*NURSING > Class Notes > NURSING NR 341 Critical Care Exam II Notes Latest Updated,100% CORRECT (All)
NURSING NR 341 Critical Care Exam II Notes Latest Updated,100% CORRECT
Document Content and Description Below
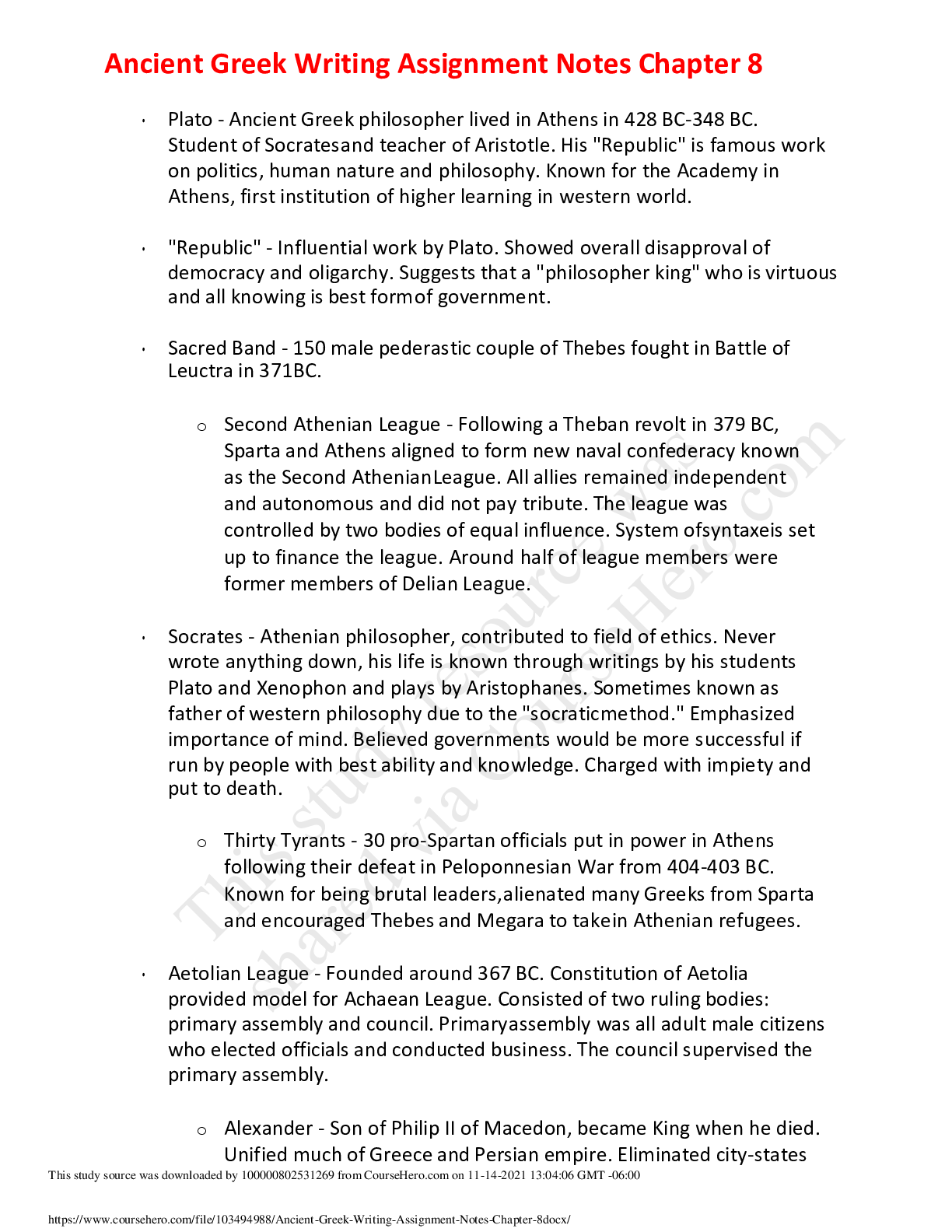
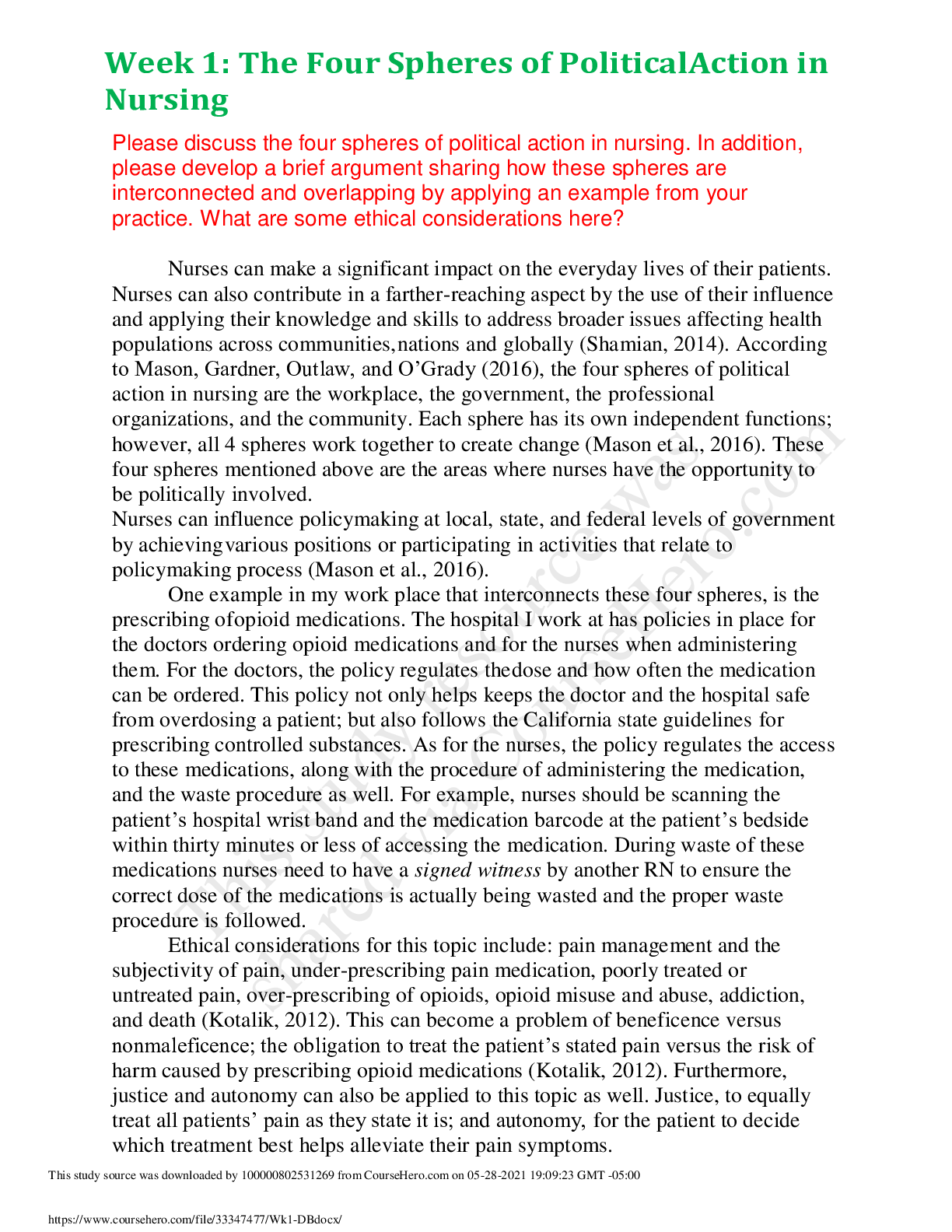
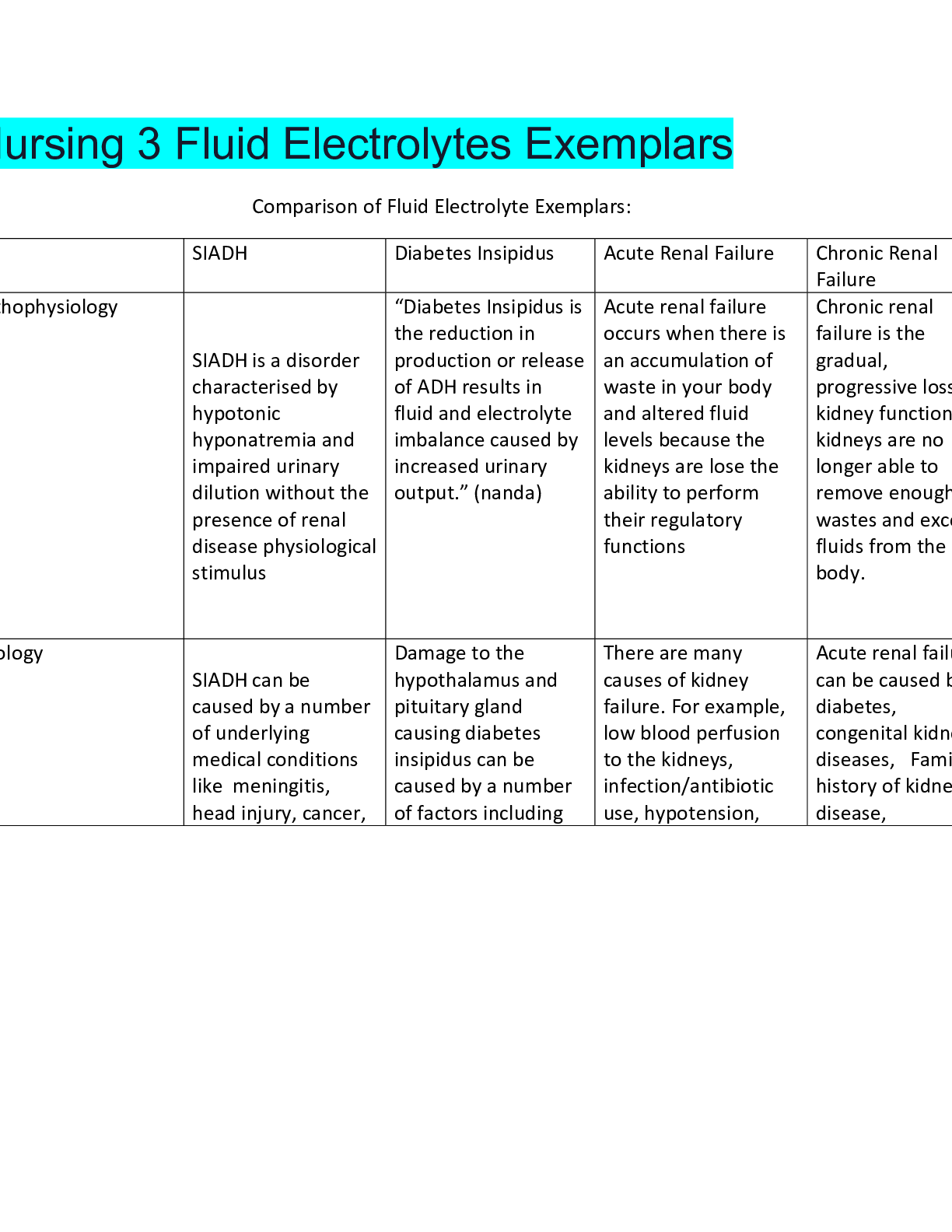
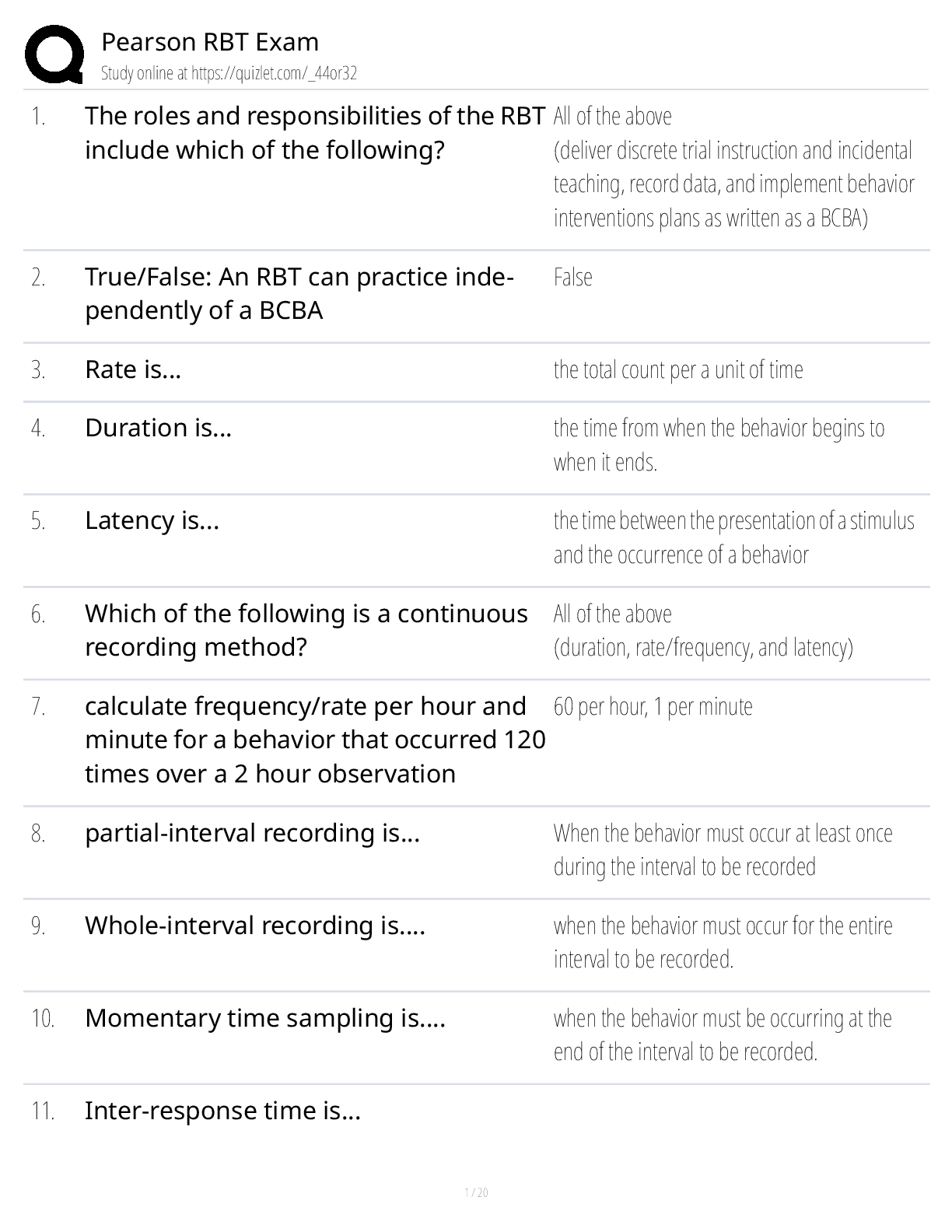
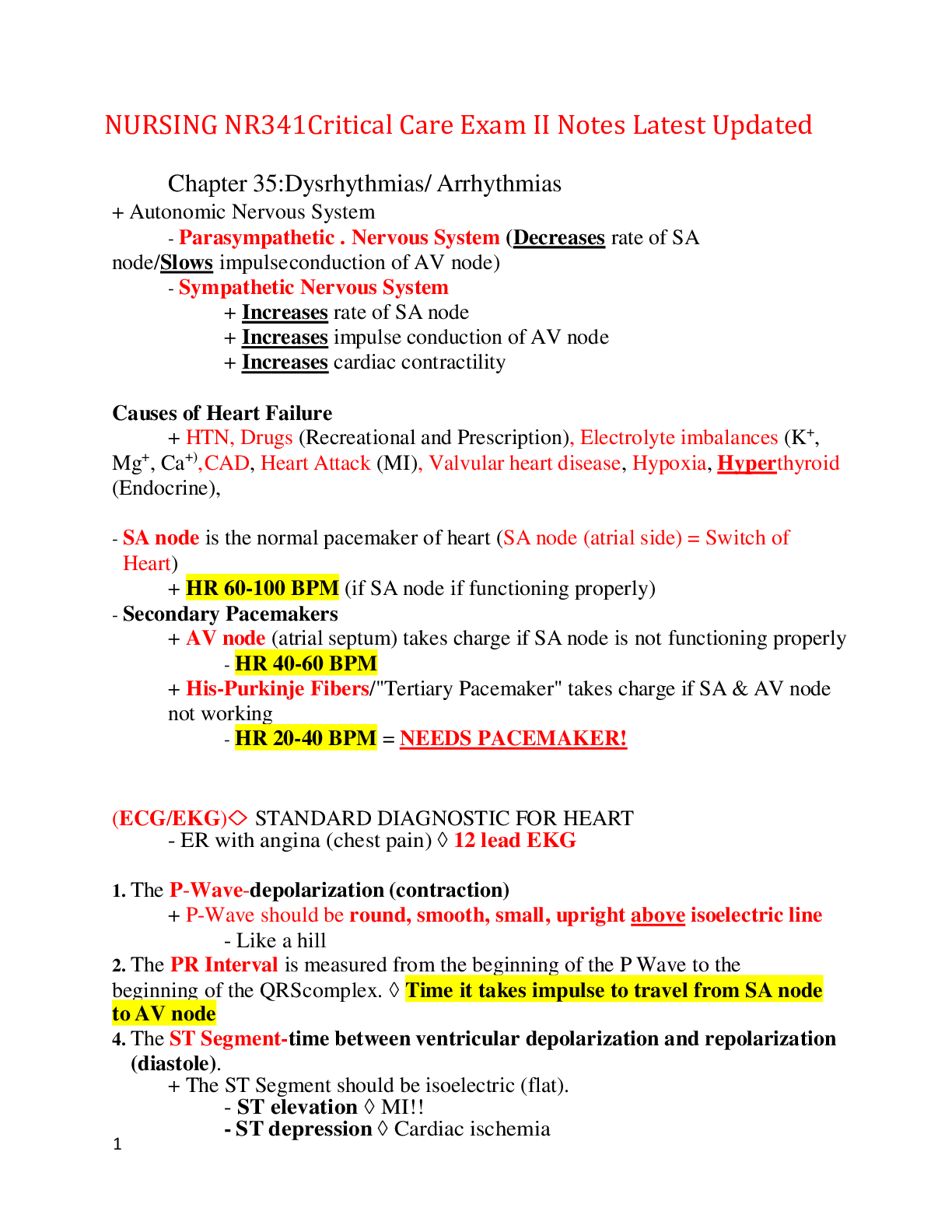
NURSING NR341Critical Care Exam II Notes Latest Updated Chapter 35:Dysrhythmias/ Arrhythmias + Autonomic Nervous System - Parasympathetic . Nervous System (Decreases rate of SA node/Slows impulse ... conduction of AV node) - Sympathetic Nervous System + Increases rate of SA node + Increases impulse conduction of AV node + Increases cardiac contractility Causes of Heart Failure + HTN, Drugs (Recreational and Prescription), Electrolyte imbalances (K+, Mg+, Ca+), CAD, Heart Attack (MI), Valvular heart disease, Hypoxia, Hyperthyroid (Endocrine), - SA node is the normal pacemaker of heart (SA node (atrial side) = Switch of Heart) + HR 60-100 BPM (if SA node if functioning properly) - Secondary Pacemakers + AV node (atrial septum) takes charge if SA node is not functioning properly - HR 40-60 BPM + His-Purkinje Fibers/"Tertiary Pacemaker" takes charge if SA & AV node not working - HR 20-40 BPM = NEEDS PACEMAKER! (ECG/EKG) STANDARD DIAGNOSTIC FOR HEART - ER with angina (chest pain) 12 lead EKG 1. The P-Wave-depolarization (contraction) + P-Wave should be round, smooth, small, upright above isoelectric line - Like a hill 2. The PR Interval is measured from the beginning of the P Wave to the beginning of the QRS complex. Time it takes impulse to travel from SA node to AV node 4. The ST Segment-time between ventricular depolarization and repolarization (diastole). + The ST Segment should be isoelectric (flat). - ST elevation MI!! - ST depression Cardiac ischemia 5. The T Wave represents the time for ventricular repolarization + T Wave should be upright [peaked T wave=hyperkalemia] + Inverted T wave=abnormality 6. The QT Interval-time taken for entire electrical depolarization and repolarization of the ventricles [prolonged=dysrhythmias] Key Things to Remember: + Tiny box = 0.04 seconds + Big box = 5 tiny boxes = 0.2 seconds + PR Interval = 3-5 tiny boxes (0.12-0.2 seconds) - PR interval > 5 boxes = 1st degree heart block + QRS = 1-3 tiny boxes (0.04-0.12 second) - QRS > 3 boxes = some type of ventricular problem + ST depression = Ischemia + ST elevation = MI (worse than ischemia) + P wave = Atrial contraction (multiple p waves= a-fib stroke) + Increase HR, Decrease BP = Dehydration Can be sinus tachycardia *** Signs and Symptoms of Decreased Cardiac Output *** + Decreased LOC (Confusion, Dizziness, Syncope, Restlessness, Agitation, Lethargy, Coma) + Muscle weakness, Angina, Decreased BP, SOB, Capillary Refill > 3 sec, hypoxia, decreased urine output, pale skin *** Dysrhythmias Key Points to Remembers *** + Dysrhythmias are not treated unless the patients are symptomatic + Dysrhythmias can be categorized as either too fast, too slow, or too ugly + Atrial dysrhythmias are fast heart rates with narrow QRS complexes + Atrial dysrhythmias lead to strokes + Ventricular dysrhythmias have wide QRS complexes + When rhythms are slow, we want to increase HR + When rhythms are fast, we want to slow HR + When rhythm is pulseless ventricular tachycardia or ventricular fibrillation, the patient requires defibrillation in addition to CPR + Pulseless electrical activity is when there is a cardiac rhythm, but the patient does not have a pulse + Asystole cannot be defibrillated Changes Associated with Myocardial Ischemia 1. ST segment is depressed = Ischemia - Normal ST line would be at isoelectric line level 2. T wave is inverted = MI (old) Patients with ischemia may display one or both changes Changes Associated with Injury 1. Physiologic Q wave- first negative deflection (wave) following the P wave. It is normally very short and narrow 2. Dramatic ST segment elevation = MI Normal Sinus Rhythm + Sinus node fires 60-100 beats/minute + Follows normal conduction pattern + P wave upright and uniform & precedes QRS complex + PQ interval 3-5 boxes + QRS narrow 1-3 boxes and equal distance - Distance same = Regular rhythm + T wave upright and uniform Sinus Bradycardia + Sinus node fires < 60 BPM + Follows normal conduction pattern + P wave upright and uniform & precedes QRS complex + PR interval 3-5 boxes + QRS narrow 1-3 boxes and equal distance - Distance same = Regular rhythm + T wave upright and uniform Nursing Action: 1. Assess the patient's tolerance to the rhythm/ Assess for signs of decreased cardiac output d/t HR is decreased 2. Identify cause & treat + If decrease BP = Give fluids + If decrease HR & symptomatic + Change position + Give atropine IV push or temp pacemaker + If HR is decreased d/t hypothyroid need Synthroid (levothyroxine) + If HR is decreased d/t increased intracranial pressure need to relieve pressure Sinus Tachycardia + Sinus nodes firing > 100 BPM + Follows normal conduction pattern + P wave upright and uniform & precedes QRS complex + PR interval 3-5 boxes + QRS narrow 1-3 boxes and equal distance - Distance same = Regular rhythm + T wave upright and uniform Possible Causes of Sinus Tachycardia + Running (Exercising) + Fever + Anxiety + Bronchodilators + Pain + Caffeine + FVD + Dehydration Nursing Action: 1. Assess the patient's tolerance to the rhythm/ Assess for signs of decreased cardiac output + If s/s present = symptomatic sinus tachycardia - Can have decreased cardiac output with increase HR d/t beat is not effective/ efficient + If symptomatic 2. Identify cause and treat + Dehydration = Give fluid + Fever = Give antipyretic 3. Beta blockers to decrease HR - Monitor: will also decrease BP 4. Calcium channel blockers to decrease HR Atrial Fibrillation (Give Amiodarone to convert back to sinus tachy) Common Causes of A-Fib + Electrolyte imbalance + Aging + Heart Disease + Atrial fibrillation is characterized by a total disorganization of p wave due to multiple ectopic foci + P waves are replaced by chaotic fib waves NO DEFINED P WAVE + QRS is NARROW and RR interval is long + Ventricular rate is between 60-100 BPM= A-fib with a controlled ventricular response + Ventricular rate greater than 100bpm is A–fib with a rapid (or uncontrolled) ventricular response + Atrial problem d/t no visible defined p wave = blood pooling blood clot brain (stroke), lung (PE) Nursing Action’s: Give 02 amiodarone 2. HR > 100 = symptomatic + Calcium channel blockers Diltiazem + Beta-blockers Metoprolol or Digoxin 3. HR > 70 IV Heparin or Enoxaparin immediately; THEN Warfarin + Check PTT 60-80 = Therapeutic level 4. Cardioversion- MAKE SURE ON ANTICOAGULANTS (Coumadin/Warfarin) + Heparin/Enoxaparin Check PTT (60-80=therapeutic) + Warfarin/Coumadin Check PT INR (2-3=therapeutic) 5. Observe for S/S of Stroke: FAST Face drooping - Does one side of the face droop or is it numb? Ask person to smile Arm weakness - Is one arm weak or numb? Ask person to raise both arms. Does one arm drift downward? Speech difficulty - Is speech slurred, are the unable to speak, or are they hard to understand? Ask the person to repeat a simple sentence "the sky is blue" Time to call 911 if any symptoms are present - even if they go away 6. Observe for S/S of PE= Rapid or irregular heartbeat, lightheadedness or dizziness, excessive sweating/fever, leg pain or swelling, or both, usually in the calf caused by a DVT, clammy or discolored skin (cyanosis) 7. Observe for s/s of MI Atrial Flutter + Saw-Tooth Nursing Action: 1. Assess the patient's tolerance to the rhythm/ Assess for signs of decreased cardiac output 2. Identify cause & treat + Monitor electrolyte imbalances (K+, Mg+) 3. If HR > = Slow down HR + Beta-blockers (metroprolol) monitor HR less than 60 notify HCP + Calcium channel blockers (Diltizem) + Cardioversion (ONLY IF ON ANTICOAGULANTS) First-Degree Hard AV Block + Prolonged PR interval (greater than 3-5 boxes) + HR is normal (60-100) + P wave is normal shape, uniform, and precedes QRS complex + QRS complex narrow and equal distance - Normal heart rhythm Nursing Action: 1. Assess the patient's tolerance to the rhythm/ Assess for signs of decreased cardiac output 2. Identify and treat cause + If you gave medication to decrease HR (betablocker, dig) = STOP Common Causes of 1st Degree Heart Block/ AV block: + MI + Previous CAD + Hypokalemia + Drugs (Digoxin and Beta-blockers) Premature Ventricular Contractions (PVC) + PVC is a contraction coming from an ectopic focus in the ventricles. It is the premature (early) occurrence of the QRS complex + A PVC is wide and distorted in shape compared to a QRS complex coming down the normal pathway + PVCs that arise from different foci appear different in shape from each other and are called multifocal PVCs. PVCs that have the same shape are called unifocal PVCs + When every other beat is a PVC, the rhythm is called ventricular bigeminy + When every third beat is a PVC, it is called ventricular trigeminy + Two consecutive PVCs are called a couplet Nursing Action: 1. Assess the patient's tolerance to the rhythm/ Assess for signs of decreased cardiac output (Can become symptomatic if 10-12 PVCs are present in 1 min) 2. Identify and treat cause + hypokalemia + Hypoxia + hypomagnesemia + smoking + anxiety Ventricular Tachycardia (VT) + Ventricular tachycardia (VT) occurs when there are three or more PVCs + Ventricular rate is 150 to 250 BPM + Rhythm may be regular or irregular + AV dissociation may be present, with P waves occurring independently of QRS complex + The P wave is usually buried in the QRS complex, and the PR interval is not measurable + The QRS complex is distorted in appearance and wide (greater than 3 boxes [0.12 seconds] in duration) - QRS can be monomorphic identical + The T wave is in the opposite direction of the QRS complex Nursing Action: CALL AN RRT!!! 1. Check pulse (carotid pulse) 1 side, no longer than 10 seconds + With a pulse 1. Tx with Amiodarone (300 mg IV, then 150 mg IV) 2. Cardioversion if Amiodarone does not work + No pulse 1. CPR 2. Defibrillate 3. Epinephrine 4. Defibrillate again V- Tach Common Causes: + MI + CAD + Electrolyte imbalance + Drug toxicity Ventricular Fibrillation (VF) + VERY BAD LETHAL DYSRHYTHMIA - Worse than V-Tach + VF is a severe derangement of heart rhythm characterized on ECG by irregular waveforms of varying shapes and amplitudes + Mechanically, the ventricle is simply "quivering," with no effective contraction, and NO CARDIAC OUTPUT OCCURS + HR is not measurable, Rhythm is irregular and chaotic, P wave is not visible, PR interval not measurable, QRS complex not measurable Nursing Action: CODE BLUE 1. CPR 2. Defibrillate 3. Epinephrine 4. Defibrillate again Asystole= NO HR Nursing Actions: 1. CODE BLUE, 2. CPR NO DEFIBRILLATION, 3. Epinephrine (3-5 doses, 3-5 min apart) Unit 3 & 4 Medications Atropine + Increases HR - Sinus bradycardia with s/s of decreased cardiac output Amiodarone + May terminate V Tach - Only use when there is a pulse Norepinephrine + Increases SVR Metroprolol + Decreases Contractility - Sinus tachycardia with s/s of decreased cardiac output Dobutamine + Increases Contractility Nitroglycerine + Decreases SVR - Use for angina, if relieved with nitro = stable angina Diuretic + Decreases preload - Use when circulating fluid is excess + Heart Failure + Kidney Failure Isotonic Fluid + Increases preload - Use when circulating fluid is deficient + Dehydration Diphenhydramine + Antihistamine Epinephrine + Used for pulseless rhythm - Use for Pulseless V-Tach, V-Fib, Asystole Unit 3: Dysrhythmia Management, Pacemakers, & Defibrillators Common Causes of Heart Problems + HF + MI + Electrolyte imbalance = - Ca+, Mg+, K+ + ETOH consumption (D/t decrease Mg+) Normal Heart Pacemakers 1. SA Node HR = 60-100 BPM 2. AV Node HR = 40-60 BPM 3. Purkinje Fibers HR = 20-40 BPM Dysrhythmia Management + Slow Rhythms < 60 1. Assess how patient's tolerance to the rhythm/ Assess for signs of decreased cardiac output If the patient is symptomatic (showing signs of decreased CO) 1. Medications to increase HR Atropine + Always check HR prior to giving Digoxin & betablockers d/t they decrease HR and can be the reason why pt. is experiencing a slow rhythm 2. Temporary/ Permanent pacemaker + If atropine doesn't work = bring crash cart - The defibrillator on the crash cart has a pacemaker option set HR 60-70 w/ pads, DO NOT SHOCK + Fast Rhythms > 100 + Sinus tachycardia 1. Assess how patient's tolerance to the rhythm/ Assess for signs of decreased cardiac output If the patient is symptomatic (showing signs of decreased CO) 1. Identify cause & treat + Fever Antipyretic + Anxiety Deep breathing, anxiolytic + Pain Analgesic + Dehydration Fluid + Other fast rhythms 1. Assess how patient's tolerance to the rhythm/ Assess for signs of decreased cardiac output If the patient is symptomatic (showing signs of decreased CO) 1. Valsalva maneuvers + Have pt. cough, bare down 2. Medications to slow HR Digoxin, Betablockers, Calcium Channel blockers 3. Anticoagulants Coumadin = PT/INR (2-3 normal) or Heparin PTT (60-80 normal) + Monitor for S/S of PE, Angina, Stroke 4. Cardioversion + Shock but not defibrillator Pacemaker Terminology - The mode, rate, and electrical output are decided by MD + Mode - Demand Allows the heart to work first, kicks in when HR is < - Fixed Bypasses the heart + Rate (HR) + Electrical Outputs -When increasing milliamps = uncomfortable d/t electricity so pt. is in ICU under a little sedation for comfort - Milliamps (Increase or decrease depending on condition; Obesity = > milliamps Pacemakers Temporary + Transcutaneous - Defibrillator machine Permanent + Subcutaneous Pocket L Chest Wall - Require surgery - Pre-Op Verify informed consent - In chart - Pt. has no questions - Pt. LOC is competent to sign + NPO (d/t anesthesia) - Post-Op + Inspect for drainage, inflammation, infection Electrical Pacemakers Atrial Pacing + When a pacing stimulus is delivered to the heart, a pacer spike will be seen on a cardiac monitor or ECG strip - The pacer spike, a vertical line, should be followed by a P Wave (atrial pacing) or QRS Complex (ventricular pacing) Biventricular (Dual-Chamber) Pacing + Dual chamber pacing will see spikes before P Wave and QRS complex for each paced beat Pacemaker Malfunction Lead but no QRS + Failure to capture occurs when the electrical charge to the myocardium is insufficient to produce atrial or ventricular contraction. This can result in serious bradycardia or asystole. Failure to capture is caused by: + Pacemaker lead damage + Battery failure (Battery lasts for ~ 5 years until it needs to be changed) + Dislodgement of electrode + Electrical charge set to low + Fibrosis at electrode tip (Can occur over time) Nursing Actions: 1. Check & Assess patient pulse 2. Monitor for signs and symptoms of decreased cardiac output 3. Notify MD Pacemaker Placement: Nursing Care + Patients usually stay for 24-hour observation - Post placement + The arm adjacent to the surgical sit should not be lifted - Arm in sling post procedure - Teach minimum shoulder movement, not above head + Incision monitored for infection - Bleeding, redness, swelling + Assess for hiccups - Hiccups = misplaced & initiating diaphragm + ID indicating pacemaker - No MRI - No wand/metal detectors in airports + Observe for S/S of decreased cardiac output Cardioversion- FOR FAST RHYTHMS WITH A PULSE!!! + Used to slow HR when meds aren't working + Depolarizes the cardiac cells so that the sinoatrial node can take over as the primary pacemaker of the heart External Cardioversion - Pads or paddles - Informed consent + Elective procedure - Conscious Sedation + D/t electrical = uncomfortable/painful Nursing Actions: 1. Document 2. Electrical monitor 3. Rhythm before, during, after 4. Document energy (Patient condition & how many times MD used) Internal Cardioversion + Automatic Implantable Cardioverter Defibrillator (AICD) - For patient at risk for lethal cardiac rhythms or sudden cardiac death + Will recognize lethal rhythm and shock patient if necessary - Will be taking an antiarrhythmic PO, but might need sometimes - Indicated for V-Tach + May have pacing capabilities Rapid Response Teams + Address changes in patient’s condition preventing a cardiac or respiratory arrest from occurring + Rapid Response Team When pt. is showing signs of decreased cardiac output, unstable + Nurse (ICU) + Physician + Respiratory Therapist Code Procedures + Recognition of arrest, assessment of ABCD's and call code - BLUE + 0 PULSE CODE BLUE Nursing Actions: 1. Begin CPR + Push hard and fast - Will need a backboard for adequate compressions 2. Code Team arrives with crash cart 3. Code procedure is determined by rhythm diagnosis, ACLS protocol, and patient's underlying pathology Crash Cart + Cardiac Board + Portable suction, Ambu Bag, Oxygen Tubing + Monitor/Defibrillator + Clipboard with code record + Airway equipment drawer/box + IV equipment drawer, Medication drawer, Misc. Supplies, Procedure Kits Code Management for Ventricular Rhythms & Asystole Ventricular Tachycardia WITHOUT a pulse *** Call CODE BLUE *** 1. CPR 2. Defibrillation 3. Epinephrine 4. Defibrillation V- Tach WITH A PULSE: Amiodarone, Cardioversion (if amiodarone doesn’t work), Epi Ventricular Fibrillation *** Call CODE BLUE *** 1. CPR 2. Defibrillation 3. Epinephrine Asystole *** Call CODE BLUE *** 1. CPR / DO NOT SHOCK 2. Epinephrine External Defibrillators + Strong Current and indicated for pulseless rhythms (V-Tach and V-Fib) Procedure: External Defibrillators + Paddle or defibrillation pad placement + Good contact with skin (protect from burns) Use pad to "wax/rip off" hair + Charge defibrillator to desired setting + "I'm clear, you're clear, everyone clear, oxygen clear" + Deliver shock & continue CPR 2 minutes, then re-assess rhythm Coronary Artery Disease (CAD) + Progressive narrowing of coronary artery by atherosclerosis - Coronary heart disease - Atherosclerotic heart disease - Narrow d/t plaque buildup Eat too much fat = Plaque buildup Risk Factors: Coronary Artery Disease + Nonmodifiable Factors - Age (Men > 45 y.o.; Women > 55 y.o) - Family history - Ethnic background (African American) + Modifiable Factors - Smoking - Inactivity - Teach 30mins x 5 day/week - Overweight (teach importance of losing weight and healthy well-balanced diet) - Cholesterol - High LDL (<100 Normal) - LDL is bad cholesterol - Low levels of HDL ( >40 M, > 50F Normal) - Want HIGH levels of HDL d/t carries LDL out - Triglycerides (<150 Normal) - Diabetes and Hypertension Acute Coronary Syndrome (ACS) + Ischemia with myocardial cell death + Imbalance of oxygen supply and demand - When you shovel snow, your demand is increased d/t using more energy + cold = narrow vessels STOP and warm body at first sign of pain + Includes stable angina, unstable angina or acute myocardial infarction Causes: Acute Coronary Syndrome (ACS) + Atherosclerosis, Emboli, Blunt trauma. Spasm Chronic Stable Angina + Precipitated by exertion or stress - D/t increased demand + Relieved with rest or nitroglycerin + Symptoms last less than 15 minutes - > 15 min = unstable angina Acute MI Types 1. Non-ST elevation MI (NSTEMI) 2. ST elevation MI (STEMI) Bad d/t = change in EKG Assessment of MI: + Midsternal chest pain - Severe, crushing, and squeezing pain (May radiate to arm, jaw, neck, back, hands, unrelieved w/nitrates or rest) + Diaphoresis + Dyspnea, tachypnea, and/or hypotension + Feeling of impending doom + Nausea + Dysrhythmias (Tachycardia d/t pain) + Anxiety (Females) Nursing Care: MI + Major Goals - Maintain cardiac output - Treat pain - Assess for complications - Promote energy conservation - Relieve anxiety - Ongoing and discharge teaching + Nursing Diagnoses - Acute Chest Pain - Poor Tissue Perfusion - Anxiety - Activity intolerance Diagnosis of MI 1. Chest Pain (A,B,C) 12 lead EKG (6 electrode on chest/ 6 electrode on extremities) 2. Signs and Symptoms (Often atypical symptoms in women Anxiety) 3. 12 lead - ST depression and/or T-wave inversion=MI - ST elevation=Injury (Old) - Q wave=MI/necrosis 4. Elevated Serum Troponin (ordered every 3-6 hours x 3) - Troponin I (< 0.4 Normal) no longer evident after 7-10 days + Enzyme/protein of heart muscle that is released during injury - Troponin T 10-14 days after MI Assessment/Nursing Interventions for Acute MI: + Stay with patient + Apply oxygen + EKG monitoring and VS + Give SL, Nitroglycerin (vasodilators), Morphine (pain relief) - Check BP Q5 min d/t vasodilators can decrease BP + At least 2 IV sites + Draw blood for troponin levels MONA 1. OXYGEN 2. NITRO + Vasodilator = Monitor BP - S/E of nitro = Headache Give Tylenol 3. MORPHINE + Relieve anxiety < demand 4. ASPIRINreduces blood clot formations + Clopidogrel (Plavix) + Educate on s/s of bleeding 1. Angiogram (Cath lab) Dye put into vessel + Check if pt. is taking metformin needs to be stopped 24 hrs. prior and resumed 48 hrs. after d/t can cause kidney failure + Check for allergies to iodine/shellfish - Give lots of fluid to flush out dye + Administer betablockers -Monitor VS - BP - HR 2. Angioplasty Pushing/ condensing plaque (widens vessel) + Common for patients with stable angina 3. STENT Keeps artery open (Stent is medicated so it won't occlude) 4. Bypass Graft Bypasses blocked artery (Take a large vein to bypass blocked artery) Medical Management: Acute MI + Medication Management - Pain Relief (Morphine) - Oxygen (2-4L/min) - Vasodilators - Nitroglycerin (Up to 3 doses, 5 min apart) CHECK BP!! - Prevention of platelet aggregation - Aspirin and Clopidogrel - Anticoagulants - Heparin, Enoxaparin - Betablockers - To decrease HR Therapeutic Procedures for MI: + Percutaneous transluminal coronary angioplasty (PTCA) + Bypass graft (also known as CABG) Complications of Acute MI + Dysrhythmias - AFIB - 1st degree heart block + Ventricular aneurysms + Heart failure/ Cardiogenic shock + Sudden death Interventional Cardiology (PCI/angiography) + Percutaneous Coronary Intervention (PCI) should be performed within 90 minutes of arrival to the emergency department, with a target of less than 60 minutes (door to balloon time). Angiography is performed with the goal of locating the presence of blockages in the coronary arteries. If blockages are found, the following may be performed + Percutaneous Transluminal Coronary Angioplasty (PTCA) - Plasty Push + Intracoronary Stenting - Drug-eluting stents To keep stent from occluding Percutaneous Transluminal Coronary Angioplasty: PTCA + Goal is to increase blood flow to myocardium Indications: PTCA + Treat coronary artery disease when there is occlusion of one to two coronary arteries + Occurrence of an acute myocardial infarction (MI), unstable angina or NSTEMI who are hemodynamically unstable + Used as an alternative to coronary artery bypass graft + Used with stent placement to prevent artery re-occlusion and to dilate with coronary artery - CAN RE OCCLUDE MAJOR TROUBLE NOTIFY MD, KEEP PT NPO d/t will need to go back to OR Complications: PTCA + Artery dissection + Cardiac tamponade (pericardial sac) = EMERGENCY D/t heart can't contract - Use needle to aspirate + Hematoma formation near insertion site - Assess for s/s > HR; < BP + External bleeding at the insertion site (femoral artery) - Assess for s/s - > HR - < BP + Allergic reaction related to the contrast dye + Embolism - Assess for s/s - Chest pain - SOB + Retroperitoneal bleeding (Backside) - Assess for s/s - > HR - < BP + Restenosis of treated vessel + Acute kidney injury Give fluids to prevent Nursing Actions: + Teach to keep extremity straight for 6 hrs. d/t don't want blood clot to move + Pressure dressing to < risk of bleeding (Observe site for bleeding) + Pt. on bed rest (Use bed pan only) + Check pedal pulses (Q 15min x 4, Q 30min x 2, Q 2 hr. x 4) Coronary Stents + Tubes placed in conjunction with angioplasty to keep vessel patent + Help prevent the restenosis associated with angioplasty (Similar procedure as PTCA) + Anticoagulation therapy - Stent is positioned at the site of the lesion - The balloon is inflated, expanding the stent - The balloon is then deflated and removed - The implanted stent is left in place Nursing Care Interventional Procedure: Stent + Client Educations - Lifestyle modifications + Exercise + Diet + Smoking cessation + Decrease LDL, increased HDL - Medications + Compliance - Warning signs and symptoms + Notify MD unstable angina + Nursing Considerations - Pre-procedure + NPO + Stop Metformin - 24 hrs. prior, 48 hrs. post + Witness informed consent - Post-procedure + VS (Q15min x 4, Q30min x 1, Q2hr x 4) + Assess 5 P's - Pain - Pallor - Paralysis - Paresthesia - Pulse CABG Surgery (Open Heart Surgery) + If client is not a candidate for an interventional procedure, CABG may be considered Goals of CABG Surgery: + Increase blood flow to myocardium + Relieve symptoms + Prolong survival + Improve quality of life Provides Additional Conduits for Blood Flow + Saphenous vein - LE + Internal mammary artery + Radial artery Nursing Care: CABG + Client Education - Lifestyle modifications - Medications - Warning signs and symptoms + Nursing Considerations - Pre-procedure + NPO - Major procedure Intubated - Intra-procedure + Constantly monitoring VS in OR - Post-procedure + Cardiac machine + BP machine + Check VS + Ambu bag accessible + Assess site - S/S infection + Assess 5 P's + KEEP PATIENT FLAT SUPINE Unit 4: Hemodynamics Introduction + Hemodynamic monitoring is coming in critical care unit - Studies relationships among several variables 1. Heart flow - [< HR = < CO]; [> HR = < CO] d/t not contracting effectively 2. Blood Flow 3. Oxygen Delivery 4. Tissue perfusion *** Ask yourself: IS EVERYTHING BEING PERFUSED ADEQUATELY? *** + Vital signs tell a lot + Central lines measure what's happening inside of the heart Components of Cardiac Output Cardiac Output (CO) = HR X SV Stroke Volume Components: + Stroke volume is that amount of blood ejected during each contraction 1. Preload (Volume) + Length of diastole + Venous return 2. Afterload (Resistance) + Arterial tone + Autonomic nervous system control + Hormone and catecholamine release 3. Contractility + Degree of muscle stretch + Catecholamine release + Inotropic agents Factors that affect HR: + Autonomic nervous system + Temperature + Electrolytes + Adrenal stimulation + Catecholamine release *** Preload (Volume) *** 1. Central Venous Pressure (CVP) = 2-6 + Use a central line to measure CVP (right atrial pressure) - CVP = Right Preload = Volume coming into the heart from Body Increased Preload (CVP) + Causes: - Fluid Volume Excess + Too much IV fluid + HF + Clinical Manifestations: - Right Sided HF (BODY) Signs and Symptoms + JVD + Bounding Pulses + Peripheral Edema + Wt. gain + Ascites + Hepatomegaly + Splenomegaly - Left Sided HF (LUNGS) Signs and Symptoms + Pulmonary Edema + Crackles + SOB + Increased RR + Coughing + Restlessness + Frothy Sputum + Decreased O2 Saturation + Treatment: - Fluid Restriction - Lasix Decreased Preload (CVP) + Causes: - FVD (Diabetes Insipidus, bleeding, diarrhea, dehydration, vomiting, DKA) + Clinical Manifestations: - Dry Mucous Membranes, Decreased BP, Increased HR, Weak thread-pulses, decreased urine output + Treatment: - Give Fluid and Give Blood (If bleeding) Increased Afterload (Vasoconstriction) + Causes: - Pulmonary HTN - Pulmonary Embolism (PE) - Too much (increased dose) of vasoconstrictor + Dopamine + Norepinephrine + Clinical Manifestations: - Hypertension + D/t narrow - Cool, clammy, pale skin + D/t not getting to - Weak thready pulses + Treatment: - Vasodilator: Nitroglycerin Decreased Afterload (Vasodilation) + Causes: - Too much (increased dose) of beta-blockers, ace inhibitors - Septic shock + Clinical Manifestations: - Decreased LOC + Confusion - Warm flushed skin + "Vessels are open and blood is in the garden" - Decreased U/O + D/t kidney's and other organs are not getting perfused -Hypotension + Treatment: - Vasoconstrictor: Dopamine, Norepinephrine Increased Contractility (strength of muscle) + Causes: - Thyroid storm - Positive inotropic medications + Epinephrine + Norepinephrine + Dopamine + Digoxin + Calcium + Clinical Manifestations: - Palpitations - Dysrhythmias - Tachycardia - Decrease C/O s/s + Treatment: - Beta-blockers: Metoprolol Decreased Contractility + Causes: - MI - Heart Failure -Calcium Imbalances (Calcium gluconate to correct it) - Too much (increased dose) of Betablockers, Calcium channel blockers + Clinical Manifestations: - Dysrhythmias - Bradycardia - Decrease C/O Muscle weakness, Angina, Decreased BP, SOB, Cap refill > 3s, Hypoxia, Decreased Urine Output, Pale skin -BNP Increased + Treatments: - Positive inotropes Dobutamine Blood Pressure ** MAP: [1 Systolic + 2 (Diastolic)] ** 3 ** Normal MAP: 70-100/3 **- For adequate perfusion Hemodynamic Monitoring + Noninvasive Modalities - Safety measures + Use proper cuff size - Too large Blood pressure will be low - Too small Blood pressure will be high + Use proper position - Transducer at phlebostatic axis + Use septic technique - Disposable cuffs if patient is in isolation - Assessment of jugular venous pressure - Assessment of serum lactate levels not good if rising + Check for pt. in shock d/t when body is not being adequately perfused the body anabolic for energy = > lactic level + Invasive Modalities - Arterial Pressure Monitoring A-line Used 90% of time for BP reads only - Right Atrial Pressure/ CVP monitoring Central line to measure CVP (2-6 normal) - Pulmonary Artery Pressure monitoring Used when unstable and in ICU + Indications - MI - Open heart surgery (Bypass) + Components of Hemodynamic Pressure Monitoring + Invasive catheter, noncompliant pressure tubing, transducer and stopcocks, flush system, bedside monitor, CONSENT + Nursing Implications + Patient Position Supine with arms above head. 4th intercostal space, mid axillary line + Zeroing the transducer phlebostatic axis + Infection control Big complication with invasive lines - Allen’s test -Assess for bleeding/infection/thrombus formation - Check distal cap refill - Prevent air emboli=flush air bubbles - Have patient suck in their breath - Assess 5 P's distal to line Pain, Pallor, Paresthesia, Paralysis, Pulse Arterial Pressure Monitoring + Invasive technique to monitor arterial blood pressure - Sites: + Radial Artery - Allen's test prior to verify collateral circulation in extremity + Brachial Artery + Femoral Artery (last choice; risk for infection) - Equipment: + Pressurized flush solution with transducer + Pressure at 300 mmHg + A-line catheter (Angiocath) - Nursing Implications: + Apply pressure when disconnecting d/t normal bleeding time post removal is 5-7 mins CVP/RAP Monitoring + Central Venous Pressure (CVP) preload on right side of heart - Measured through a central venous catheter/ TLC - Used to guide fluid replacement and assess the status of the right ventricle - Normal CVP/RAP values are 2-6 mmHg + Nursing Implications: - Assess site for complications - Change dressing per hospital protocol or anytime it is soiled + Complications: - Bleeding - Infection - Air embolus Pulmonary Artery Pressure Monitoring - Measured through a Pulmonary Artery Catheter (PAC)- left ventricle function -PAP too high (too much preload); PAP too low (not enough preload) + Insertion of PA Catheter - Proper position of patient - Look for waveform changes as catheter progresses - Chest X-Ray + Routinely measure PAWP/PAOP/PCWP - Never a continuous measurement - D/t will occlude artery (Inflate balloon and quickly deflate) - Record amount of air to inflate balloon NO MORE THAN 1.5 mL + Monitor for Complications - Pneumothorax Stages of Shock 1. Initiation + No obvious clinical signs - Assess and observe for change + O2 sat + Lactic acid level (> = not enough 02) -Increase in Lactic acid = Anaerobic metabolism 2. Compensatory + Compensatory mechanisms initiated INTERVENE NOW! - Sympathetic Nervous System + Increased HR + Increased Temp + Increased RR - RAAS + Vasoconstriction to give vital organs blood - Aldosterone Retain sodium, lose potassium if too high - ADH Keep fluid = DECREASED U/O - Cortisol + Increased - Glucose (hyperglycemia) + Increased d/t body converts stored glycogen to glucose for energy 3. Progressive + Profound cardiovascular effects HARD TO TREAT! - Decreased BP - Hypoxemia - S/S Decreased C/O - Increased capillary permeability + Fluid in lungs (Dyspnea, Crackles, Increased RR) + Anasarca (Generalized edema) - Increased lactate level - Normal lactate level 0.5-1.0 4. Refractory + Inadequate tissue perfusion unresponsive to therapy RECOVERY UNLIKELY! - Decreased BP - Decreased HR + Decreased HR is a warning sign d/t HR is > in earlier stages - Decreased Glucose, Cerebral Edema - Poor Reflexes, Dilated Pupils - Unresponsive Shock 1. Hypovolemic Shock + Fluid Volume Deficit - Inadequate intravascular (circulating) blood volume CO D | BP D | HR I| CVP D (less than 2) | PAWP I | PVR & SVR I - PVR & SVR increase d/t body vasoconstricts to keep fluid Causes: Hypovolemic Shock + External or internal fluid loss - Diarrhea, vomiting, bleeding, burns, DKA, Diabetes Insipidus, Hemorrhage Clinical Manifestations: Hypovolemic Shock + Signs and Symptoms of FVD - Cool & clammy skin - Weak, thready pulse - Decreased UO - Decreased BP/Increased HR Collaborative Management: Hypovolemic Shock + Goal is to stop fluid loss and replace lost volume NS, LR, plasma, platelets - Client positioning Supine with lower extremities elevated on pillows - Use warmer with blood products 2. Cardiogenic Shock + Engine failure MI, Heart Failure - Heart fails to act as an effective pump Decrease CO; impaired perfusion CO D | BP D | HR I | CVP I (over 6) | PAWP I | PVR I | SVR I Causes: Cardiogenic Shock + Decreased Contractility - Myocardial Infarction, valve dysfunctions, certain drugs - Heart Failure Clinical Manifestations: Cardiogenic Shock + Heart Failure Signs and Symptoms - Left side = Lungs - Right side = Body (Brain Natriuretic Peptide > 100 = HF) Collaborative Management: Cardiogenic Shock + Goal is to improve cardiac function - Dobutamine to increase strength & contractilityWant to see good BP/labs -Smaller doses of Furosemide to < preload; Nitroglycerin 3. Obstructive Shock - Physical impairment to adequate circulating blood flow CO D | BP D | HR I | CVP I | PAWP I | PVR I | SVR I Causes: Obstructive Shock - Cardiac Tamponade - Tension Pneumothorax - Pulmonary Embolism Clinical Manifestations: Obstructive Shock + Cardiac Tamponade S/S Muffled heart sounds, JVD, hypotension, pulsus paradoxus (systolic BP drops during inhalation) + Tension pneumothorax S/S Deviated trachea, + PE S/S Dyspnea, SOB, chest pain, hemoptysis (coughing blood) Collaborative Management: Obstructive Shock + Cardiac Tamponade Pericardiocentesis + Tension pneumothorax Needle aspiration, chest tube + PE TPA to break clot and Heparin to prevent further clots 6. Anaphylactic shock Massive vasodilation, bronchoconstriction + Introduction of an antigen into a sensitive individual initiating an antigen-antibody response - Release of vasoactive mediators Histamine CO D | BP D | HR I | CVP D | PAWP D | PVR I | SVR D Causes: Distributive Anaphylactic Shock + Contrast dye + Latex + ACE inhibitors + Bee stings Clinical Manifestations: Distributive Anaphylactic Shock + Flushed, red, skin + Dyspnea (D/t massive bronchoconstriction) + Wheezing + Stridor + Hives + Itching + Decreased BP (D/t massive vasodilation) + Pain +Angioedema Collaborative Management: Distributive Anaphylactic Shock + Epinephrine + Oxygen + Diphenhydramine + IV Steroids Cortisol/Methroprominsol + Vasoconstrictor + Bronchodilator (Albuterol) + Nebulizer Tx + Dopamine if BP is < 3. Septic shock Massive vasodilation + Follows invasion of a host by a microorganism - Systemic Inflammatory Response Syndrome (SIRS) Widespread inflam response CO D | BP D | HR I | CVP D | PAWP D | PVR D | SVR D Causes: + Infection - Bacterial 1. SIRS 2. Sepsis 3. Severe Sepsis 4. Septic Shock Clinical Manifestations: + Flushed, red skin (D/t massive vasodilation) + Decreased BP + Decreased LOC + Increased WBC (Normal (4-10) + Decreased U/O + Decreased PLT/ Increased PTT + Increased lactic acid + Riggers (uncontrolled shaking) Collaborative Management: + Measure lactate level + Culture everything and STAT broad spectrum antibiotics FIRST + Bolus fluids + Dopamine or Norepinephrine to increase BP Shock Expected Findings + Physical Assessment - Decreased/Changes in LOC (Dizziness, Syncope, lethargy, restlessness) - Increased RR (Dyspnea, SOB, Wheezing, Stridor) - Weak, thready pulses (Hypovolemic shock) - Decreased U/O (< 30 ml/hr.) - Decreased/ Absent peristalsis/ bowel sounds + Lab Results - pH variations; PaO2 decreased (D/t not being perfused) - Serum Lactic acid increased (Normal 0.5-1.0) - Glucose increased - BUN increased (D/t kidneys not being perfused) - Creatinine increased (D/t kidneys not being perfused) - Urine specific gravity increased (D/t RAAS is holding onto fluids) - Culture (Blood, urine, wound) D/t need to find source of infection - PT/INR/PTT (Risk for coagulation) - Decreased PLT & Increased WBC (Indicative of infection Septic Shock) Disseminated Intravascular Coagulation (DIC) + DIC can be a complication of septic shock - It has a "Thrombotic Phase" -- activation of clotting factors - Then a "Fibrinolytic Phase" -- clotting factors are depleted and the client is at risk for hemorrhage Multiple Organ Dysfunction Syndrome (MODS) + Progressive dysfunction of two or more organ systems - 50% chance of death with 2 or more organ system dysfunctions - 80% chance of death with 3 or more organ system dysfunctions + Can occur after any severe injury or illness + Results in maldistribution of blood flow to organs + Organs severely affected - Lungs - Splanchnic bed - Liver - Kidneys Clinical Manifestations: MODS + Decreased PaO2/ Increased CO2 + ABG disturbances + Decreased peristalsis (Decreased/Absent bowel sounds) + Jaundice + Encephalopathy + Increased ALT, AST + Decreased K+ + Increased BUN + Increased Creatinine + Decreased U/O Patient Outcomes: Shock, Sepsis, and MODS + Improve tissue perfusion to major organs + Improved LOC (Alert, oriented) + Normotensive + Warm, dry skin + Adequate U/O + Normal Hemodynamics + Normal Lab values + Absence of infection + Intact skin [Show More]
Last updated: 3 years ago
Preview 1 out of 54 pages
Buy this document to get the full access instantly
Instant Download Access after purchase
Buy NowInstant download
We Accept:

Reviews( 0 )
$16.00
Can't find what you want? Try our AI powered Search
Document information
Connected school, study & course
About the document
Uploaded On
Sep 24, 2022
Number of pages
54
Written in
All
Additional information
This document has been written for:
Uploaded
Sep 24, 2022
Downloads
0
Views
131