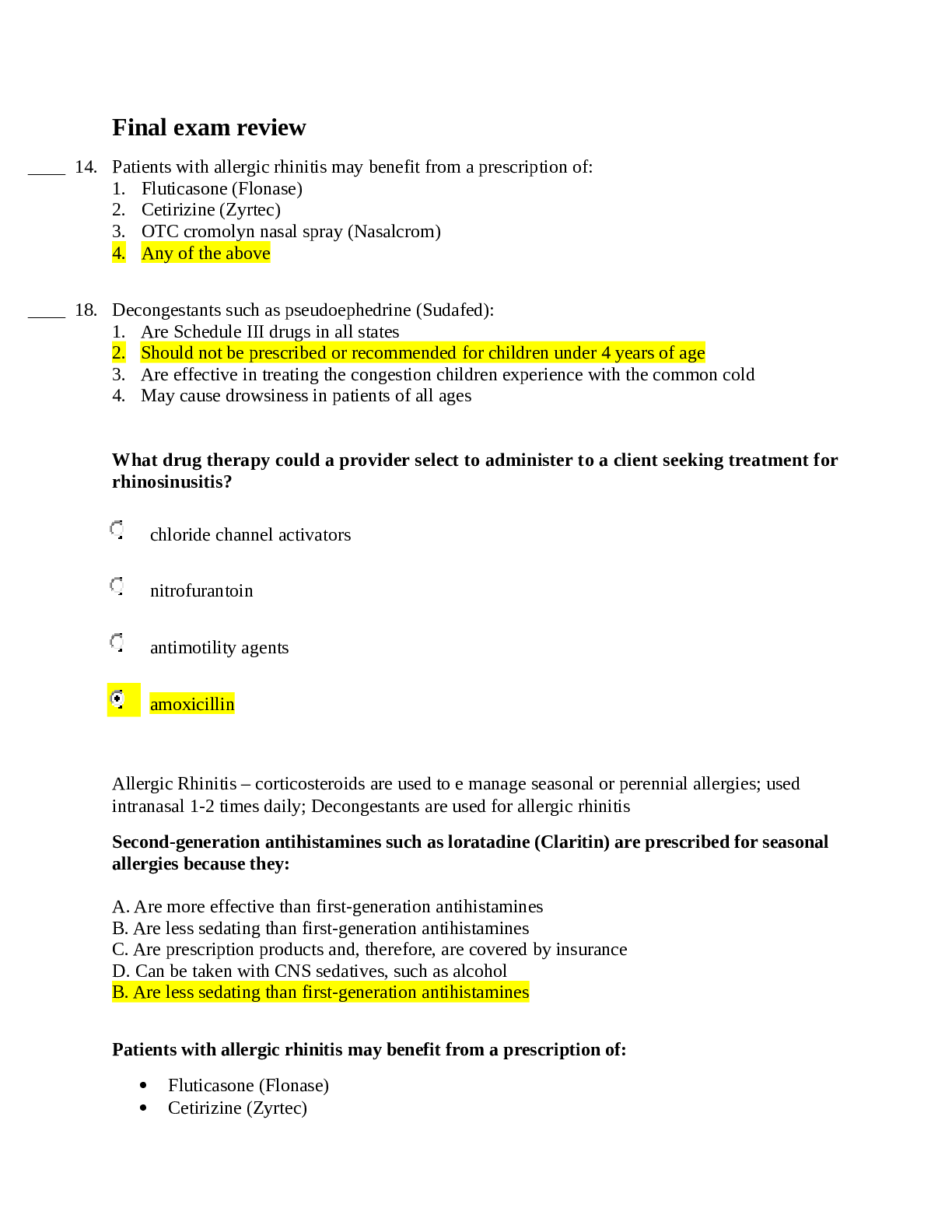
4. Patients with allergic rhinitis may benefit from a prescription of:
1. Fluticasone (Flonase)
2. Cetirizine (Zyrtec)
3. OTC cromolyn nasal spray (Nasalcrom)
4. Any of the above
____ 18. Decongestants such as pseud
...
4. Patients with allergic rhinitis may benefit from a prescription of:
1. Fluticasone (Flonase)
2. Cetirizine (Zyrtec)
3. OTC cromolyn nasal spray (Nasalcrom)
4. Any of the above
____ 18. Decongestants such as pseudoephedrine (Sudafed):
1. Are Schedule III drugs in all states
2. Should not be prescribed or recommended for children under 4 years of age
3. Are effective in treating the congestion children experience with the common cold
4. May cause drowsiness in patients of all ages
What drug therapy could a provider select to administer to a client seeking treatment for
rhinosinusitis?
chloride channel activators
nitrofurantoin
antimotility agents
amoxicillin
Allergic Rhinitis – corticosteroids are used to e manage seasonal or perennial allergies; used
intranasal 1-2 times daily; Decongestants are used for allergic rhinitis
Second-generation antihistamines such as loratadine (Claritin) are prescribed for seasonal
allergies because they:
A. Are more effective than first-generation antihistamines
B. Are less sedating than first-generation antihistamines
C. Are prescription products and, therefore, are covered by insurance
D. Can be taken with CNS sedatives, such as alcohol
B. Are less sedating than first-generation antihistamines
Patients with allergic rhinitis may benefit from a prescription of:
Fluticasone (Flonase)
Cetirizine (Zyrtec)
OTC cromolyn nasal spray (Nasalcrom)
All of the above
Nonpharmacological therapy includes increasing fluid intake, using nonmedicated cough drops,
nasal saline spray/drops to decrease viscosity of nasal secretions, and rest.
Anorexia is often associated with the common cold and fluids may need to be forced to maintain
hydration.
Infants who are congested cannot breathe and feed at the same time causing fluid intake to be
inadequate. Nasal suctioning may be required to clear secretions.
Oral decongestants are used for the temporary relief of nasal congestion from the common cold,
sinus infections, and allergic rhinitis. They may be used to promote nasal or sinus drainage and
are also indicated in the relief of eustachian tube congestion.
Pseudoephedrine for those over 4 y/o
Viral URI (the common cold) are self-limiting and require no treatment, the goal is relieving
irritating symptoms, specifically nasal congestion.
ANTIBIOTICS HAVE NO PLACE IN THE TREATMENT OF VIRAL URIs. They can cause
antimicrobial resistances to secondary bacterial infections.
Antihistamines have not been shown to change the course of the common cold. But many OTC
medications contain antihistamines, most likely for their “drying out” effect.
Decongestants are the mainstay treatment for the common cold (systemic or topical).
Tylenol/Ibuprofen/ASA can be given for fever and malaise.
Topical decongestants are safe for 3 consecutive days of use.
Topical decongestants adverse effects – transient stinging, burning, sneezing, dryness, local
irritation, rebound congestion with prolonged use.
Topical decongestants can symptomatically relieve nasal congestion and relieve ear blockage and
pressure pain.
Topical decongestant adverse reactions – insomnia, dizziness, weakness, tremor, or irregular
heartbeat.
Topical decongestant meds – Afrin, phenylephrine, oxylmetazoline, Neo-Synephrine
Theophylline – a bronchodilator that can affect the blood pressure
Monitor decongestant use in cardiac patients as they can increase hypertension from the added
vasoconstriction.
A diabetic client with high blood pressure and a pacemaker is seeking relief from excess
mucous production due to the common cold. Why would a provider not recommend
decongestants to this client?
The risk for contraindications is high.
The risk for poor metabolism of the drug is high.
The efficacy of the drug will be low due to the client’s other health conditions.
The risk for urinary incontinence is high.
Older adults are more likely to have adverse reactions from decongestants.
Common complications for URIs – Sinusitis, otitis media, asthma exacerbation
Echinacea is widely used in Europe, and increasing use in the US, for prevention of the common
cold and flu and is considered an herbal remedy.
How can a provider assess airflow limitation?
By examining the natural expiratory volume and total volume of exhaled air and their difference
By examining the forced expiratory volume and total volume of exhaled air and their ratio
By examining the relaxed state of the expiratory volume and last recorded volume of exhaled air and their
sum
By examining the elicited expiratory volume and limited volume of exhaled air and their quotient
Albuterol, beta agonists, is generally considered the first-choice medication for treatment of
asthma.
Inhaled corticosteroids are recommended as first-line therapy for athletes who have persistent
asthma to prevent worsening symptoms with exercise.
How is first-line treatment for COPD the same as for asthma?
Both diseases require maintenance therapies.
Both diseases are treated based on the number of hospitalizations.
Both diseases results from first- or second-hand smoking.
Both diseases are first always treated with short-acting muscarinic antagonists (SAMAs).
Mast cell stabilizer – cromolyn; works by inhibiting antigen-induced bronchospasm, blocks
histamine release, stabilizes mast cells.
Monoclonal antibody binds to free IgE and prevents them from responding to relevant allergens
____ 13. What is the desired mixed of T3 to T4 drug levels in newly diagnosed endocrine patients?
1. 99% of T3 and the rest is T4 to get rapid resolution.
2. Most needs to be T4 to mimic natural ratios of hormone.
3. The ratio is unimportant.
4. The mix needs to be 50-50 at first
[Show More]