Digestive and Gastrointestinal Treatment Modalities �
Purposes of Gastrointestinal Intubation
Decompress the stomach
Lavage the stomach
Diagnose GI disorders
Administer medications and feeding
To compress a bleedi
...
Digestive and Gastrointestinal Treatment Modalities �
Purposes of Gastrointestinal Intubation
Decompress the stomach
Lavage the stomach
Diagnose GI disorders
Administer medications and feeding
To compress a bleeding site
To aspirate gastric contents for analysis
Types of Tubes
Lavage tubes
Levin
Gastric (Salem) Sump
Enteric tubes
Gastric Sump Tube
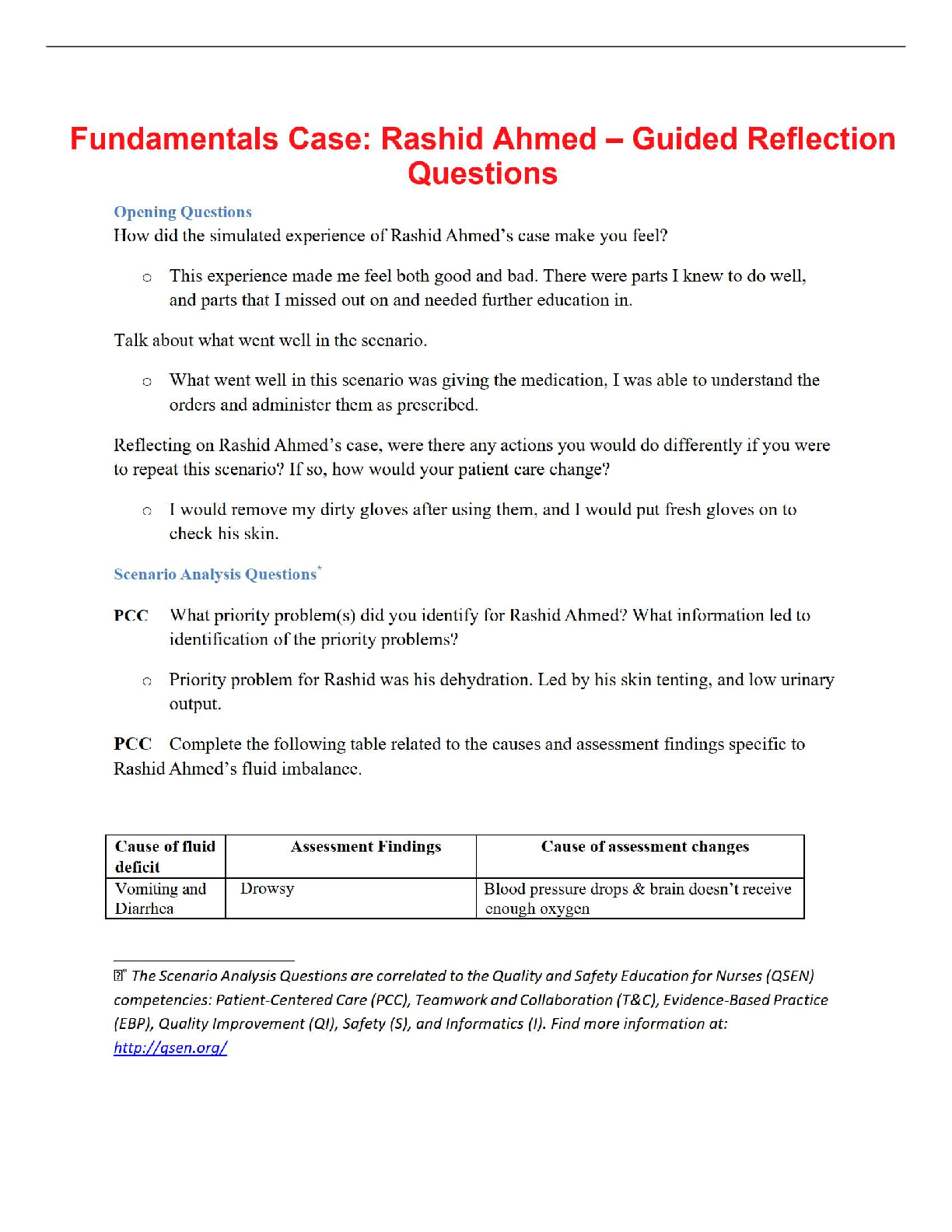
Collaborative Problems and Potential Complications #1
Diarrhea
Nausea and vomiting
Gas, bloating, cramping
Dumping syndrome
Aspiration pneumonia
Tube displacement
Tube obstruction
Nasopharyngeal irritation
Hyperglycemia
Dehydration and azotemia
Maintaining Nutrition Balance and Tube Function
Administer feeding at prescribed rate and method and according to patient tolerance.
Measure gastric residual volumes (GRV) before intermittent feedings and every 4 to 8 hours during continuous feedings
Administer water before and after each medication and each feeding, before and after checking residual, every 4 to 6 hours, and whenever the tube feeding is discontinued or interrupted
Do not mix medications with feedings
Use a 30-mL or 60-mL catheter tip syringe
Maintain delivery system as required. To avoid bacterial contamination, do not hang more than 4 hours of feeding in an open system
Maintaining Normal Bowel Elimination
Selection of TF formula; consider fiber, osmolality, and fluid content
Prevent contamination of TF; maintain closed system; do not hang more than 4 hours TF in an open system
Maintain proper nutritional intake
Assess for reason for diarrhea and obtain treatment as needed
Administer TF slowly to prevent dumping syndrome
Avoid cold TF
Reduce Risk for Aspiration
Elevate head of bed at least 30 to 45 degrees during and for at least 1 hour after feedings
Monitor residual volumes
Stop feedings 1 hour before traveling or placing head down
Other Interventions
Maintain hydration by supplying additional water and assessing for signs of dehydration
Promote coping by support and encouragement; encourage self-care and activities
Frequent oral hygiene
Patient education
Nursing Process: The Care of the Patient With a Gastrostomy or Jejunostomy —Assessment
Patient knowledge and ability to learn
Self-care ability and support
Skin condition
Nutrition and fluid status
Inspection of the tube
Nursing Process: The Care of the Patient With a Gastrostomy or Jejunostomy—Diagnoses
Imbalanced nutrition
Risk of infection
Risk for impaired skin integrity
Disturbed body image
Collaborative Problems and Potential Complications #2
Wound infection, cellulitis, leakage
GI bleeding
Premature dislodgment of tube
[Show More]
.png)