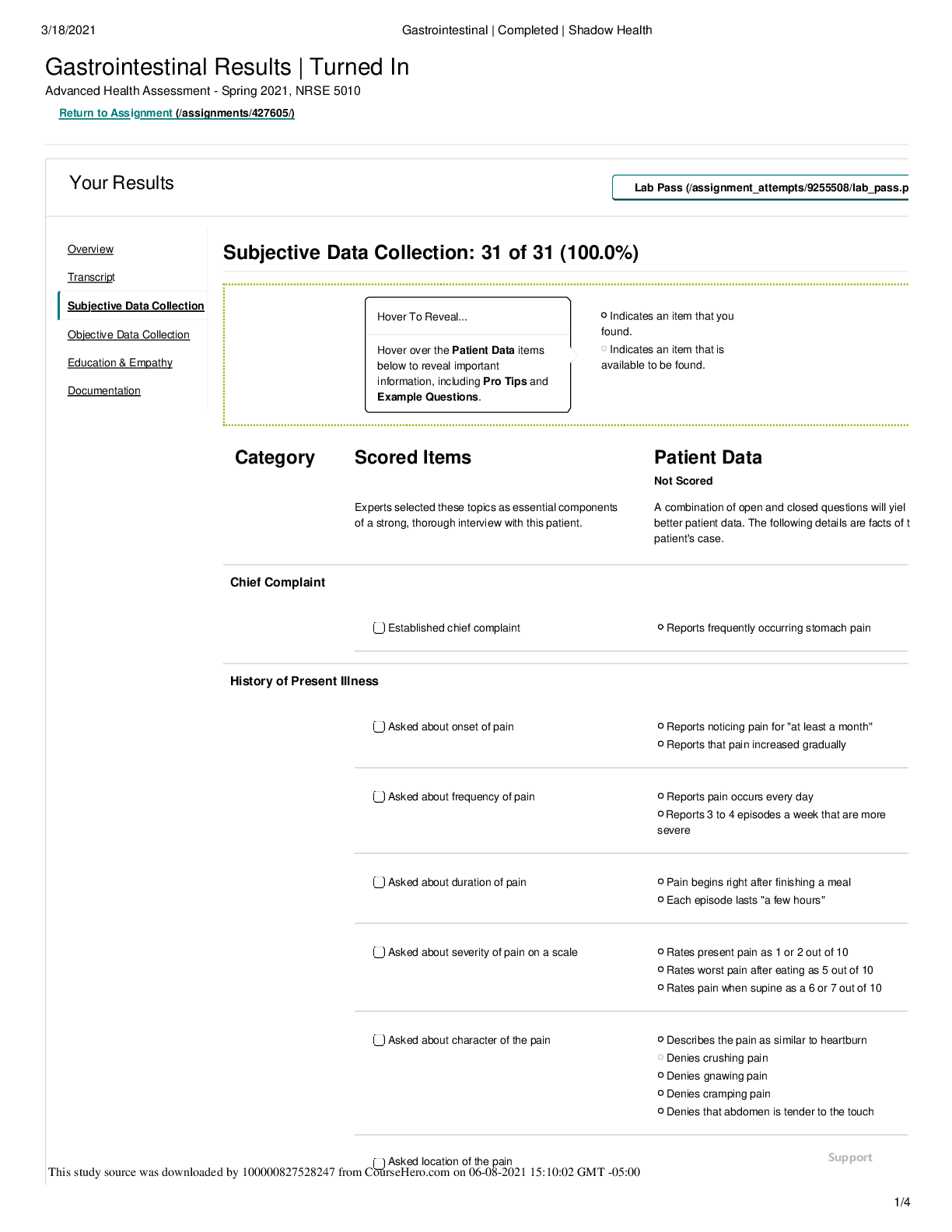
NURS 6512 Week 5 Episodic/Focused SOAP Note Template
NURS 6512 Week 5 Episodic/Focused
SOAP Note Template
Patient Information:
L., 20, F, Caucasian
SUBJECTIVE.
CC: “I have been having sore throat for three da
...
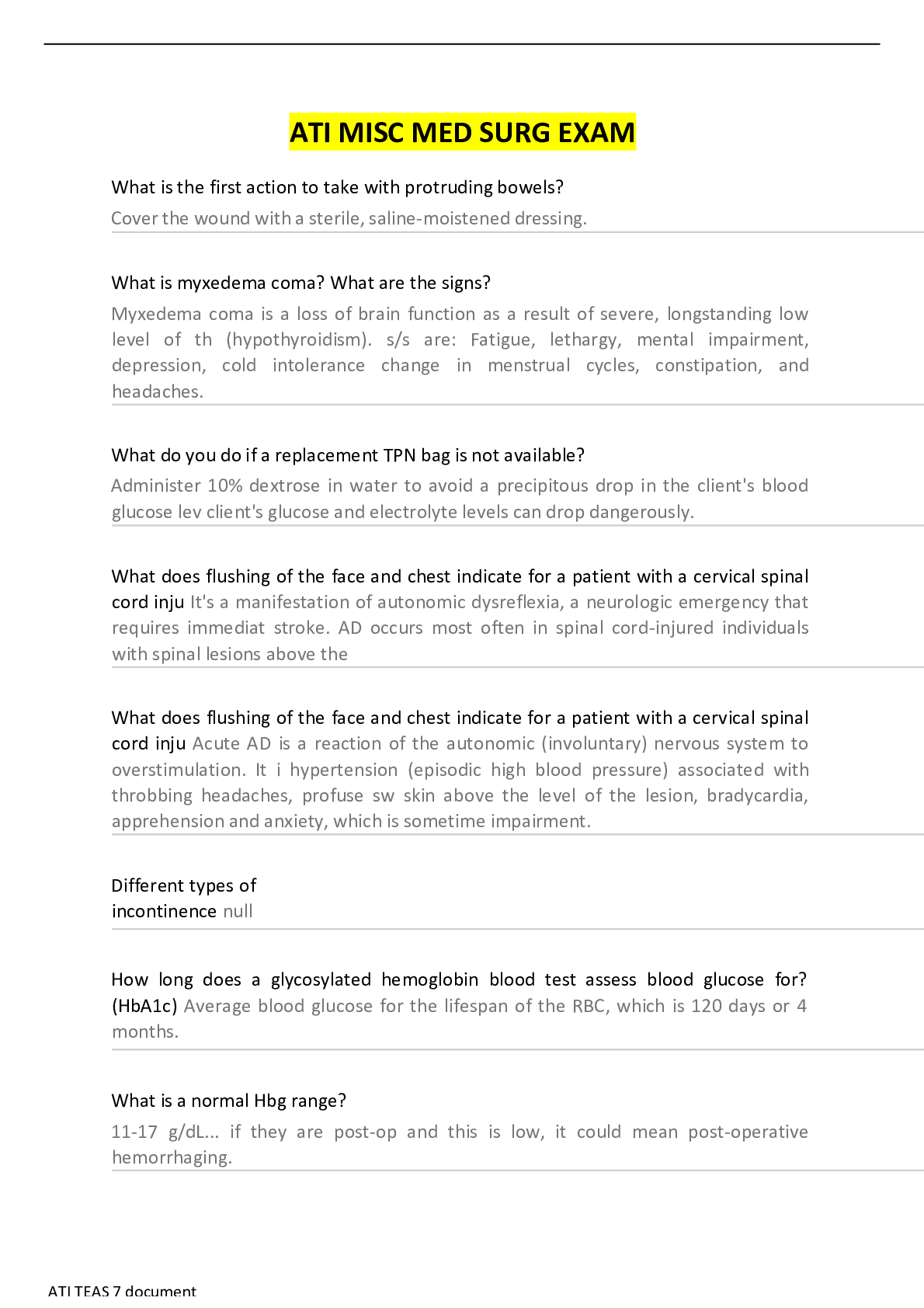
NURS 6512 Week 5 Episodic/Focused SOAP Note Template
NURS 6512 Week 5 Episodic/Focused
SOAP Note Template
Patient Information:
L., 20, F, Caucasian
SUBJECTIVE.
CC: “I have been having sore throat for three days, and I also have decreased appetite, headache,
and pain with swallowing.”
HPI: Ms. L is a 20-year-old female college student who presents with sore throat for three days,
with additional decreased appetite, headache, and pain with swallowing. She recounts that
similar “flu-like” symptoms recently affecting multiple students on campus. Ms. L also noted
runny nose and a slight hoarseness in her voice but doesn't sound congested. She took Tylenol
and Chloraseptic lozenges, but did little for relief.
Location: throat
Onset: 3 days ago
Character: throat is sore
Associated signs and symptoms: decreased appetite, headache, and pain with
swallowing.
Timing: constant
Exacerbating/ relieving factors: light bothers eyes, Tylenol makes it tolerable but not
completely better.
Severity: 8/10 pain scale
Problem-Specific Questions:
Have you been coughing? Any drainage or phlegm? Is it productive, if so how much?
What is the color of the phlegm?
Have you been running a fever or exhibiting chills?
Are you taking any medications for this? Are they helping?
Are you having any pain or pressure in your face, head, or sinuses? Have you recently
had a head injury? Any nasal bleeding noted?Do you smoke or have you been around anyone who smokes?
Do you experience gastroesophageal reflux or heartburn?
Does it hurt to swallow solids, liquids, or both?
Do you feel like something is stuck in your throat?
Do you cough or choke when swallowing?
Do you have any changes in your appetite? Did it start with the onset of your sore throat?
Any changes in your weight? Did you lose or gain weight?
What have you eaten in the last twenty-four hours?
Have you had any nausea or vomiting?
Current Medications: Multivitamins 1 tablet daily; and Blisovi Fe 1/20 1 tab daily
Allergies: Penicillin (Hives)
PMHx: No pertinent medical history reported, it is unremarkable. No recent hospitalizations
reported in the past. Immunizations are current. Last tetanus shot was taken June 2010. Last flu
shot was taken September 2016. Denies any history of accidents/injury or falls.
Soc Hx: Ms. L was born in Galveston, TX, and currently attends a community college at
Houston Community College – Katy Campus. She attends classes Mon-Fri from 8am to 3pm.
She works at daycare center on the weekends while in school, and during the week on Summer
break. She is Single, and heterosexual. She is in a monogamous relationship with her boyfriend,
and sexually active. She exercises 3x/week, and eats a diet consisting of meat/fish, vegetables,
fruits, rice and beans. She drives a vehicle, and always put on her seatbelt. She is a social drinker,
takes 1-2 glasses of wine every 2 weeks. Never smoked, and denies use of illicit/recreational
drugs. Drinks green tea daily.
Fam Hx:
Maternal Grandmother: deceased at age 83 related to Stroke
Maternal Grandfather: deceased at age 98, no health conditions noted
Paternal Grandmother: deceased at age 38, post-partum hemorrhage
Paternal Grandfather: deceased at age 102 related to uncontrolled HTN
Mother: age 57, No health conditions reportedFather: age 63, has Arthritis, and HTN
Siblings: She has 2 sisters age 18 and 16. Both are alive and well, no health conditions reported
Review of Systems:
GENERAL: The patient is awake, alert, oriented and appears generally well. See HPI.
HEENT: Eyes: No visual loss, blurred vision, double vision or yellow sclera. No decreased
hearing. No hearing loss, sneezing, or congestion. Has complaints of runny nose, sore throat,
headaches, and hoarse voice.
SKIN: No rash or itching.
CARDIOVASCULAR: No chest pain, chest pressure or chest discomfort. No palpitations or
edema.
RESPIRATORY: Respirations are regular and unlabored. No shortness of breath, cough or
sputum.
GASTROINTESTINAL: No anorexia, nausea, vomiting or diarrhea. No abdominal pain or
blood. Complaints of decreased appetite
GENITOURINARY: Denies burning in urination, never been pregnant. Menses are regular, last
menstrual period, 05/28/2017.
NEUROLOGICAL: No dizziness, syncope, paralysis, ataxia, numbness or tingling in the
extremities. No change in bowel or bladder control. Complains of headache that started with the
onset of sore throat.
MUSCULOSKELETAL: No muscle, back pain, joint pain or stiffness.
HEMATOLOGIC: No anemia, bleeding or bruising.
LYMPHATICS: No history of splenectomy. Swollen nodes in the neck
PSYCHIATRIC: No history of depression or anxiety.
ENDOCRINOLOGIC: No reports of sweating, cold or heat intolerance. No polyuria or
polydipsia.
ALLERGIES: Allergic to PCN, gives her hives.
OBJECTIVE.Physical exam: The patient is awake, alert, oriented and appears generally well. The patient is in
no distress. Vital signs revealed a Ht. 5’10”, Wt. 150 lbs; BMI= 21.5; pulse of 96, respirations of
18, temperature of 101.6 and O2 saturation on room air of 98%. HEENT: Pupils are equal, round
and reactive to light. There is no sinus tenderness. Ears are clear. Throat is slightly red with some
swelling and exudate. Neck is supple with anterior cervical lymphadenopathy. Note runny nose
and hoarse voice. Lungs are clear. Heart has regular rate and rhythm without murmur or gallop.
Back showed no CVA tenderness. Abdomen is soft and non-tender. No organomegaly.
Extremities: No edema or tenderness. Skin/Hair/Nails: Normal color for ethnicity and turgor
without rash.
Diagnostic results: CBC and CMP ordered; throat swab was obtained and sent to the lab for
rapid strep testing, rapid influenza diagnostic testing, and follow-up throat culture.
ASSESSMENT.
Differential Diagnoses
1. Influenza: Patient is exhibiting classic signs of sore throat, fever, headache, and nasal
discharge (National Foundation for Infectious Diseases, 2016), with exposure to multiple
infectious sources on her close-quartered college campus, this condition may be likely
pending diagnostics.
2. Group A streptococcal pharyngitis: I would consider this due to her sore throat, but would
need to visualize her mouth and throat to observe for possible erythematous and exudative
tonsils and uvula, as well as other symptoms common to this diagnosis (Vincent et al, 2004).
3. Diphtheria: Common clinical manifestation includes low grade fever, sore throat, headache,
malaise, and hoarseness (Centers for Disease Control and Prevention, 2016), very similar to
my patient’s symptoms. However, this may be unlikely in United States as most people are
vaccinated, though still prevalent in developing countries. In addition, Children under 5 and
adults over 60 years old are particularly at risk for contracting the infection.
4. Epiglottitis: Because of her sore throat and vocal changes, this should be ruled out as it can
advance to emergent airway obstruction, however, my suspicions would tell me that this is
not probable as these patients often present in respiratory distress and it is a potentially lifethreatening illness. This condition is historically a condition more common in children, but itis becoming more frequent in adults. It requires prompt diagnosis and treatment in anyone,
but especially in children, who are more vulnerable to breathing complications (Marcin,
2017).
5. Epstein-Barr virus (EBV) infectious mononucleosis: Typically, these viruses spread most
commonly through bodily fluids, especially saliva. Though classic signs of EBV is prolonged
malaise, sore throat is a very prevalent sign, and the condition more common for those
between ages 15-30 years, and close quarters being a common factor for transmission
(Vincent et al, 2004), however, EBV should also be ruled out due to short time onset, and no
enlarged spleen or liver noted.
PLAN.
This section is not required for the assignments in this course (NURS 6512) but will be required
for future courses.
References
[Show More]





.png)


.png)