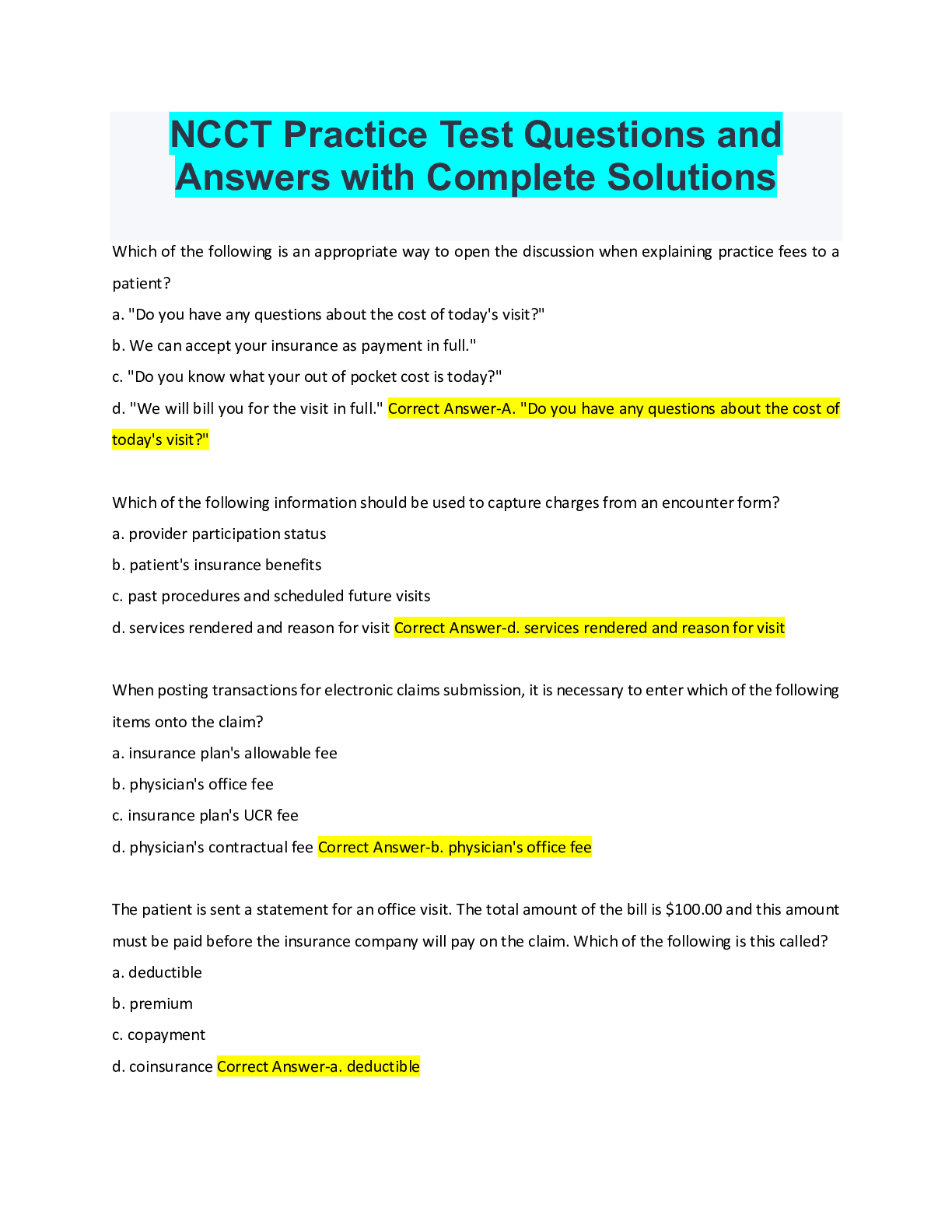
NCCT Practice Test Questions and
Answers with Complete Solutions
Which of the following is an appropriate way to open the discussion when explaining practice fees to a
patient?
a. "Do you have any questions about the
...
NCCT Practice Test Questions and
Answers with Complete Solutions
Which of the following is an appropriate way to open the discussion when explaining practice fees to a
patient?
a. "Do you have any questions about the cost of today's visit?"
b. We can accept your insurance as payment in full."
c. "Do you know what your out of pocket cost is today?"
d. "We will bill you for the visit in full." Correct Answer-A. "Do you have any questions about the cost of
today's visit?"
Which of the following information should be used to capture charges from an encounter form?
a. provider participation status
b. patient's insurance benefits
c. past procedures and scheduled future visits
d. services rendered and reason for visit Correct Answer-d. services rendered and reason for visit
When posting transactions for electronic claims submission, it is necessary to enter which of the following
items onto the claim?
a. insurance plan's allowable fee
b. physician's office fee
c. insurance plan's UCR fee
d. physician's contractual fee Correct Answer-b. physician's office fee
The patient is sent a statement for an office visit. The total amount of the bill is $100.00 and this amount
must be paid before the insurance company will pay on the claim. Which of the following is this called?
a. deductible
b. premium
c. copayment
d. coinsurance Correct Answer-a. deductibleWhen posting an insurance payment via an EOB, the amount that is considered contractual is the:
a. co-insurance
b. NON-PAR payment allowable
c. patient responsibility
d. insurance allowed amount Correct Answer-d. insurance allowed amount
Developing an insurance claim begins
a. when the patient calls to schedule an appointment
b. once the charges have been entered into the computer
c. when the patient arrives for the appointment
d. after the medical encounter is completed Correct Answer-a. when the patient calls to schedule an
appointment
When should a provider have a patient sign an ABN?
a. when a service is excluded from coverage under Medicare
b. when the items may be denied and prior to performing the service
c. when the service is covered under Part B fee schedule
d. prior to treating a patient who requires emergency services that might not be covered Correct Answerb. when the items may be denied and prior to performing the service
Which of the following regulations prohibits the submission of a fraudulent claim or making a false
statement or representation in connection with a claim?
a. Stark Law
b. Federal Claims Collection Act
c. Federal False Claims Act
d. Anti-kickback Law Correct Answer-c. Federal False Claims Act
The patient's total charges are $300. The allowed amount is $150. Benefits pay 60%. Which of the
following will the patient have to pay?
a. $60
b. $90
c. $150d. $180 Correct Answer-a. $60
Which of the following process makes a final determination for payment in an appeal board?
a. deposition
b. peer to peer
c. special handing
d. arbitration Correct Answer-d. arbitration
Which of the following items are mandatory in patient financial policies? (Select the three (3) correct
answers.)
a. participating insurance companies
b. provider fee schedule
c. statement that responsibility for payment lies with patient
d. collection process
e. expectation of payment due at time of service Correct Answer-c. statement that responsibility for
payment lies with patient
d. collection process
e. expectation of payment due at time of service
Collections agencies are regulated by the
a. Outpatient Prospective Payment System
b. Health Care Finance Administration
c. Uniform Bill of 2004
d. Fair Debt Collections Practices Act Correct Answer-d. Fair Debt Collections Practices Act
In order to have claims paid as quickly as possible, the insurance specialist must be familiar with which of
the following?
a. Automated claims status requests
b. clearinghouse processing procedures
c. prompt pay laws
d. payer's claim processing procedures Correct Answer-d. payer's claim processing proceduresWhich of the following are violations of the Stark Law? (Select the two (2) correct answers)
a. accepting gifts in place of payment from patients
b. referring patients to facilities where the provider has a financial interest
c. upcoding
d. negligent handling of protected health information (PHI)
e. billing for services not rendered Correct Answer-a. accepting gifts in place of payment from patients
b. referring patients to facilities where the provider has a financial interest
HIPAA allows a health care provider to communicate with a patient's family, friends, or other persons who
are involved in the patient's care regarding their mental health status providing
a. the patient is not incapacitated
b. a second physician signs off on the disclosure
c. the patient does not object
d. psychotherapy notes are used for further treatment Correct Answer-c. the patient does not object
[Show More]