King Abdulaziz University - IE 411TakeHomeQuiz#2-IE411-Fall2020-Solution. INSTANT DOWNLOAD
$ 14
VATI Maternal Newborn Review.[COMPLETE QUIZ AND ANSWERS FINAL EXAM GRADED A+]
$ 9.5
Dosage-Calculations-A-Ratio-Proportion-Approach-Pediatric-And-Adult-Dosage-Based-On-Body-Weight-
$ 20
OCR 2023 Biology A H420/03: Unified biology A Level Question Paper & Mark Scheme (Merged)
$ 7

Midterm Pharm 2020
$ 10
Straighterline BIO 201L Lab 1 Introduction to Science Quiz 2022 | Complete | 100% Correct Answers
$ 5
CS 1101 Programming Fundamentals Final Exam
$ 7
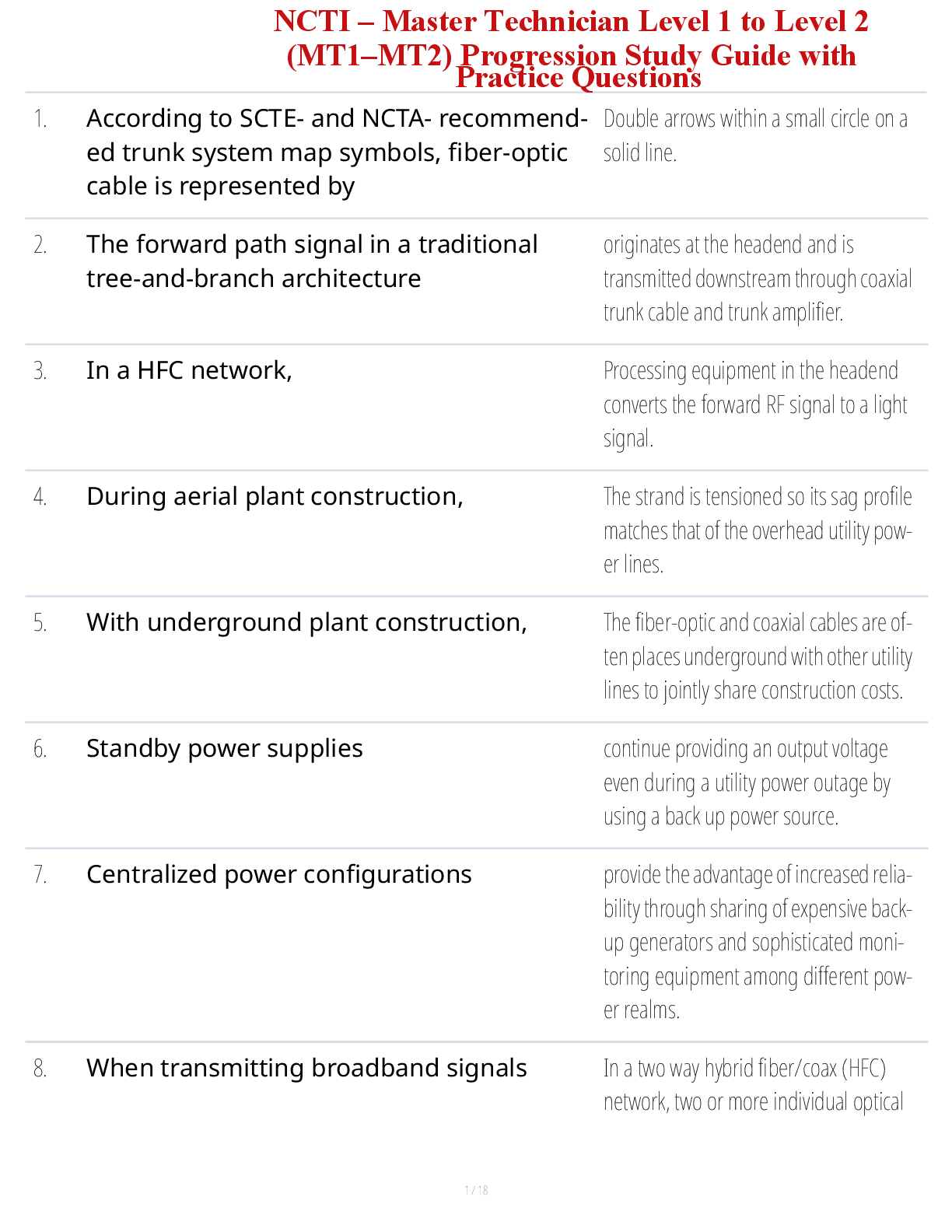
ICT 110 – Final Exam Study Guide with Key Topics and Complete Practice Questions
$ 15
NDG 3325 - Troy University - Adult Health II Lecture Notes: Shock, MODS, and Cardiac Care
$ 10
(answered) STAT 200 STAT200 LAB 7 COMMON DISTRIBUTIONS - PENN STATE
$ 10
eBook [PDF] Towards Wireless Heterogeneity in 6G Networks 1st Edition By Abraham George, G. Ramana Murthy
$ 30
MED SURG NUR 546 EXAM 2
$ 13

IHP 510 Final Project Milestone One Introduction| NYC Health+Hospitals | Bellevue:








.png)