Module 3 Knowledge Check: GI and Hepatobiliary Disorders:
A 45-year-old male comes to the clinic with a chief complaint of epigastric abdominal pain that
has persisted for 2 weeks. He describes the pain as burning, non
...
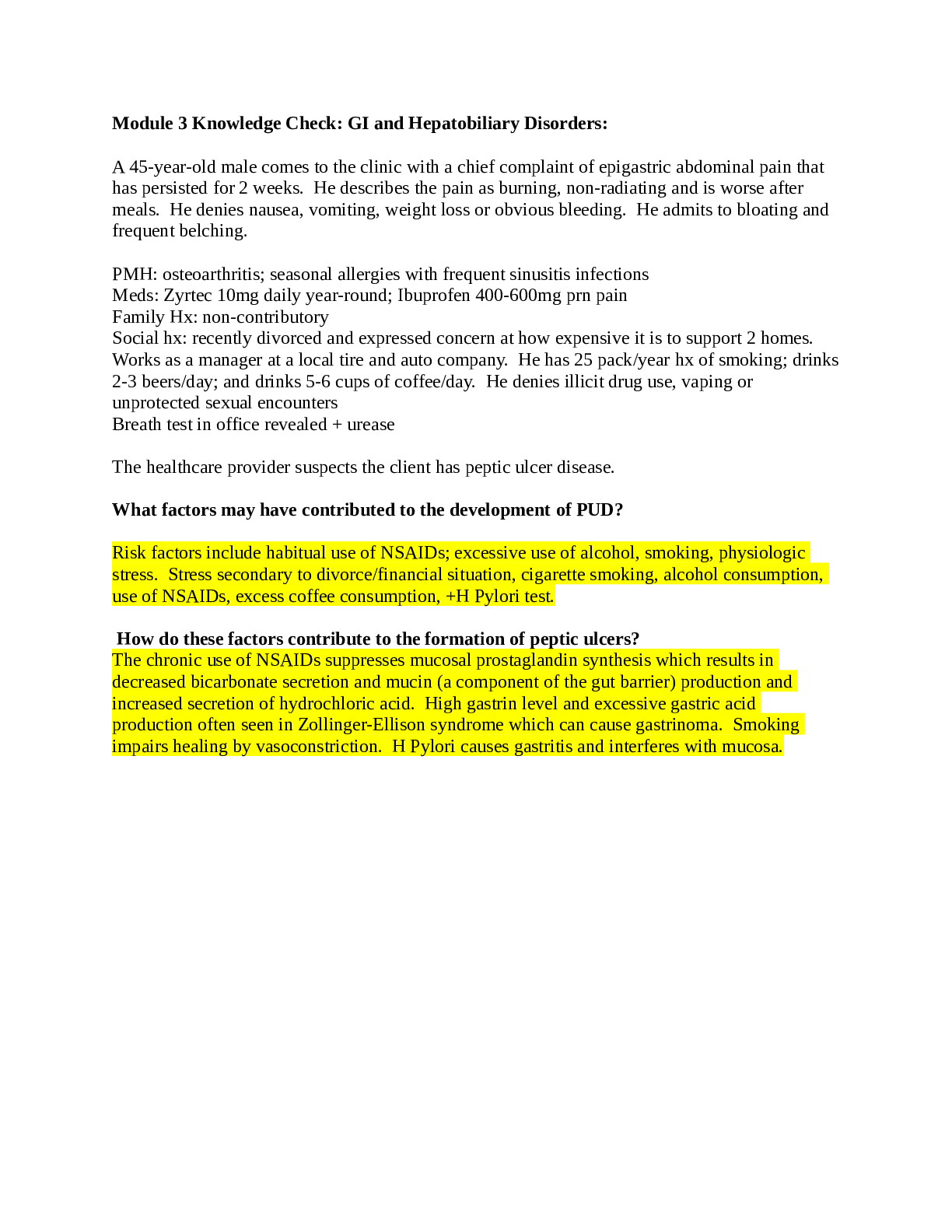
Module 3 Knowledge Check: GI and Hepatobiliary Disorders:
A 45-year-old male comes to the clinic with a chief complaint of epigastric abdominal pain that
has persisted for 2 weeks. He describes the pain as burning, non-radiating and is worse after
meals. He denies nausea, vomiting, weight loss or obvious bleeding. He admits to bloating and
frequent belching.
PMH: osteoarthritis; seasonal allergies with frequent sinusitis infections
Meds: Zyrtec 10mg daily year-round; Ibuprofen 400-600mg prn pain
Family Hx: non-contributory
Social hx: recently divorced and expressed concern at how expensive it is to support 2 homes.
Works as a manager at a local tire and auto company. He has 25 pack/year hx of smoking; drinks
2-3 beers/day; and drinks 5-6 cups of coffee/day. He denies illicit drug use, vaping or
unprotected sexual encounters
Breath test in office revealed + urease
The healthcare provider suspects the client has peptic ulcer disease.
What factors may have contributed to the development of PUD?
Risk factors include habitual use of NSAIDs; excessive use of alcohol, smoking, physiologic
stress. Stress secondary to divorce/financial situation, cigarette smoking, alcohol consumption,
use of NSAIDs, excess coffee consumption, +H Pylori test.
How do these factors contribute to the formation of peptic ulcers?
The chronic use of NSAIDs suppresses mucosal prostaglandin synthesis which results in
decreased bicarbonate secretion and mucin (a component of the gut barrier) production and
increased secretion of hydrochloric acid. High gastrin level and excessive gastric acid
production often seen in Zollinger-Ellison syndrome which can cause gastrinoma. Smoking
impairs healing by vasoconstriction. H Pylori causes gastritis and interferes with mucosa.
A 36-year-old morbidly obese female comes to the office with a chief complaint of “burning in
my chest and a funny taste in my mouth.” The symptoms have been present for years but patient
states she had been treating them with antacid tablets which helped until the last 4 or 5 weeks.
She never saw a healthcare provider for that. She says the symptoms get worse at night when
she is lying down and has had to sleep with 2 pillows. She says she has started coughing at night
which has been interfering with her sleep. She denies palpitations, shortness of breath or nausea.
PMH: HTN; venous stasis ulcers; IBS; OA of knees; morbid obesity
Family hx: non-contributory
Meds: Amlodipine 10mg QD; Dicyclomine 20mg QD; Motrin 600mg q6hrs prn
Social: 15 pack/year hx of smoking; occasional alcohol use; denies vaping
The healthcare provider diagnoses the patient with GERD.
The client asks the APRN what causes GERD. What is the APRN’s best response?
GERD manifestations result directly from gastric acid reflux into the esophagus. Pyrosis, the
classic symptom, is a substernal burning sensation typically described as heartburn. It may be
accompanied by regurgitation, particularly in someone who has recently eaten. The lower
esophageal sphincter (LES) relaxes due to certain meds (calcium channel blockers), hiatal hernia,
and obesity allows stomach contents to enter the lower esophagus causing inflammation and
possibly erosion of the esophagus.
A 34-year-old construction worker presents to his PCP with a chief complaint of passing foul
smelling dark, tarry stools. He stated the first episode occurred last week, but it was only a small
amount after he had eaten a dinner of beets and beef. The episode today was accompanied by
nausea, sweating, and weakness. He states he has had some mid epigastric pain for several
weeks and has been taking OTC antacids. The most likely diagnosis is upper GI bleed which
won’t be confirmed until further endoscopic procedures are performed.
What factors can contribute to an upper GI bleed?
UGI bleeds can be caused by PUD which remains the most common cause. Esophageal bleeding
from a Mallory-Weiss tear (caused by repeated vomiting, retching, erosions of the mucosa),
gastric carcinomas.
A 64-year-old steel worker presents to his PCP with a chief complaint of passing bright red blood
when had a BM that morning. He stated
[Show More]