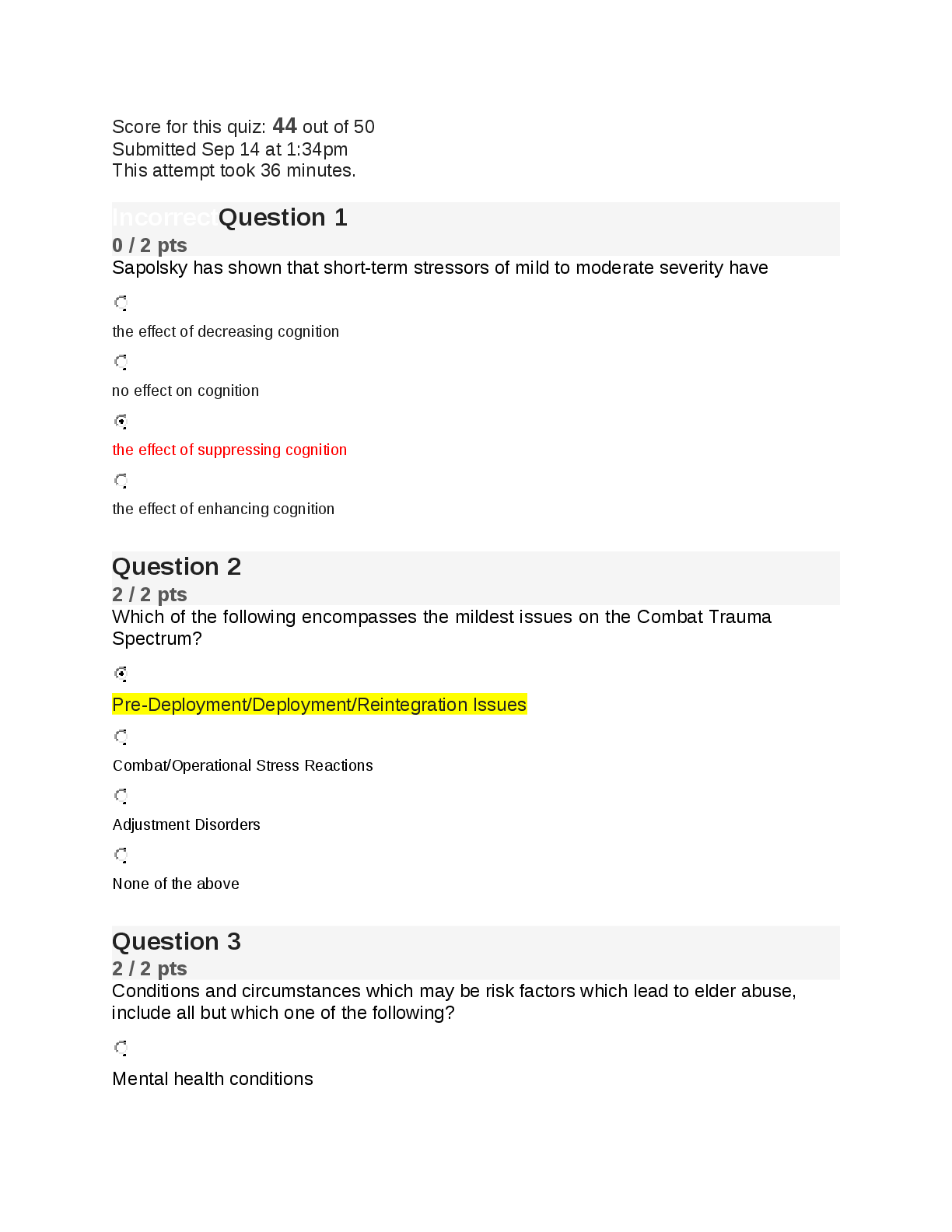
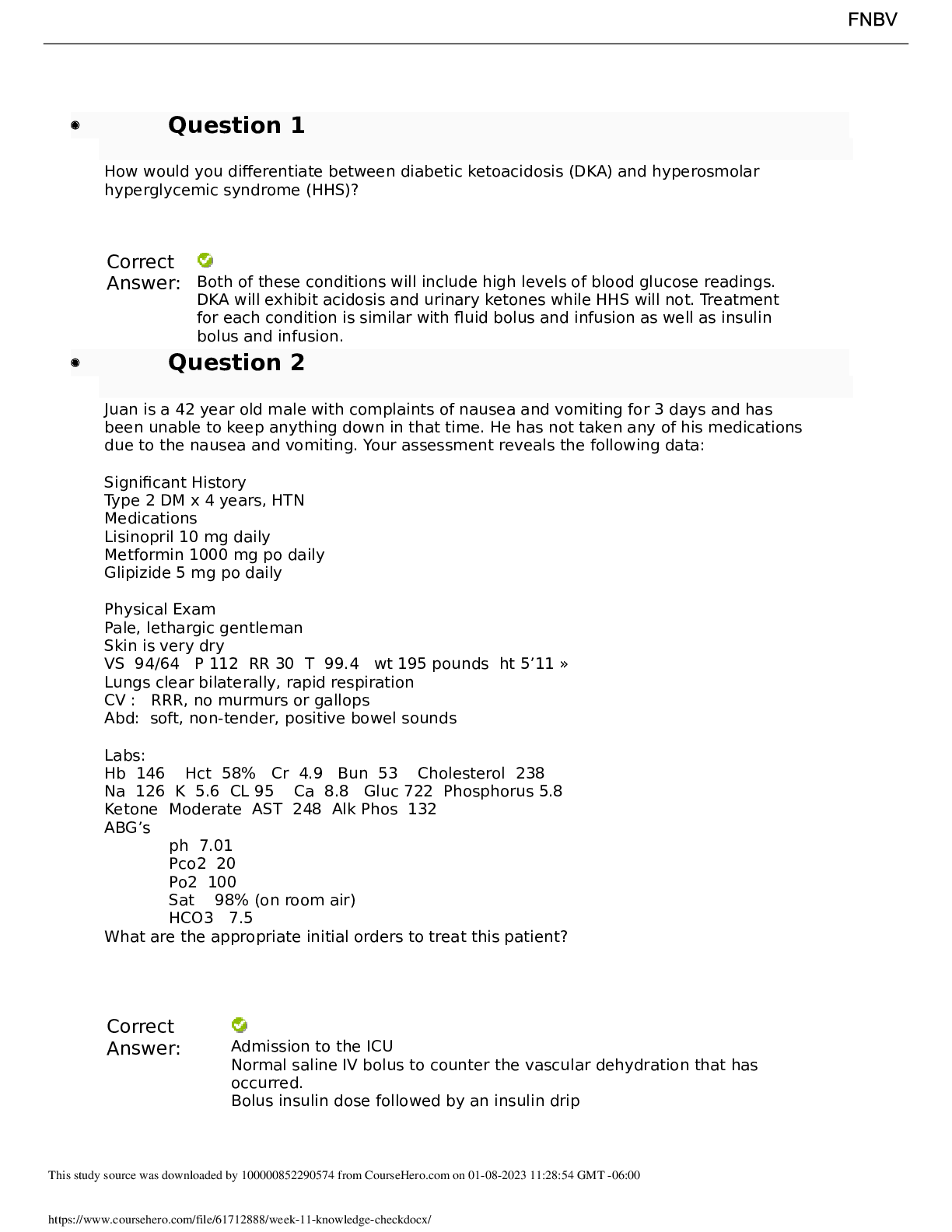
How would you differentiate between diabetic ketoacidosis (DKA) and hyperosmolar
hyperglycemic syndrome (HHS)?
Correct
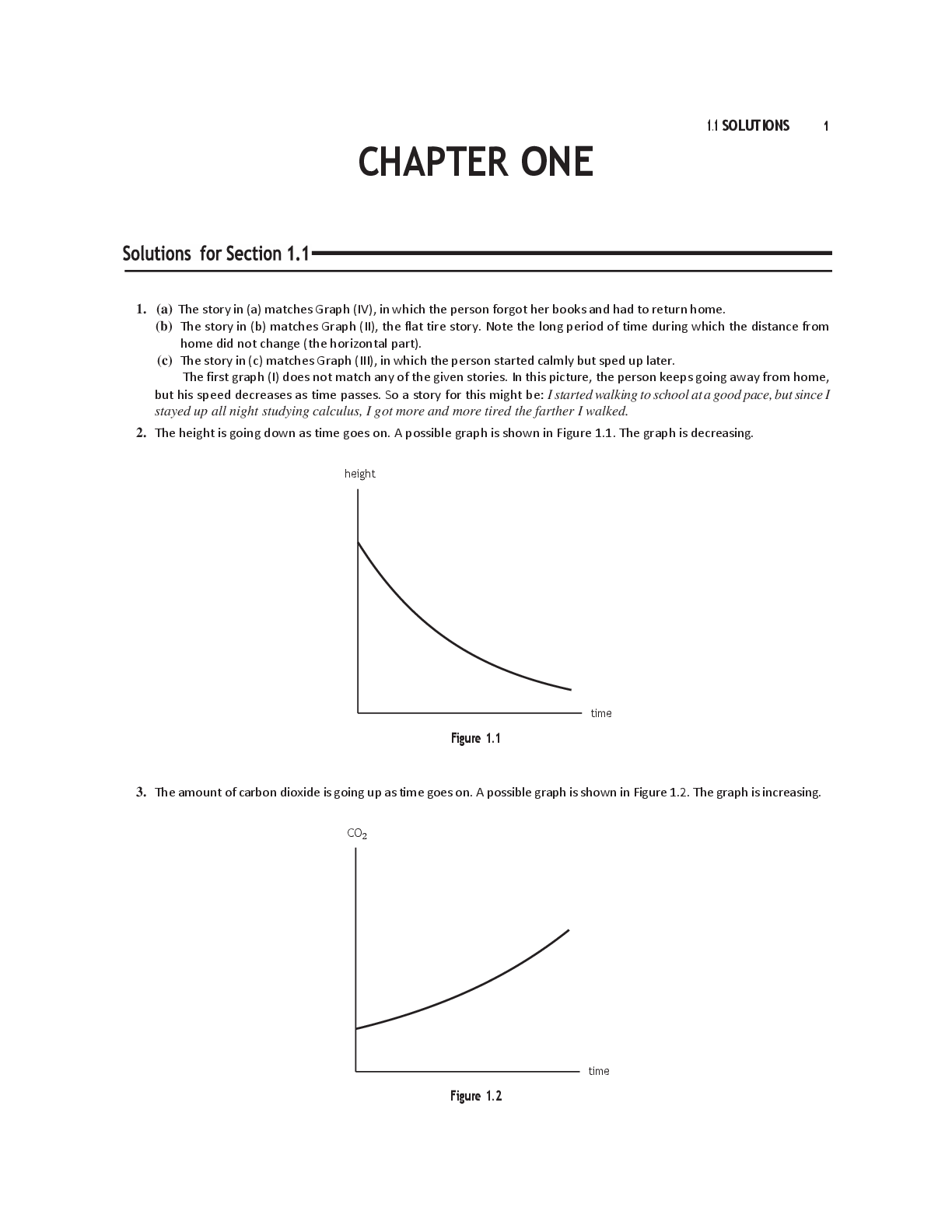
Answer: Both of these conditions will include high levels of blood glucose readings.
DKA will exh
...
How would you differentiate between diabetic ketoacidosis (DKA) and hyperosmolar
hyperglycemic syndrome (HHS)?
Correct
Answer: Both of these conditions will include high levels of blood glucose readings.
DKA will exhibit acidosis and urinary ketones while HHS will not. Treatment
for each condition is similar with fluid bolus and infusion as well as insulin
bolus and infusion.
Question 2
Juan is a 42 year old male with complaints of nausea and vomiting for 3 days and has
been unable to keep anything down in that time. He has not taken any of his medications
due to the nausea and vomiting. Your assessment reveals the following data:
Significant History
Type 2 DM x 4 years, HTN
Medications
Lisinopril 10 mg daily
Metformin 1000 mg po daily
Glipizide 5 mg po daily
Physical Exam
Pale, lethargic gentleman
Skin is very dry
VS 94/64 P 112 RR 30 T 99.4 wt 195 pounds ht 5’11 »
Lungs clear bilaterally, rapid respiration
CV : RRR, no murmurs or gallops
Abd: soft, non-tender, positive bowel sounds
Labs:
Hb 146 Hct 58% Cr 4.9 Bun 53 Cholesterol 238
Na 126 K 5.6 CL 95 Ca 8.8 Gluc 722 Phosphorus 5.8
Ketone Moderate AST 248 Alk Phos 132
ABG’s
ph 7.01
Pco2 20
Po2 100
Sat 98% (on room air)
HCO3 7.5
What are the appropriate initial orders to treat this patient?
Correct
Answer: Admission to the ICU
Normal saline IV bolus to counter the vascular dehydration that has
occurred.
Bolus insulin dose followed by an insulin drip
This study source was downloaded by 100000852290574 from CourseHero.com on 01-08-2023 11:28:54 GMT -06:00
https://www.coursehero.com/file/61712888/week-11-knowledge-checkdocx/
Electrolyte and blood glucose monitoring frequently fluid resuscitation
and insulin administration.
Bicarbonate is typically not administered unless the pH is below 7
Assess the patient for presence of any infection that may have
precipitated this event
Question 3
Juan is a 42 year old male with complaints of nausea and vomiting for 3 days and has
been unable to keep anything down in that time. He has not taken any of his medications
due to the nausea and vomiting. Your assessment reveals the following data:
Significant History
Type 2 DM x 4 years, HTN
Medications
Lisinopril 10 mg daily
Metformin 1000 mg po daily
Glipizide 5 mg po daily
Physical Exam
Pale, lethargic gentleman
Skin is very dry
VS 94/64 P 112 RR 30 T 99.4 wt 195 pounds ht 5’11 »
Lungs clear bilaterally, rapid respiration
CV : RRR, no murmurs or gallops
Abd: soft, non-tender, positive bowel sounds
Labs:
Hb 146 Hct 58% Cr 4.9 Bun 53 Cholesterol 238
Na 126 K 5.6 CL 95 Ca 8.8 Gluc 722 Phosphorus 5.8
Ketone Moderate AST 248 Alk Phos 132
ABG’s
ph 7.01
Pco2 20
Po2 100
Sat 98% (on room air)
HCO3 7.5
What is the “ corrected” sodium level for the hyperglycemia? What does this mean and
how would it impact your treatment plan for this patient?
Correct
Answer: The equation for corrected sodium is:
Corrected sodium (mEq/L) = measure sodium (mEq/L) + 0.016 {glucose
(mg/dL)-100}.
Juans corrected sodium is 136.
126+ 0.016 {722-100} = 135.95
The measured serum sodium concentration should be corrected for the
hyperglycemia by adding 1.6 mEq per L to the measured sodium value.
Corrected serum sodium concentrations of greater than 140 mE1 per L and
calculated total osmolalities greater than 330 most per kg of water are
This study source was downloaded by 100000852290574 from CourseHero.com on 01-08-2023 11:28:54 GMT -06:00
https://www.coursehero.com/file/61712888/week-11-knowledge-checkdocx/
associated with large fluid deficits.
If the corrected sodium is less than 135 mEq/L, then isotonic saline should be
continued at a rate of 250 to 500 mL/ hour. If the corrected sodium is normal
or elevate, then IV fluid is generally switched to 0.45 normal saline.
Question 4
A 56 year old male with an acute COPD exacerbation is admitted to the ICU. He has type I
diabetes and utilizes NPR and regular insulin twice a day to manage his diabetes. He is
currently taking very little orally due to his shortness of breath. What would the best way
to manage his diabetes and insulin needs in the ICU?
Correct
Answer: According to the American Diabetes Association (2019) guideline, basal long
acting insulin should be administered once a day. Point of care blood glucose
testing should be completed at least four times a day with sliding scale insulin
coverage. The stress of illness will require the need for insulin but the
evolution of the patients condition, varying oral intake, and medications will
cause variations in the patients blood glucose. Point of care testing with
sliding scale coverage along with basal insulin is the most flexible method to
meet the patients insulin needs while in the ICU.
Question 5
A 56 year old male with an acute COPD exacerbation is admitted to the ICU. He has type I
diabetes and utilizes NPR and regular insulin twice a day to manage his diabetes. He is
currently taking very little orally due to his shortness of breath. What is the blood glucose
goal for this patient in the ICU?
Correct
Answer: According to the American Diabetes Association (2019) guideline, pre-prandial
blood glucose control of less than 126 is the goal. Post prandial no greater
than 180. Hyperglycemia is associated with poor outcomes especially in
critical illness. According to the NICE-SUGAR study, patients with goals lower
than this (considered intensive insulin therapy) had increased mortality
[Show More]




.png)