation
palpate uterusfortenderness tone provideEmotional support
AssessFHR forpatientandFamily
immediatebirthismanagement
AdministerNfluidsBPproductsEmedicationsasprescribed
Administer028104minutafacemask
monitorinalsobservingfordeclininghemodynamic
status
Continousfetalmonitoring
Assessurinaryoutputomonitor fluidbalanceEItpwgnanc.ly 2ndmost frequentcauseofbleeding
linearlypregnancya leadingcauseof
Abnormalimplantationof a
fertalkedovumoutsidetheuterinecavity Mtrtility
Usually inthefallopiantube
www.hcanresultmatubalrupture EIpectdFI.gs
Causingfetalhemorrhage unilateral stabbingpainelenderness
unthelowerabdominal quadrant
Delayed11102Wks lighter thanusual
Assessment riskfactory orirregularmenses
Scant darkred.orbrownvaginal
Anyfactors thatcompromisetubalpatencySTIsassisted spottingoccurs6108weeks
reproductivetechnologiestubal
surgery contraceptive afterlastnormal menses redvaginal
intrauterineDevice IUD bleedingfrupturehasoccurred
Referredshoulderpaindltbloodinthe
Diagnostic ETherapeuticProcedures peritoneal orphrenunerveaftertubal cavityirrilatingtheacaphragm rupture
Reportofindicationsofshock
such faintness dizzinessrelatedto
Transvaginalultrasoundshowsempty amountofbleedingmabdominal
Uterus Cavity
useCAUTIONIfllaginaldblmanual Clinicalfindingsofhemorrhage shock
examinationareused hypotensiontachycardiapallor
Rapidtreatment
Medical Management ifrupturehasnotoccuredetubepreservationdesired
Methotrexate inhibitscell divisionEembryoenlargementDissolvingthepregnancy
Salpingotomyisotonetosalvagethefallopiantubeifnotruptured
laparoscopicsalpingectomycremovalotthetube isperformedwhenthetubehasruptured
PATIENT CENTERED Care PATIENTEDUCATION
replacetiuideimaintainelectrobiebalance
instructptwnoistaking methotrexate
provideaeducationpsychological support toavoidalcoholconsumption vitaminscontaining
folicaciatopreventatoxicresponsetothe
adminmeasasprescribed medication
Dreppttorsurgeryapostopnursingcare Advisetheclienttoprotect herself from
providereterralforcuinttpartnertopregloss sunexposurephotosensitivity
obtainserumncaanaprogesterone levels liver
renal functionstudiescBc.anatypernPI Previn
OccursWhentheplacentaabnormallyimplantsinthelower segment
oftheuterusnear oroverthecervical OSinsteadofattachingtothefundus
Theabnormalimplantationresultsinbleeding
duringthethirdTrimesterofpregnancyasthe
Arvinbeginstodilateandefface
Assessment
Bsuper
completeortotal thecervicalOSiscompletelycovered previousplacentapremier
bytheplacentalattachment
IncompleteorpartialThecervicalosistheonly uterinescarringpreviouscesarian
partiallycoveredbytheplacentalattachment birthcurettageendometritis
Marginalorlowlying Theplacentaisattached maternal agegreater than35
in theloweruterinesegmentbutdoesnotwalkthe multifetalgestation
cervical OS
multiplegestationsorclosely
spacedpregnancies
ExpectedFindings snoring
painlessBright redvaginalBleedingduringthesecondorthirdtrimester
Uterussoftrelaxed nontenderwithnormal tone
fundal height greater thanusuallyexpectedforgestational age
Fetusinbreechobliqueortransverseposition
ReasuringFAR L yTestN
Vital signswithinnormallimits Hgb and Hot forbloodloss Assessm
Decreaseurinaryoutputcanbebetter indicator
cBc
ofbloodloss
BloodLupe and Rh
coagulationprofile
Kleihauer Betketest
usedtodetectfetalblood in maternal
circulationcontinuePlacentaPrevia PATIENTCENTEREDCARE
DiagnosticProcedure Assessforbleedingleakageorcontractions
Transabdominalontransraginalultrasoundfor
placementoftheplacenta
Assessfundalheight
fetal monitoringforfetal wellbeingassessment PerformLeopoldManeyerslfetalpositione
PATIENTEDUCATION Presentation
BedRest refrainfromperformingvaginalExams
Exacerbatebleeding
NothingInsertedVaginally AdministerIVfluidsbloodproducts tomedications
Asprescribed Corticosteriods betamethasone
promotefetallungmaturationifearlydelivery
isanticipatedIcesarianbirth
Have02equipmentavailableincaseof
fetal distress
ThrombophlebitisEducation ThrombophlebitisPrevention
walking Activity DontSmoke
PromoteActivity Exercise CompressionSocks
EngorgementRelief coldcabbageleauestforfeeding
Displaced uterus full bladder empty
Massagingfondue aftertheDeliveryofplacenta
Babynotreceivingenoughmilk musthave atleat 6 8Mt diapers
Funduslocation12hrumbilicus
14day_fullydescended
rubellateaching
NONimmune APGARscores
NegativebeforeDK
cantbecomePregnantfor4months LF Maynudtomin 1 5min
Normallnfant
36.5 37.6 110 160 30 60 60 80 40 50Rooting helpsencouragefeeding
Infantfeeding Q2hours
SIDSteaching sleeponbacknoextrafirmmattress
CONDUCTION AvoidContactWithColdSurfaces
Circumcision Don'tremove1Touch yellowcrust
Hyperbillrubinemia Poorfeeding
Hypoglycemia Sls Jittery Respiratory difficultyPoorfeeding
carseat rearfacing Anchoredtocar
SKINTOSKIN Bonding CTX feeding Thermoregulation
cord AHA 2arteries Nein
postpartumhems
Methergine prevents controlsPPH improvemuscletonestrengthofcontractions
HighFiberfoodsoatmeallentils Asparagus
Transcutaneous
TENS gffmmugaay.no Drugfreepainrelief duringearlylabor
Effleuragemassagetorelaxmusclesbetweencontractions
Erythema Toxicumrashinnewborns
804 effaced 8cmdilated
NeoNatalabstinencesyndrome withdrawseizureFussypoor feeding
Thchomonal'SIS PretermriskAbdominaldiscomfort
ACTIVElabor 1MitralValvestenosis pulmonaryEdemaAFBright sidedHF
Tx DiureticBetablockerCalciumChannel blockersidelying AssistedDelivery
Labs
Bilirubin Platelet 15,000 350,000
Hgb1420 Glucose 4596
Hot 43631PreEclampsia swelling134 proteinuriaABDWeight gaintoutputabdominalpain
Herpes
Cytomegalovirus babyatriskforcongenitalanomalies
CordProlapse kneestochestsidelying continousFAR
Oxygen18lol perminute
[Show More]