Documentation / Electronic Health Record
Document: Provider Notes
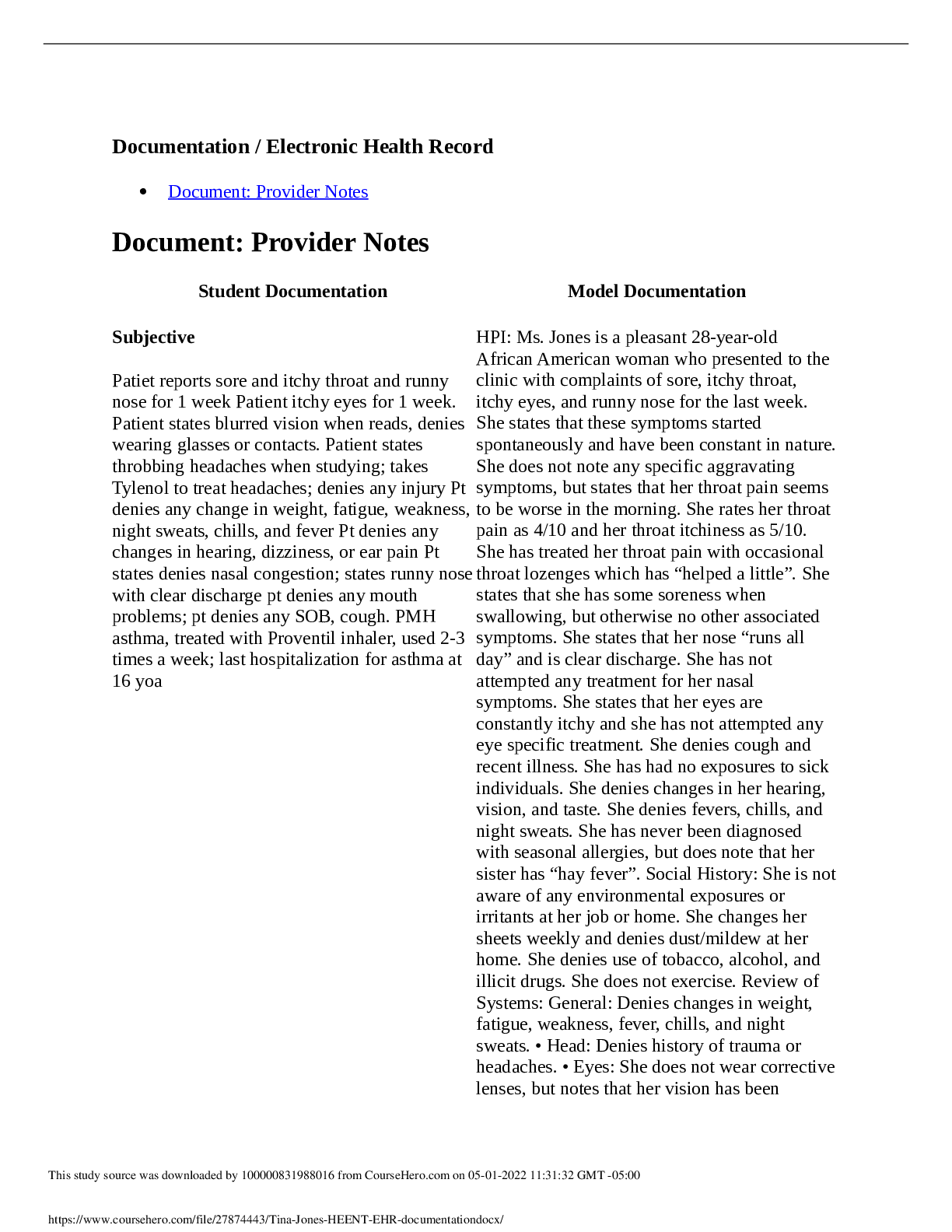
Document: Provider Notes
Student Documentation Model Documentation
Subjective
Patiet reports sore and itchy throat and runny
nose for 1 week Patie
...
Documentation / Electronic Health Record
Document: Provider Notes
Document: Provider Notes
Student Documentation Model Documentation
Subjective
Patiet reports sore and itchy throat and runny
nose for 1 week Patient itchy eyes for 1 week.
Patient states blurred vision when reads, denies
wearing glasses or contacts. Patient states
throbbing headaches when studying; takes
Tylenol to treat headaches; denies any injury Pt
denies any change in weight, fatigue, weakness,
night sweats, chills, and fever Pt denies any
changes in hearing, dizziness, or ear pain Pt
states denies nasal congestion; states runny nose
with clear discharge pt denies any mouth
problems; pt denies any SOB, cough. PMH
asthma, treated with Proventil inhaler, used 2-3
times a week; last hospitalization for asthma at
16 yoa
HPI: Ms. Jones is a pleasant 28-year-old
African American woman who presented to the
clinic with complaints of sore, itchy throat,
itchy eyes, and runny nose for the last week.
She states that these symptoms started
spontaneously and have been constant in nature.
She does not note any specific aggravating
symptoms, but states that her throat pain seems
to be worse in the morning. She rates her throat
pain as 4/10 and her throat itchiness as 5/10.
She has treated her throat pain with occasional
throat lozenges which has “helped a little”. She
states that she has some soreness when
swallowing, but otherwise no other associated
symptoms. She states that her nose “runs all
day” and is clear discharge. She has not
attempted any treatment for her nasal
symptoms. She states that her eyes are
constantly itchy and she has not attempted any
eye specific treatment. She denies cough and
recent illness. She has had no exposures to sick
individuals. She denies changes in her hearing,
vision, and taste. She denies fevers, chills, and
night sweats. She has never been diagnosed
with seasonal allergies, but does note that her
sister has “hay fever”. Social History: She is not
aware of any environmental exposures or
irritants at her job or home. She changes her
sheets weekly and denies dust/mildew at her
home. She denies use of tobacco, alcohol, and
illicit drugs. She does not exercise. Review of
Systems: General: Denies changes in weight,
fatigue, weakness, fever, chills, and night
sweats. • Head: Denies history of trauma or
headaches. • Eyes: She does not wear corrective
lenses, but notes that her vision has been
This study source was downloaded by 100000831988016 from CourseHero.com on 05-01-2022 11:31:32 GMT -05:00
https://www.coursehero.com/file/27874443/Tina-Jones-HEENT-EHR-documentationdocx/
Student Documentation Model Documentation
worsening over the past few years. She
complains of blurry vision after reading for
extended periods. Denies increased tearing or
itching prior to this past week. • Ears: Denies
hearing loss, tinnitus, vertigo, discharge, or
earache. • Nose/Sinuses: Denies rhinorrhea
prior to this episode. Denies stuffiness,
sneezing, itching, previous allergy, epistaxis, or
sinus pressure. • Mouth/Throat: Denies bleeding
gums, hoarseness, swollen lymph nodes, or
wounds in mouth. No sore throat prior to this
episode. • Respiratory: She denies shortness of
breath, wheezing, cough, sputum, hemoptysis,
pneumonia, bronchitis, emphysema,
tuberculosis. She has a history of asthma, last
hospitalization was age 16 for asthma, last chest
XR was age 16. Her current inhaler use has
been her baseline of 2-3 times per week.
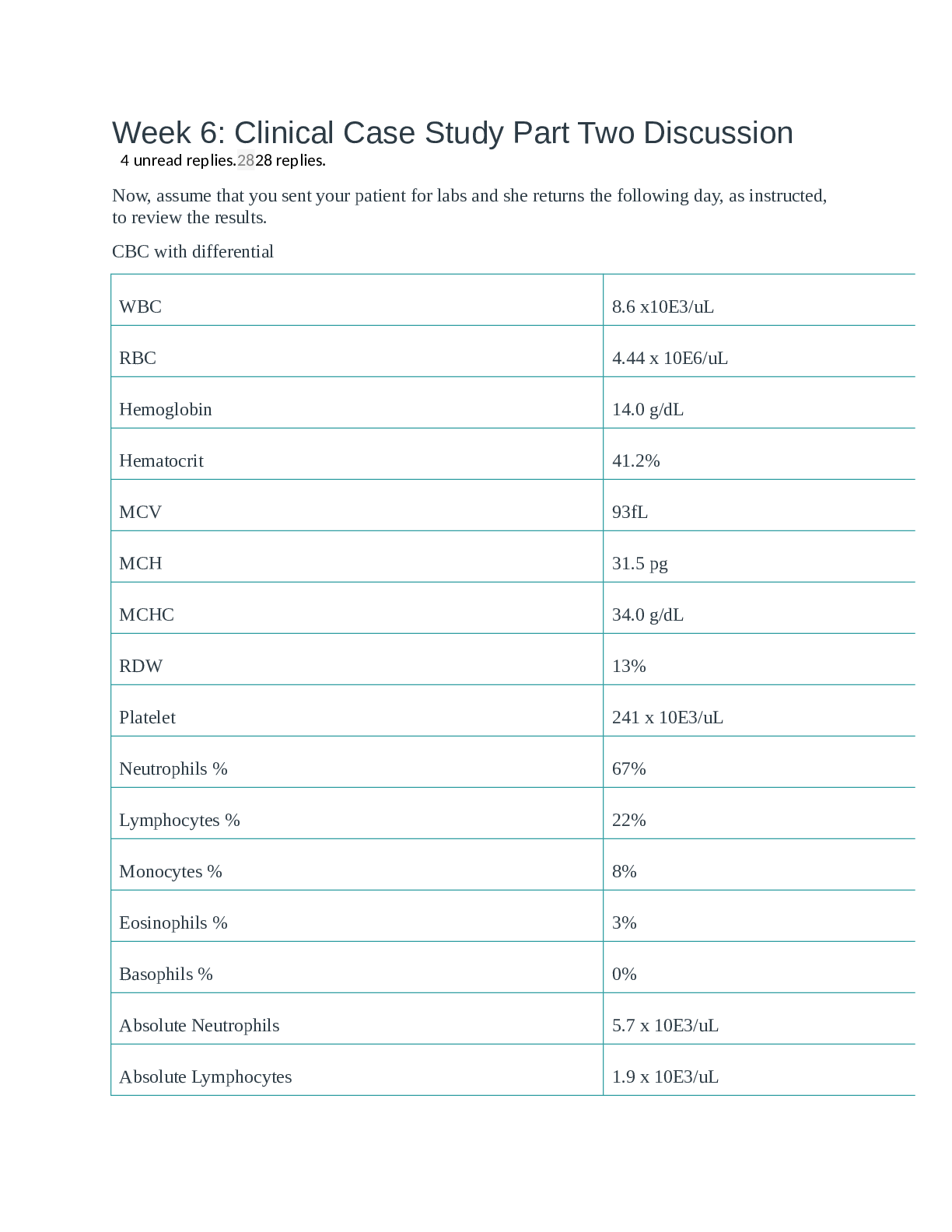
Objective
Acne on right side face oropharynx
erythematous with mild cobblestoning, post
nasal discharge nasal mucosa pale injection
noted on sclera visulal acuity: 20/40 right eye,
20/20 left eye
General: Ms. Jones is a pleasant, obese 28-yearold African American woman in no acute
distress. She is alert and oriented. She maintains
eye contact throughout interview and
examination. • Head: Head is normocephalic
and atraumatic. Scalp with no masses, normal
hair distribution. • Eyes: Bilateral eyes with
equal hair distribution, no lesions, no ptosis, no
edema, conjunctiva clear and injected.
Extraocular movements intact bilaterally. Pupils
equal, round, and reactive to light bilaterally.
Normal convergence. Left fundoscopic exam
reveals sharp disc margins, no hemorrhages.
Right fundoscopic exam reveals mild
retinopathic changes. Left eye vision: 20/20.
Right eye vision: 20/40. • Ears: Ear shape equal
bilaterally. External canals without
inflammation bilaterally. Tympanic membranes
pearly grey and intact with positive light reflex
bilaterally. Rinne, Weber, and Whisper tests
normal bilaterally. • Nose: Septum is midline,
nasal mucosa is boggy and pale bilaterally. No
pain with palpation of frontal or maxillary
sinuses. • Mouth/Throat: Moist buccal mucosa,
This study source was downloaded by 100000831988016 from CourseHero.com on 05-01-2022 11:31:32 GMT -05:00
https://www.coursehero.com/file/27874443/Tina-Jones-HEENT-EHR-documentationdocx/
Student Documentation Model Documentation
no wounds visualized. Adequate dental hygiene.
Uvula midline. Tonsils 1+ and without evidence
of inflammation. Posterior pharynx is slightly
erythematous with mild cobblestoning. •Neck:
No cervical, infraclavicular lymphadenopathy.
Thyroid is smooth without nodules or goiter.
Acanthosis nigricans present. Carotid pulses 2+,
no thrills. Jaw with no clicks, full range of
motion. Bilateral carotid artery auscultation
without bruit. • Respiratory: Chest is
symmetrical with respirations. Lung sounds
clear to auscultation without wheezes, crackles,
or cough.
Assessment
Allergic Rhinitis
Allergic Rhinitis
Plan
Claritin 10mg by mouth daily encourage to
increase fluid intake Avoid allergy triggers
Come back when symptoms are worsening such
as uncontrolled nose bleedin, fever, headaches
follow up within 1 month for evaluation
Encourage Ms. Jones to continue to monitor
symptoms and log her episodes of allergic
symptoms with associated factors and bring log
to next visit. • Initiate trial of loratadine
(Claritin) 10 mg by mouth daily. • Encourage to
increase intake of water and other fluids and
educate on frequent handwashing. • Educate on
avoidance of triggers and known allergens •
Educate Ms. Jones on when to seek care
including episodes of uncontrollable epistaxis,
worsening headache, or fever. • Revisit clinic in
2-4 weeks for follow up and evaluation.
[Show More]