CEHRS Study Guide
An insurance adjustor requests a patient's progress notes following a motor vehicle crash. Which
of the following should guide the EHR specialist in releasing this information?
A. meaningful use
B.
...
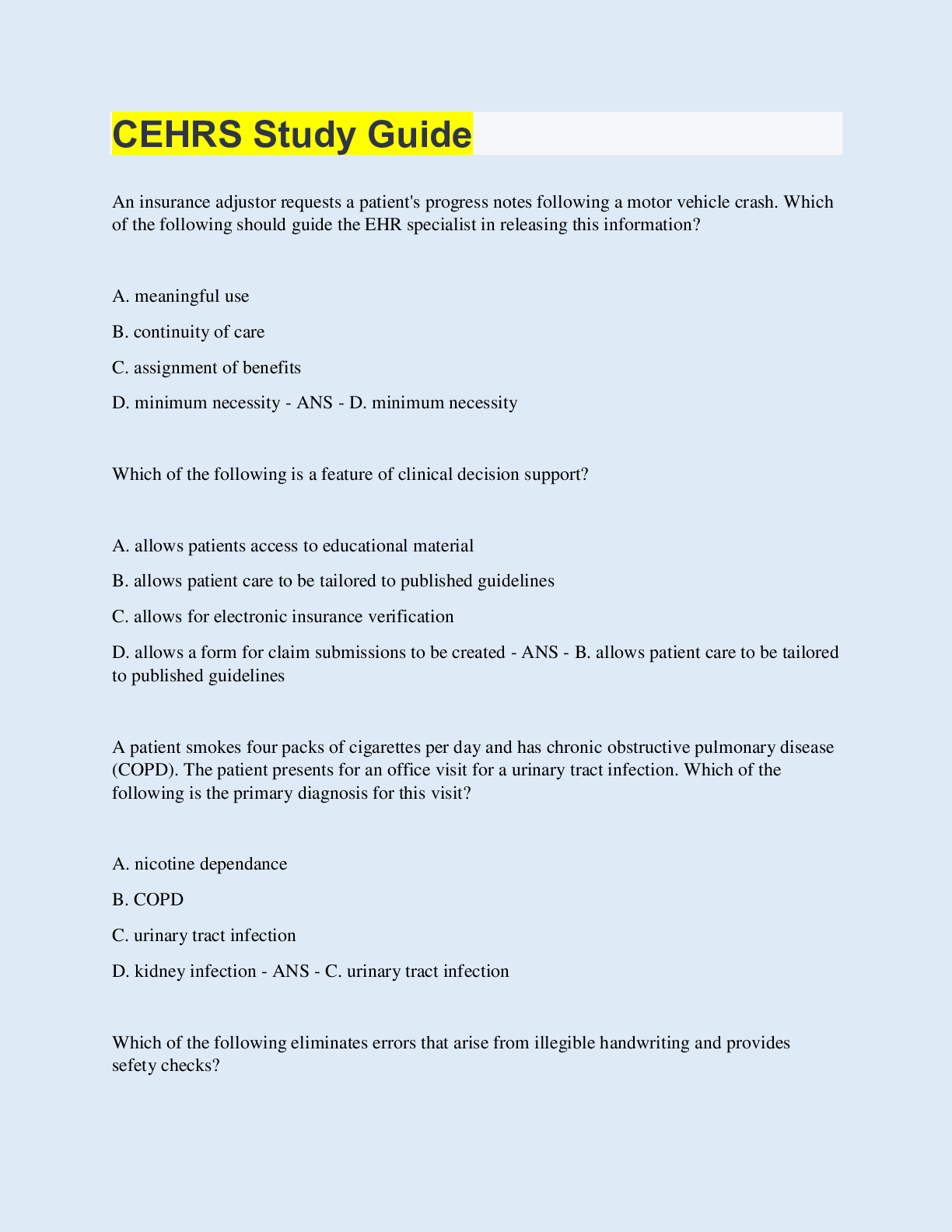
CEHRS Study Guide
An insurance adjustor requests a patient's progress notes following a motor vehicle crash. Which
of the following should guide the EHR specialist in releasing this information?
A. meaningful use
B. continuity of care
C. assignment of benefits
D. minimum necessity - ANS - D. minimum necessity
Which of the following is a feature of clinical decision support?
A. allows patients access to educational material
B. allows patient care to be tailored to published guidelines
C. allows for electronic insurance verification
D. allows a form for claim submissions to be created - ANS - B. allows patient care to be tailored
to published guidelines
A patient smokes four packs of cigarettes per day and has chronic obstructive pulmonary disease
(COPD). The patient presents for an office visit for a urinary tract infection. Which of the
following is the primary diagnosis for this visit?
A. nicotine dependance
B. COPD
C. urinary tract infection
D. kidney infection - ANS - C. urinary tract infection
Which of the following eliminates errors that arise from illegible handwriting and provides
sefety checks?
A. ePrescribing
B. voide recognition software
C. dictation
D. formulary - ANS - A. ePrescribing
A patient presents to a provider's office with strep throat. In which of the the following locations
of the EHR would information about the onset and duration of the symptoms be documented?
A. history of present illness (HPI)
B. chief complaint (CC)
C. review of systems (ROS)
D. past medical history (PMH) - ANS - A. history of present illness (HPI)
A government research study has requested patient data. Which of the following actions should
an EHR specialist take after confirming correct authorization?
A. make back up of data before releasing the information
B. request a release from the patient
C. ask a provider to validate the aggregate data
D. remove PHI from the data - ANS - D. remove PHI from the data
Which of the following circumstances requires a patient to give specific authorization for the
release of PHI?
A. referral to a surgeon
B. mental health treatment
C. provider's participation in research study
D. insurance underwriter's request - ANS - B. mental health treatment
A provider peforms a chest x-ray before and after the placement of a chest tube. This repeat
procedure by the same provider should be coded with which of the following?
A. manifestation rule
B. modifier
C. bundled code
D. global surgery policy - ANS - B. modifier
Which of the following is the most important reason to maintain an inventory of software used in
an office?
A. to verify hardware capability
B. to deter unauthorized duplication
C. to confirm disks and media are kept in a fire-proof box
D. to ensure the versions are correct - ANS - B. to deter unauthorized duplication
A patient presents to a provider's office with a third degree burn on his hand from cooking oil.
Which of the following should an EHR specialist code first?
A. severity
B. cause
C. location
D. classification - ANS - D. classification
The scheduling template within an EHR system can be used for which of the following?
A. automatic canceling of shifts if the pt schedule is sparse
B. identifying a lack of resources that interferes w. workflow
C. reminding providers when annual performance appraisals are due
D. tracking vacation time and sick leave for employees - ANS - B. identifying a lack of resources
that interferes with workflow
Which of the following is the process of converting electronic information into an unreadable
format before it is distributed?
A. access level
B. encryption
C. integration
D. firewall conversion - ANS - B. encryption
Billed procedures and services should be supported by which of the following?
A. medical record
B. compliance plan
C. audit trail
D. encounter form - ANS - A. medical record
An EHR specialist is posting payments for a patient whose insurance plan covers 100% of the
price of an office visit with a $25 co-payment per visit after the patient meets the annual
deductible of $250. To
[Show More]