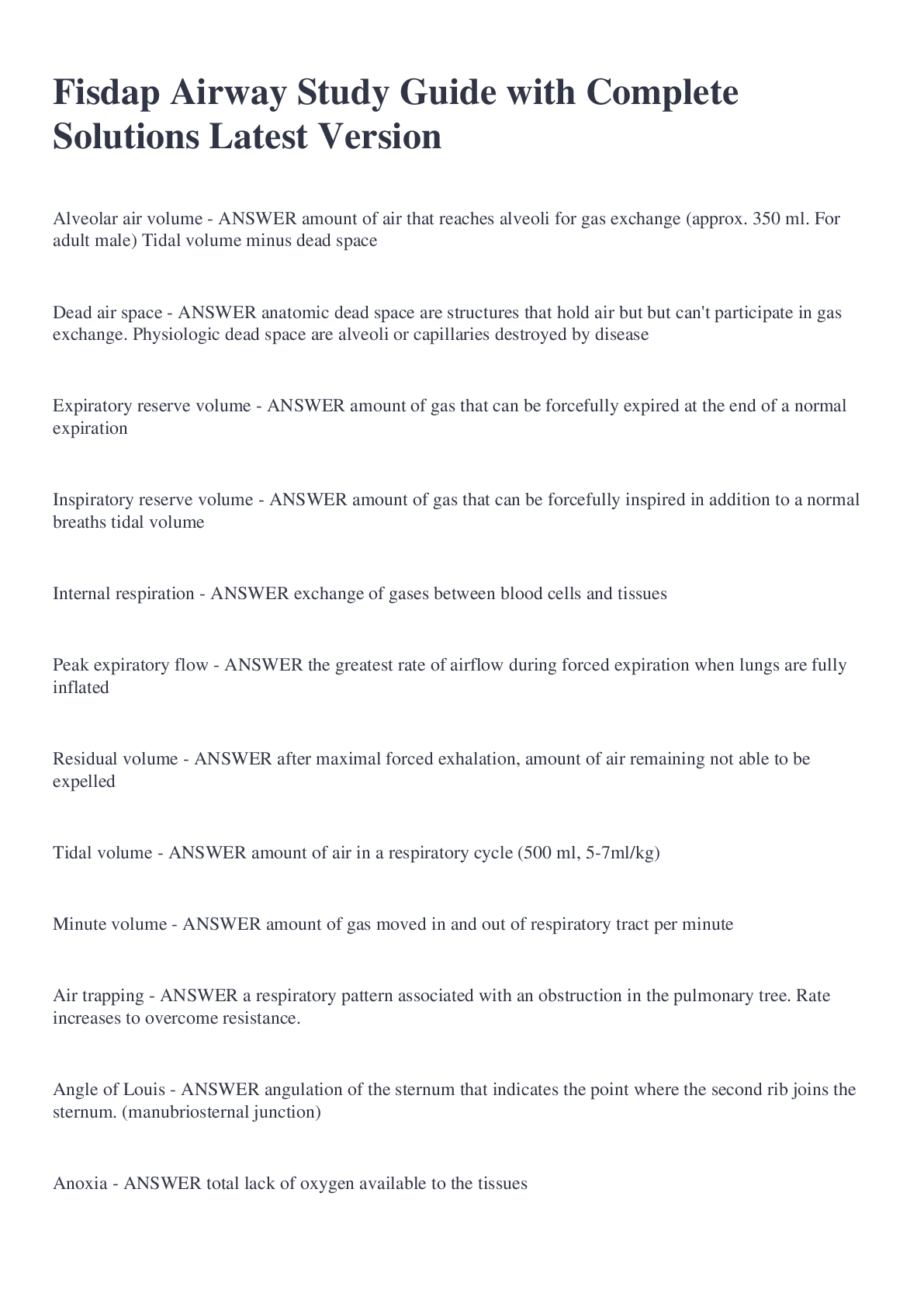
Alveolar air volume - ANSWER amount of air that reaches alveoli for gas exchange (approx. 350 ml. For adult male) Tidal volume minus dead space
Dead air space - ANSWER anatomic dead space are structures that hold air
...
Alveolar air volume - ANSWER amount of air that reaches alveoli for gas exchange (approx. 350 ml. For adult male) Tidal volume minus dead space
Dead air space - ANSWER anatomic dead space are structures that hold air but but can't participate in gas exchange. Physiologic dead space are alveoli or capillaries destroyed by disease
Expiratory reserve volume - ANSWER amount of gas that can be forcefully expired at the end of a normal expiration
Inspiratory reserve volume - ANSWER amount of gas that can be forcefully inspired in addition to a normal breaths tidal volume
Internal respiration - ANSWER exchange of gases between blood cells and tissues
Peak expiratory flow - ANSWER the greatest rate of airflow during forced expiration when lungs are fully inflated
Residual volume - ANSWER after maximal forced exhalation, amount of air remaining not able to be expelled
Tidal volume - ANSWER amount of air in a respiratory cycle (500 ml, 5-7ml/kg)
Minute volume - ANSWER amount of gas moved in and out of respiratory tract per minute
Air trapping - ANSWER a respiratory pattern associated with an obstruction in the pulmonary tree. Rate increases to overcome resistance.
Angle of Louis - ANSWER angulation of the sternum that indicates the point where the second rib joins the sternum. (manubriosternal junction)
Anoxia - ANSWER total lack of oxygen available to the tissues
Apnea - ANSWER respiratory arrest
Atelectasis - ANSWER abnormal condition characterized by collapse of alveoli, preventing exchange of CO2 and O2 in a part of the lungs
Barrier device - ANSWER thin film of material placed on the patient's face used to prevent direct contact with the patient's mouth during PPV
Carina - ANSWER where the trachea divides into right and left bronchi
Ronchi - ANSWER rattling or rumbling in the lungs. Inspiration and expiration. Fluid in larger airways and may be cleared from a cough.
Stridor - ANSWER harsh, high-pitched inspiratory sound best heard over the neck
Rattles (ronchi) - ANSWER inflammation and mucus or fluid in larger airways heard on inspiration. Associated with bronchitis or pneumonia
Crackles (rales) - ANSWER wet lungs - sounds like hair rolled in finger tips. fluid in smaller airways, crackling or popping sound on inspiration, sound that indicates presence of fluid in smaller airways
Croup - ANSWER viral infection in upper airway that sounds like a seal bark
Wheeze - ANSWER whistling sound heard on inspiration or expiration in pharynx, trachea, bronchi
Biot's respirations - ANSWER irregular respirations and rate with periods of apnea from increased ICP, brain damage at medulla, DKA, and OD'ing
Agonal respirations - ANSWER slow, shallow, irregular from anoxic brain injury
Central neurogenic hyperventilation - ANSWER similar to kussmaul respirations, deep and rapid breathing from increased ICP
Cheyne-Stokes respiration - ANSWER a pattern of gradually increasing rate and depth of breathing that tapers to slower and shallower breathing with a period of apnea before the cycle repeats.
Hering-Breuer reflex - ANSWER a reflex that limits inspiration and prevents over inflation
Hiccup - ANSWER spasm of the diaphragm
Benign tumor - ANSWER not spreading aggressively
Malignant tumor - ANSWER aggressively spreads
Secondary tumor - ANSWER spread from its original location
Primary tumor - ANSWER collection of cells that grow out of control, in excess of normal rate. Tumor that develops in only 1 tissue
Acute Respiratory Distress syndrome (ARDS) - ANSWER collection of fluid in the alveoli of the lung, usually from trauma or illness
Chronic Obstructive Pulmonary Disease (COPD) - ANSWER see Pathophysiology of COPD below.
Compliance - ANSWER resistance of the patient's lung tissue to ventilation
Bilevel Positive Airway Pressure Device (BiPAP) - ANSWER air pressure during inhalation and lower pressure to during exhalation
Continuous Positive Airway Pressure (CPAP) - ANSWER slight PPV throughout the respiratory cycle to prevent airway collapse
Costal angle - ANSWER the angle formed by the margins of the ribs and the sternum
Coughing - ANSWER protective mechanism from mucosal irritation. Can clear bronchioles and bronchi
Crepitation - ANSWER crackling sound from bones grinding
Cricothyroid membrane - ANSWER fibrous membrane between cricoid and thyroid cartilage
Cricothyrotomy - ANSWER emergency entrance into the airway
Dyspnea - ANSWER uncomfortable awareness of one's breathing
Functional reserve capacity - ANSWER at end of normal expiration, the volume of air remaining in lungs
External respiration - ANSWER exchange of gases between alveoli and pulmonary capillaries
Fraction of Inspired Oxygen (FiO2) - ANSWER The percentage of oxygen in inspired air. This percentage increases with supplemental oxygen. This value is commonly given as a decimal (Ex: room air is 21% O2, so FiO2 = 0.21).
Gagging - ANSWER Brooks on a Friday night
Gag reflex - ANSWER something Brooks is working on getting rid of.
Glottis - ANSWER true vocal cords and space between them
Hemoglobin - ANSWER a protein
Hilum - ANSWER point of entry for bronchial vessels, bronchi, and nerves in lung
Hypoxemia - ANSWER deficiency in the concentration of oxygen in arterial blood.
Hypoxia - ANSWER inadequate oxygenation of the cells
Orthopnea - ANSWER dyspnea relieved by a change in position, SLEEPING UPRIGHT with pillows, usually CHF pulmonary edema problem.
Oxyhemoglobin - ANSWER hemoglobin with oxygen bound to it
Partial pressure - ANSWER pressure exerted by an individual gas in a mixture
Positive End-Expiratory Pressure (PEEP) - ANSWER amount of pressure above atmospheric pressure present in the airway at the end of the expiratory cycle
Respiration - ANSWER exchange of gas
SpO2 - ANSWER Saturation of peripheral oxygen
Sellick maneuver - ANSWER technique used to compress the cricoid against the cervical vertebrae, occluding the esophagus
Surfactant - ANSWER specialized cells that keep alveoli from collapsing
Tracheal stoma - ANSWER surgical opening in neck
Tracheostomy - ANSWER surgical creation
Uvula - ANSWER fleshy tissue resembling a grape that hangs down from soft palate
Vallecula - ANSWER depression or pocket between the base of the tongue and the epiglottis
Ventilation - ANSWER mechanical process of moving air
Alveoli - ANSWER functional units of the respiratory system. Area in the lungs where the majority of the gas exchange takes place
Aspiration pneumonitis - ANSWER inflammation of the bronchi and alveoli caused by inhaled foreign objects.
Atelectasis - ANSWER partial or full collapse of the alveoli
Bacterial tracheitis - ANSWER potentially serious bacterial infection of trachea
Barotrauma - ANSWER injury that results from rapid or extreme changes in pressure
Bronchiolitis - ANSWER acute infectious inflammatory disease of the upper and lower respiratory tracts that results in obstruction of the small airways
Bronchitis - ANSWER inflammation of the lower respiratory tract
Bronchopulmonary dysplasia - ANSWER respiratory condition in infants usually arising from preterm birth
Carbon Dioxide narcosis - ANSWER mostly seen in COPD where CO2 is excessively retained causing ALOC
Carpopedal spasm - ANSWER cramping of extremities from hyperventilation
Circumoral paresthesia - ANSWER a feeling of tingling around lips
Collapsed lung - ANSWER lung that has failed and will no longer take in air
Costochondritis - ANSWER inflammation of the cartilage in the anterior chest that is painful
Cystic Fibrosis (CF) - ANSWER genetic disease marked by hyper-secretion of glands, including mucous in lungs (see Cystic Fibrosis below).
Emphysema - ANSWER destruction of the alveoli
Esophagoduodenoscopy - ANSWER endoscope is used to look at the esophagus, stomach, and duodenum
Hamman's sign - ANSWER crunching sounds occasionally heard on the heart when air is in mediastinum
Mainstem bronchi - ANSWER each of two main breathing tubes off the trachea
Mediastinitis - ANSWER infection in the mediastinum
Mediastinoscopy - ANSWER surgical procedure of looking into mediastinum with an endoscope
Non-Cardiogenic Pulmonary Edema (NCPE) - ANSWER fluid collection in the alveoli of the lung that does not result from heart failure
Ostomy - ANSWER a hole, usually referring to a surgically made hole.
Pallor - ANSWER pale washed out coloration of skin
Peak flow meter - ANSWER device used to assess severity of respiratory distress
Pleural effusion - ANSWER fluid in the pleural space, usually fluid that seeped from lung or chest wall
Pleurisy - ANSWER painful rubbing of pleural lining
Pneumomediastinum - ANSWER air entrapped within the mediastinum.
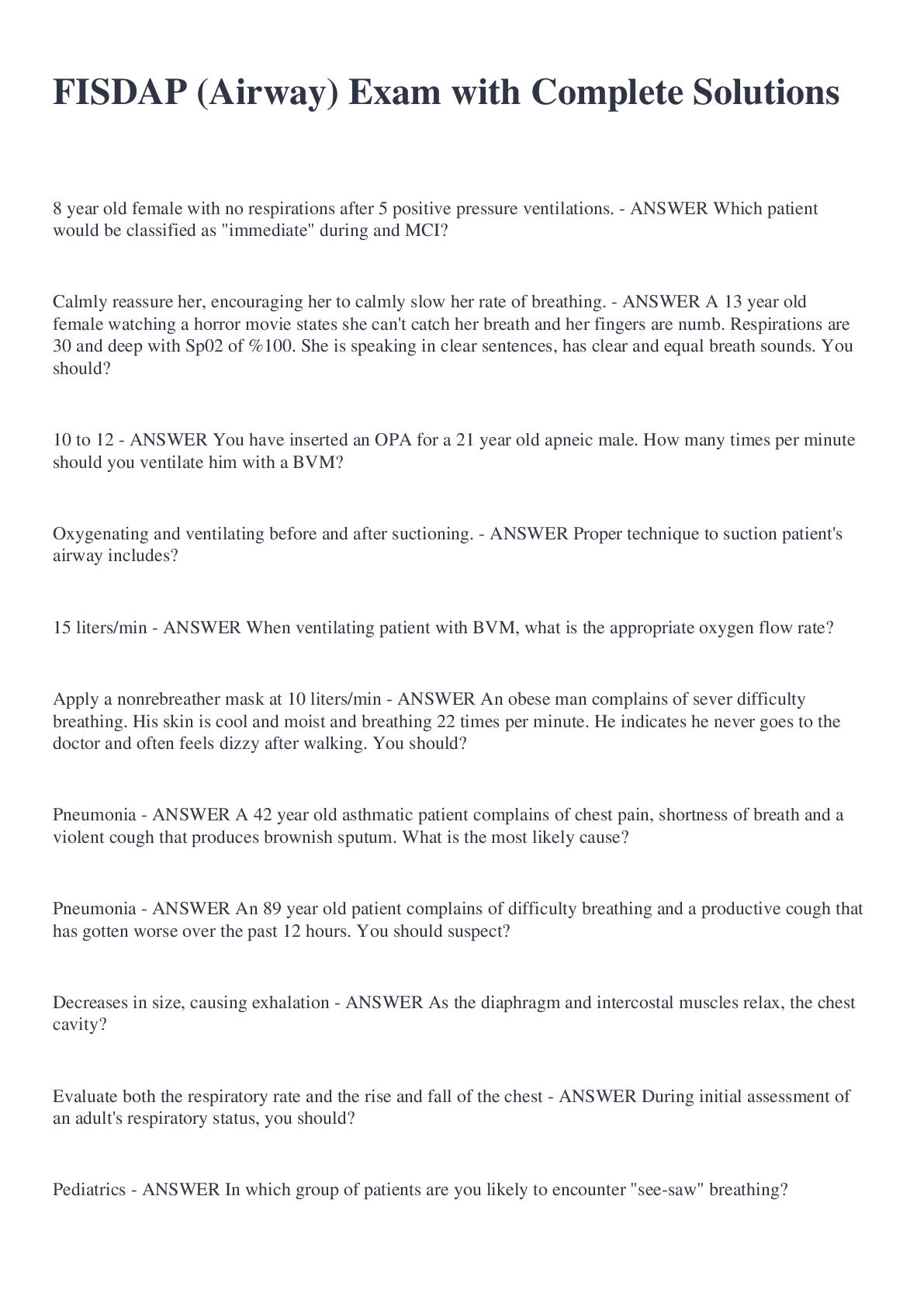
Pneumonia - ANSWER infection in lungs
Pulmonary abscess - ANSWER collection of pus within the lung
Pulmonary bleb - ANSWER cavity in the lung much like a balloon
Pulmonary Embolism (PE) - ANSWER clot lodged in pulmonary artery
Respiratory failure - ANSWER inadequate blood oxygenation and or ventilation to meet the metabolic demands of body tissue
Retractions - ANSWER use of accessory muscles
Supraglottic - ANSWER airway structure above vocal chords
Synchronized Intermittent Mandatory Ventilation (SIMV) - ANSWER vent setting that generally allows the patient to inspire at will and to the depth that he or she desires
Tracheostomy - ANSWER surgical hole in the anterior trachea for breathing
Tuberculosis (TB) - ANSWER highly contagious bacterial infection known for causing pneumonia and infecting other parts of the body
Peritonsillar abscess (PTA) - ANSWER infection of tissue between the tonsil and pharynx
Respiratory Syncytial Virus (RSV) - ANSWER a virus linked to bronchiolitis in infants and children
Methicillin Resistant Staphylococcus Aureus (MRSA) - ANSWER any of several bacterial strains of S. aureus resistant to methicillin (a penicillin) and related drugs
Upper Respiratory Infection (URI) - ANSWER viral syndrome causing nasal congestion and fever
Vancomycin Resistant Enterococcus (VRE) - ANSWER bacteria resistant to vancomycin
Apneustic Breathing (pages 476 - 477) - ANSWER Located in the pons, the apneustic center is the backup control center of involuntary respiration, secondary to the medulla oblongata. It stimulates the inspiratory center prolonging inhalation and inhibiting expiration. Another center located in the pons is the pneumotaxic center. It's main function is to inhibit inspiration, or act as a "shut off switch" for inhalation. The impulses of the pneumotaxic center normally override the the impulses of the apneustic center. When the pneumotaxic center is damaged, a respiratory pattern called apneustic respirations (a.k.a. apneusis) may occur. This consists of prolonged inhalation with decreased exhalation.
Characteristics of Cystic Fibrosis (pages 716 - 717) - ANSWER Cystic Fibrosis (CF) is a genetic disease that affects mostly the lungs, but also the liver, pancreas, and kidneys. It is mainly characterized by a change in the functioning chemistry of the glands that create thicker than normal secretions. These thicker than normal secretions cause chronic infections, resulting in the most common complication of the disease - pulmonary infections. Most fatalities from the disease result from progressive lung disease. Patients may present similar to those with COPD or pneumonia. You may see cough, chest wall pain, dyspnea, or fever. Physical examination may crackles on auscultation. The chest wall may be tender on palpation. As with other pulmonary disease processes, management hinges on supplemental oxygen, ventilation, and monitoring of oxygenation, ventilation function, and cardiac function.
Complications of ET Tube Placement (pages 530 - 531) - ANSWER If used incorrectly, a laryngoscope can break teeth and cause soft tissue damage. This can cause severe bleeding, further compromising the airway. Manipulation of any tissue can result in swelling, and if severe, laryngeal swelling can further obstruct airflow. Stimulation of the laryngeal structures may induce spasm of the larynx, especially in a patient with an intact or partially intact gag reflex. Spasm of the vocal cords will make it nearly impossible to pass an ET tube into the trachea. Severe laryngospasm obstructs the airway and further compromises oxygenation. Direct manipulation of the vocal cords with the tip of the laryngoscope blade or traumatically forcing a tube past the vocal cords may lead to nerve or direct cord damage, possibly resulting in permanent voice changes. Overinflation of the cuff after the tube is placed in the trachea can interfere with adequate blood flow and oxygenation to the mucosal lining that the cuff is pressed against, resulting in tissue death. Barotrauma is an injury that results from rapid or extreme changes in pressure. Overinflation of the lungs, especially when using positive pressure ventilation, can cause a tension pneumothorax. Patients with an underlying lung pathology, such as emphysema, are especially susceptible. Overinflation may cause a weakness to develop in the alveoli, alveolar ducts, or bronchioles called a bleb. This bleb could cause lung tissue to rupture, forcing air to leak into the pleural space, causing a pneumothorax. Accidental endobronchial intubation can occur from placing the ET tube too deep into the airway. What most commonly happens is that the tube is inserted into the right mainstream bronchus. This results in ventilation and oxygenation of only the right lung, with resulting hypoxia and inadequate gas exchange from the opposite lung. Esophageal intubation can cause gastric distention, vomiting, and aspiration. (Not only is the patient not receiving any oxygen with the tube in the esophagus, but the aspirated vomitus may cause further complications such as occlusion of the airway, more difficult intubation, poor bag compliance, and pulmonary infections such as pneumonia.) After tube placement, occlusions may occur from secretions or the patient biting the tube, causing lack of ventilations and hypoxia. Hypoxia may occur from prolonged or unsuccessful intubation. Dysrhythmias may occur. Intracranial pressure may increase.
Complications of Hyperventilation (pages 530 - 531, 722) - ANSWER Can lower CO2 because the rate or depth of breathing of blowing off too much CO2, causing respiratory alkalosis. Barotrauma is an injury that results from rapid or extreme changes in pressure. Overinflation of the lungs, especially when using positive pressure ventilation, can cause a tension pneumothorax. Patients with an underlying lung pathology, such as emphysema, are especially susceptible. Overinflation may cause a weakness to develop in the alveoli, alveolar ducts, or bronchioles called a bleb. This bleb could cause lung tissue to rupture, forcing air to leak into the pleural space, causing a pneumothorax. Hyperventilation while using a BVM can cause gastric distention, vomiting, and aspiration. The aspirated vomitus may cause further complications such as occlusion of the airway, poor bag compliance, and pulmonary infections such as pneumonia.
Complications of Intubating a Burn Patient (book 2, page 368) - ANSWER Airway edema progresses rapidly, obstructing the view of the landmarks used for intubation. Landmarks may be discolored, from soot or burned tissue, making it significantly more difficult to intubate. An example of this is that the normally white vocal cords may be black from inhaled soot. After the tube is placed, tape does not work well in the presence of facial burns because it does not adhere well. Another securement device should be used. In pediatric patients, the airway is much smaller than an adult's. Swelling will obstruct the airway much quicker than in the adult. If intubation is necessary, do it sooner rather than later in a pediatric patient.
Complications of Toxic Inhalation (book 2, page 356) - ANSWER As with all burns, airway management is key because the airway can become severely compromised is a very short period of time. Because of the potential lack of oxygen in the environment, patients may be hypoxic. Place toxic inhalation patients on supplemental oxygen via NRB. Treatment of chemical injuries revolves around the following basic steps: 1. Remove the exposed patient from the environment. 2. Secure the airway. 3. Provide supplemental oxygen. 4. Assist with ventilation.
Congestive Heart Failure (CHF) - ANSWER CHF is caused by a condition which reduces the efficiency of the heart muscle, through damage or overloading. It can be caused by myocardial infarction, hypertension, and stiffening of the heart muscle. These disease processes will increase workload, and over time, increases in workload will cause changes to the heart. The heart
[Show More]