NURS 5315 Advanced Pathophysiology Hematologic System
Core Knowledge Objectives with Advanced Organizers
Disorders of Hemostasis
1. Examine the etiology, clinical manifestations, and the pathophysiology of disord
...
NURS 5315 Advanced Pathophysiology Hematologic System
Core Knowledge Objectives with Advanced Organizers
Disorders of Hemostasis
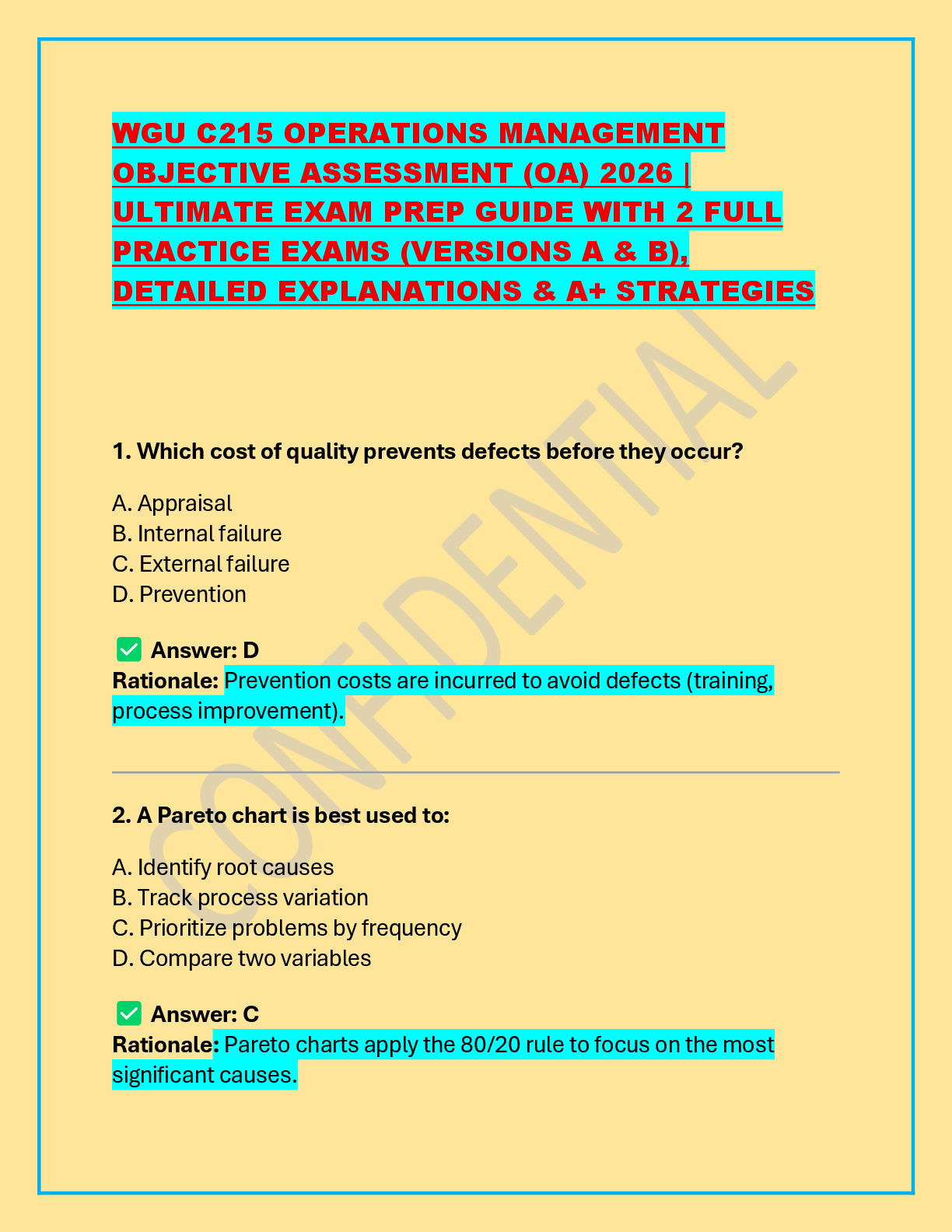
1. Examine the etiology, clinical manifestations, and the pathophysiology of disorders of hemostasis.
a. Discuss how the process of hemostasis is altered by select disorders and medications.
How is the Platelet Plug Process altered? How is Coagulation altered?
Aspirin Aspirin inhibit the formation of TXA2 by blocking the COX-1 pathway of the arachidonic acid pathway. N/A
Clopidogrel These drugs block ADP from binding to the P2Y12 receptor thus allowing cAMP to exert its action and prevent platelet aggregation. N/A
Warfarin N/A Warfarin blocks the genetic coding for vitamin K oxide reductase thus decreasing the amount available to reduce vitamin K. A lack of reduced vitamin K prevents the process of carboxylation and subsequently decreases the amount of “functional” vitamin K dependent coagulation factors
Low molecular weight heparin N/A They inhibit activated Xa and prevent the formation of the prothrombinase complex and consequently thrombin
Factor Xa Inhibitors N/A These drugs (fondaparinux, apixiban, rivaroxaban) increase antithrombin’s affinity for Xa. Antithrombin neutralizes Xa and thereby prevents the formation of the prothrombinase complex and thrombin.
-
-
-
-
-
-
-
-
-
-
-
-
-
-
-
-
-
-
--
-
-
-
-
-
-
-
-
-
-c. Analyze the pathophysiology of pernicious anemia, folate deficiency anemia, iron deficiency anemia, anemia of chronic disease, hemolytic anemia of the newborn and sickle cell disease and describe the implications for clinical practice.
Red Cell Disorders Pathophysiology Clinical Implications
Pernicious Anemia
Folate Deficiency
Iron Deficiency
Anemia of Chronic Disease
Hemolytic Disease of the Newborn
Sickle Cell Disease
Disorders of White Blood Cells
3. Analyze the etiology, clinical manifestations and pathophysiology of select white blood cell disorders.
a. Differentiate between the meanings and etiologies of quantitative abnormalities of white blood cell counts (leukocytes, neutrophils, lymphocytes, eosinophils, monocytes, basophils).
b. Differentiate between the meanings of acute and chronic leukemias and lymphocytic and myelogenous leukemias.
Type of Leukemia Definition
Acute Leukemia
Chronic Leukemia
Lymphocytic Leukemia
Myelogenous Leukemia
c. Evaluate the pathology, age of onset, clinical manifestations, and prognosis of the four types of leukemia and describe the clinical implications for your practice as a nurse practitioner. Reference the chart provided in the lecture.
d. Analyze the pathophysiology of acute and chronic leukemia and describe the clinical implications for your practice as a nurse practitioner.
e. Evaluate the etiology, epidemiology, pathophysiology and clinical manifestations of multiple myeloma and describe the clinical implications for your practice as a nurse practitioner.
f. Evaluate the etiology, epidemiology, pathophysiology and clinical manifestations of Hodgkin’s Lymphoma and Non-Hodgkin’s Lymphoma and describe the clinical implications for your practice as a nurse practitioner.
Type of Lymphoma Etiology Epidemiology Pathophysiology Clinical Manifestations
Hodgkin’s Lymphoma
Non-Hodgkin’s Lymphoma
[Show More]














 – University of the People.png)