1137 Final Study Guide
1. Clinical
Judgment #1,2,3
Clinical Judgment
Tanner’s Clinical Model
Knowledge Safe and Effective Care
Environment:
Management of Care
Nursing Process Tanner
A class of nursing students i
...
1137 Final Study Guide
1. Clinical
Judgment #1,2,3
Clinical Judgment
Tanner’s Clinical Model
Knowledge Safe and Effective Care
Environment:
Management of Care
Nursing Process Tanner
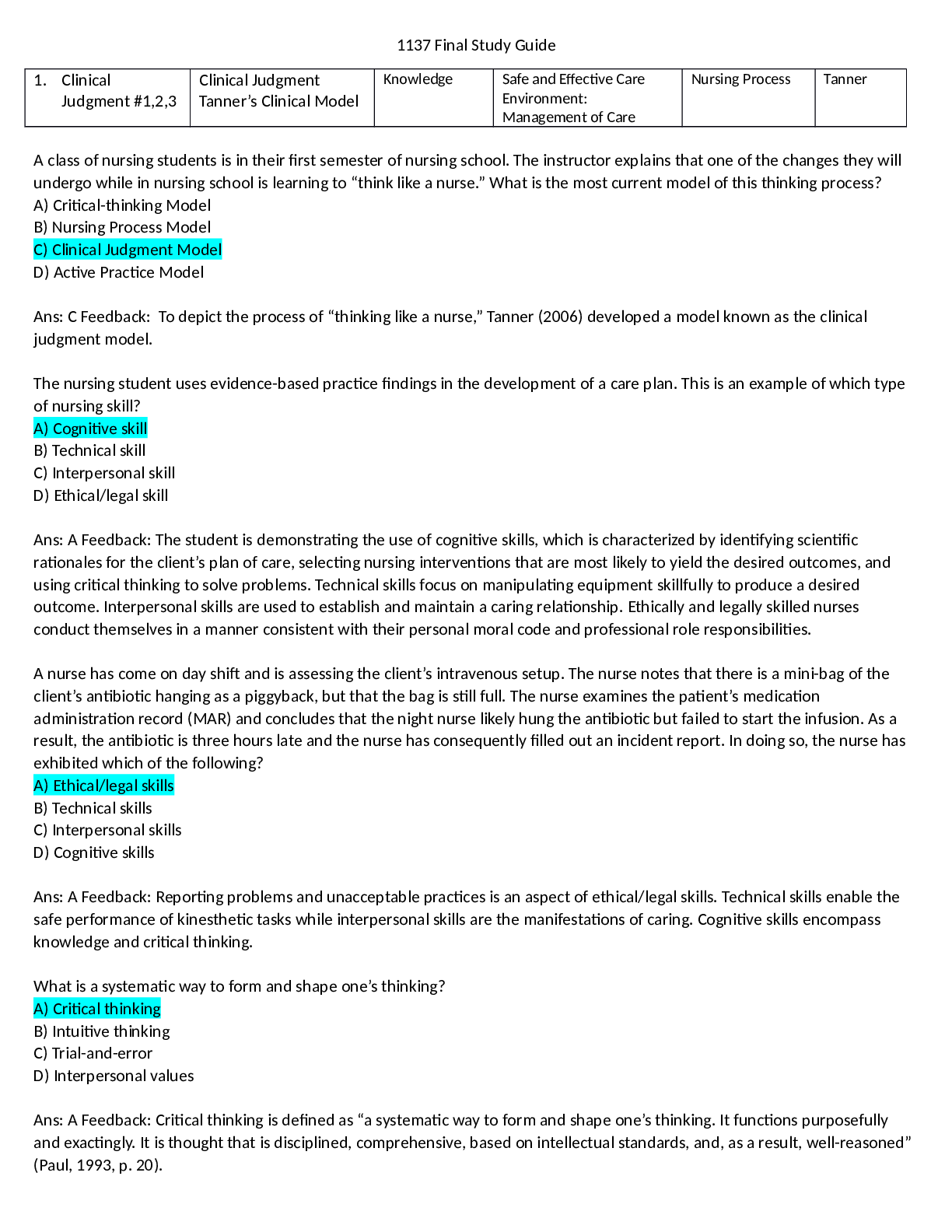
A class of nursing students is in their first semester of nursing school. The instructor explains that one of the changes they will
undergo while in nursing school is learning to “think like a nurse.” What is the most current model of this thinking process?
A) Critical-thinking Model
B) Nursing Process Model
C) Clinical Judgment Model
D) Active Practice Model
Ans: C Feedback: To depict the process of “thinking like a nurse,” Tanner (2006) developed a model known as the clinical
judgment model.
The nursing student uses evidence-based practice findings in the development of a care plan. This is an example of which type
of nursing skill?
A) Cognitive skill
B) Technical skill
C) Interpersonal skill
D) Ethical/legal skill
Ans: A Feedback: The student is demonstrating the use of cognitive skills, which is characterized by identifying scientific
rationales for the client’s plan of care, selecting nursing interventions that are most likely to yield the desired outcomes, and
using critical thinking to solve problems. Technical skills focus on manipulating equipment skillfully to produce a desired
outcome. Interpersonal skills are used to establish and maintain a caring relationship. Ethically and legally skilled nurses
conduct themselves in a manner consistent with their personal moral code and professional role responsibilities.
A nurse has come on day shift and is assessing the client’s intravenous setup. The nurse notes that there is a mini-bag of the
client’s antibiotic hanging as a piggyback, but that the bag is still full. The nurse examines the patient’s medication
administration record (MAR) and concludes that the night nurse likely hung the antibiotic but failed to start the infusion. As a
result, the antibiotic is three hours late and the nurse has consequently filled out an incident report. In doing so, the nurse has
exhibited which of the following?
A) Ethical/legal skills
B) Technical skills
C) Interpersonal skills
D) Cognitive skills
Ans: A Feedback: Reporting problems and unacceptable practices is an aspect of ethical/legal skills. Technical skills enable the
safe performance of kinesthetic tasks while interpersonal skills are the manifestations of caring. Cognitive skills encompass
knowledge and critical thinking.
What is a systematic way to form and shape one’s thinking?
A) Critical thinking
B) Intuitive thinking
C) Trial-and-error
D) Interpersonal values
Ans: A Feedback: Critical thinking is defined as “a systematic way to form and shape one’s thinking. It functions purposefully
and exactingly. It is thought that is disciplined, comprehensive, based on intellectual standards, and, as a result, well-reasoned”
(Paul, 1993, p. 20).
What step in the nursing process is most closely associated with cognitively skilled nurses?
A) Assessing
B) Planning
C) Implementing
D) Evaluating
Ans: B Feedback: Cognitively skilled nurses are critical thinkers and are able to select those nursing interventions that are most
likely to yield the desired outcomes.
Members of the staff on a hospital unit are critical of a client’s family, who has different cultural beliefs about health and illness.
A student assigned to the patient does not agree, based on her care of the client and family. What critical thinking attitude is
the student demonstrating?
A) Being curious and persevering
B) Being creative
C) Demonstrating confidence
D) Thinking independently
Ans: D Feedback: Although all the attitudes listed are components of critical thinking, the student is thinking independently.
Nurses who are independent thinkers are careful not to let the status quo or a persuasive individual control their thinking.
Excerpts from Tanner:
Research on nursing work in acute care environments has shown how contextual factors profoundly influence nursing
judgment. Ebright et al. (2003) found that nursing judgments made during actual work are driven by more than textbook
knowledge; they are influenced by knowledge of the unit and routine workflow, as well as by specific patient details that help
nurses prioritize tasks. Benner, Tanner, and Chesla (1997) described the social embeddedness of nursing knowledge, derived
from observations of nursing practice and interpretation of narrative accounts, drawn from multiple units and hospitals.
Benner’s and Ebright’s work provides evidence for the significance of the social groups style, habits and culture in shaping what
situations require nursing judgment, what knowledge is valued, and what perceptual skills are taught. A number of studies
clearly demonstrate the effects of the political and social context on nursing judgment. Interdisciplinary relationships, notably
status inequities and power differentials between nurses and physicians, contribute to nursing judgments in the degree to
which the nurse both pursues understanding a problem and is able to intervene effectively (Benner et al., 1996; Bucknall &
Thomas, 1997). The literature on pain management confirms the enormous influence of these factors in adequate pain control
(Abu-Saad & Hamers, 1997). Studies have indicated that decisions to test and treat are associated with patient factors, such as
socioeconomic status (Scott, Schiell, & King, 1996). However, others have suggested that social judgment or moral evaluation of
patients is socially embedded, independent of patient characteristics, and as much a function of the pervasive norms and
attitudes of particular nursing units (Grieff & Elliot, 1994; Johnson & Webb, 1995; Lauri et al., 2001; McCarthy, 2003a;
McDonald et al., 2003).
In this model, noticing is not a necessary outgrowth of the first step of the nursing process: assessment. Instead, it is a function
of nurses’ expectations of the situation, whether or not they are made explicit. These expectations stem from nurses’
knowledge of the particular patient and his or her patterns of responses; their clinical or practical knowledge of similar
patients, drawn from experience; and their textbook knowledge. For example, a nurse caring for a postoperative patient whom
she has cared for over time will know the patient’s typical pain levels and responses. Nurses experienced in postoperative care
will also know the typical pain response for this population of patients and will understand the physiological and
Clinical Judgment/
Tanner’s Clinical Model
First test was Noticing -recognizing a potential issue, perceptually grasping
situation
Tanners clinical judgment model Remembering
Remembering = Reflecting: attending to patient’s responses to nursing action
while in the process of acting
Reflection on action and clinical learning, breakdown in clinical judgement
which is critical in developing clinical knowledge and improvement of clinical
reasoning (incorporation of skills and clinical knowledge in patient situations)
“Thinking Like A Nurse”
(2006)
Clinical Judgment Model
208
pathophysiological mechanisms for pain in surgeries like this. These understandings will collectively shape the nurse’s
expectations for this patient and his pain levels, setting up the possibility of noticing whether those expectations are met. Other
factors will also influence nurses’ noticing of a change in the clinical situation that demands attention, including nurses’ vision
of excellent practice, their values related to the particular patient situation, the culture on the unit and typical patterns of care
on that unit, and the complexity of the work environment. The factors that shape nurses’ noticing, and, hence, initial grasp, are
shown on the left side of the Figure.
*Deciding on a course of action deemed appropriate for the situation, which may include “no immediate action,” termed
“responding.”
*Attending to patients’ responses to the nursing action while in the process of acting, termed “reflecting.”
*Reviewing the outcomes of the action, focusing on the appropriateness of all of the preceding aspects (i.e., what was noticed,
how it was interpreted, and how the nurse responded).
Conclusions Thinking like a nurse, as described by this model, is a form of engaged moral reasoning. Expert nurses enter the
care of particular patients with a fundamental sense of what is good and right and a vision for what makes exquisite care.
Educational practices must, therefore, help students engage with patients and act on a responsible vision for excellent care of
those patients and with a deep concern for the patients’ and families’ well-being. Clinical reasoning must arise from this
engaged, concerned stance, always in relation to a particular patient and situation and informed by generalized knowledge and
rational processes, but never as an objective, detached exercise with the patient’s concerns as a sidebar. If we, as nurse
educators, help our students understand and develop as moral agents, advance their clinical knowledge through expert
guidance and coaching, and become habitual in reflection on-practice, they will have learned to think like a nurse.
Blueprint note: Research based on Tanners clinical judgement
Noticing -recognizing a potential issue, perceptually grasping situation
Interpreting: reasoning pattern, analytic, intuitive, narrative, developing a sufficient
understanding of the situation
Observation and interpretation are hallmarks of trained nursing practice
Responding: deciding on the court of action deemed appropriate for the situation, which
may include, no immediate action
Reflecting: attending to patient’s responses to nursing action while in the process of
acting
Blueprint note: Know what clinical judgement model is?
Which model is relevant?
Clinical judgement model
Supports the idea that nurses engage in a complex process of clinical reasoning when
caring for patients. Nurses draw on personal knowledge and experience from various
situations and consider the contextual background of the clinical culture.
Blueprint note: Effective use of clinical judgement, center of the process
Critical Thinking is the center of the process for clinical judgement
This article reviews the growing body of research on clinical judgment in nursing and presents an alternative model of clinical
judgment based on these studies. Based on a review of nearly 200 studies, five conclusions can be drawn: (1) Clinical
judgments are more influenced by what nurses bring to the situation than the objective data about the situation at hand; (2)
Sound clinical judgment rests to some degree on knowing the patient and his or her typical pattern of responses, as well as an
engagement with the patient and his or her concerns; (3) Clinical judgments are influenced by the context in which the
situation occurs and the culture of the nursing care unit; (4) Nurses use a variety of reasoning patterns alone or in combination;
and (5) Reflection on practice is often triggered by a breakdown in clinical judgment and is critical for the development of
clinical knowledge and improvement in clinical reasoning. A model based on these general conclusions emphasizes the role of
nurses’ background, the context of the situation, and nurses’ relationship with their patients as central to what nurses notice
and how they interpret findings, respond, and reflect on their response.
Reflection-in-action and reflection-on-action together comprise a significant component of the model. Reflection in-action
refers to nurses’ ability to “read” the patient—how he or she is responding to the nursing intervention—and adjust the
interventions based on that assessment. Much of this reflection-in-action is tacit and not obvious, unless there is a breakdown
in which the expected outcomes of nurses’ responses are not achieved. Reflection-on-action and subsequent clinical learning
completes the cycle; showing what nurses gain from their experience contributes to their ongoing clinical knowledge
development and their capacity for clinical judgment in future situations. As in any situation of uncertainty requiring
judgment, there will be judgment calls that are insightful and astute and those that result in horrendous errors. Each situation
is an opportunity for clinical learning, given a supportive context and nurses who have developed the habit and skill of
reflection-on-practice. To engage in reflection requires a sense of responsibility, connecting one’s actions with outcomes.
Reflection also requires knowledge outcomes: knowing what occurred as a result of nursing actions.
[Show More]