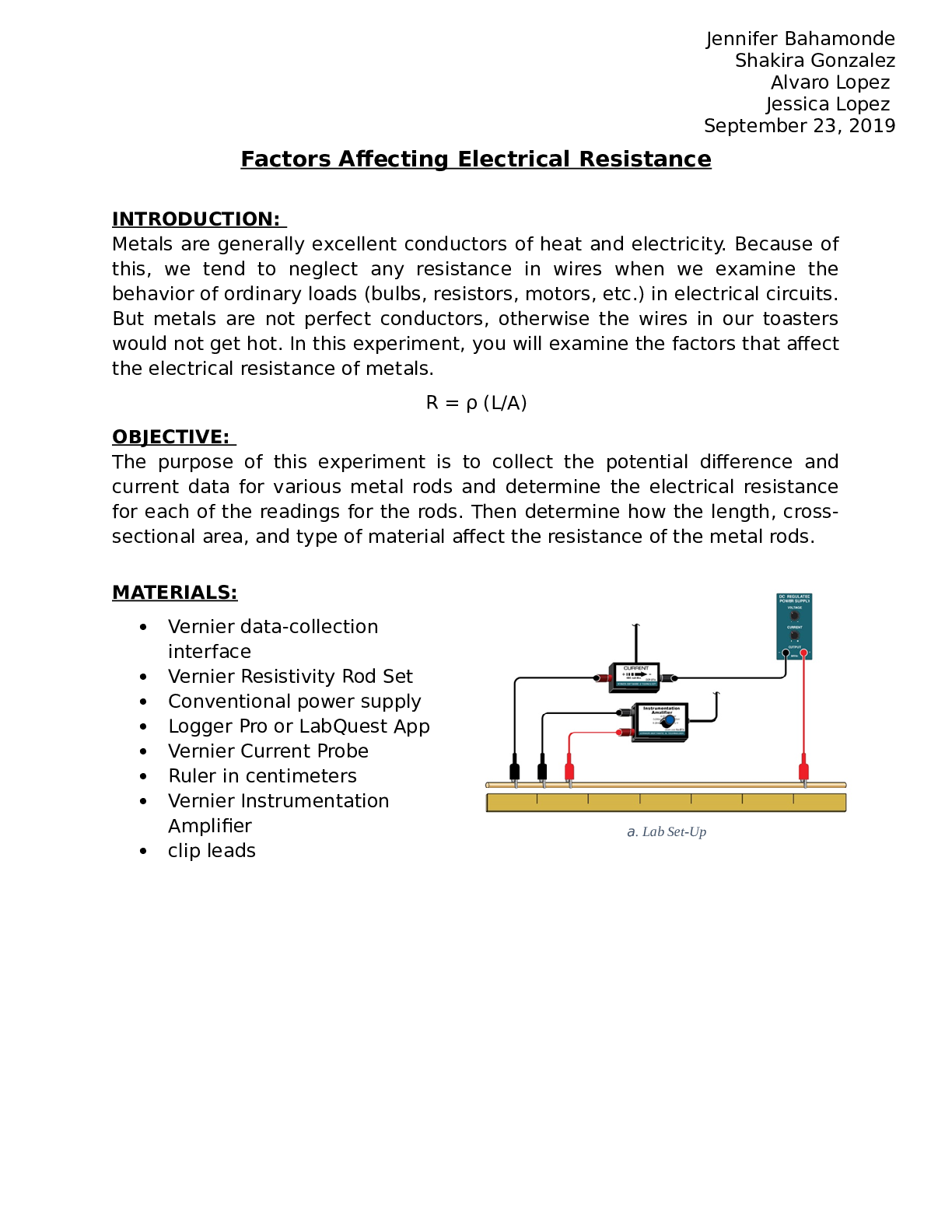
PHY 2053L Physics 2 lab - Miami Dade College, Miami. Factors Affecting Electrical Resistance Experiment Research and Pleriminary Q&A
$ 10.5
NCLEX RN NEWEST 2024,2023 AND 2025 (3 LATEST VERSIONS) TEST BANK ACTUAL EXAM 2500 QUESTIONS AND CORRECT DETAILED ANSWERS WITH RATIONALES 100 % COMPLETE (VERIFIED ANSWERS)/ RN NCLEX TEST BANK|ALREADY GRADED A+|BRAN NEW!!2024
$ 20
SHS 465 Module 6 Quiz | Questions with 100% Correct Answers | Updated & Verified
$ 3
Education Quiz 1 Study Guide / 2025 Update / Score 100% Test Prep
$ 10
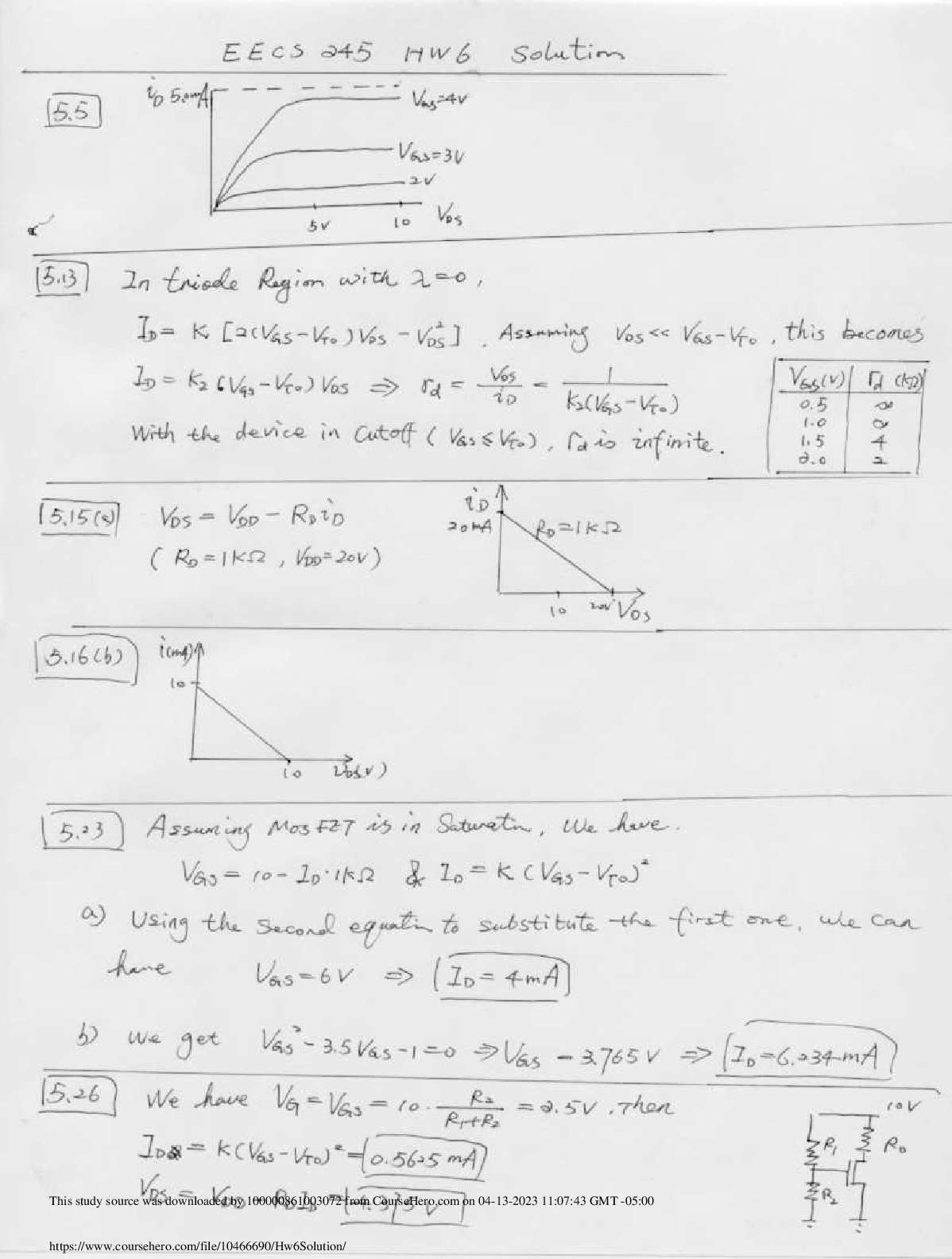
EECS 245 Electronic Circuits Homework 6 Solution:- Case Western Reserve University
$ 7.5
PEDIATRICS FINAL EXAM 2022
$ 15
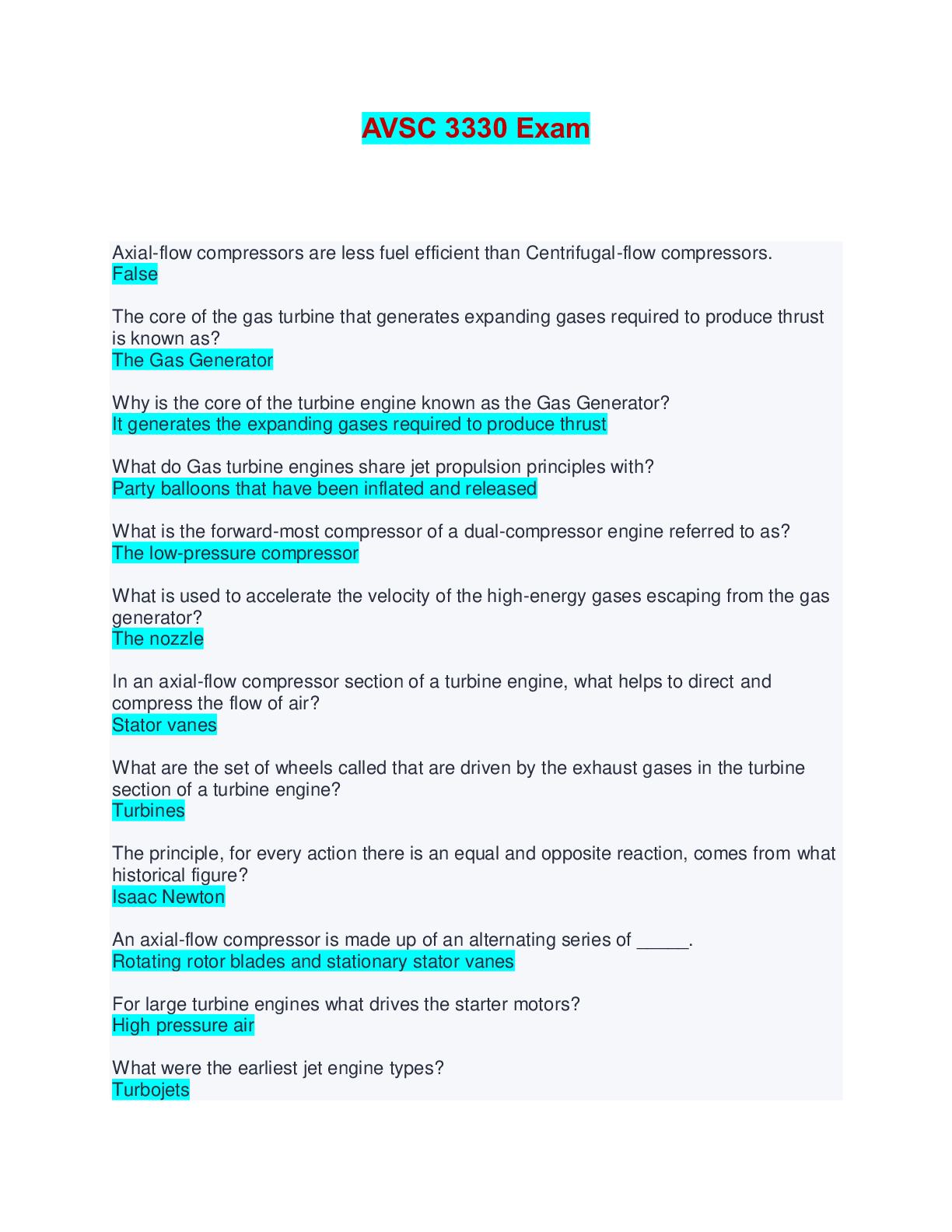
AVSC 3330 Exam | Questions and Answers
$ 13

> AS Level Physics A H156/01 Breadth in physics October 2021
$ 5

GLO-BUS Decisions & Reports years 6/ GLOBUS Decisions & Reports years; Latest 2019/20 Complete Guide, Already Graded A.
$ 8
eBook PDF Legal Research Analysis & Writing 5th Edition By William Putman, Jennifer Albright
$ 27

GCSE (9-1) MATHEMATICS J560/03 Paper 3 (Foundation Tier) PRACTICE PAPER (SET 2) MARK SCHEME
$ 7.5

DeGarmos Materials and Processes in Manufacturing 13th Edition By Black, Ronald ,Kohser (Solution Manual All Chapters)
$ 20

OCR GCE Mathematics A H230/01 Pure Mathematics and Statistics Advanced Subsidiary GCE Mark Scheme for Autumn 2021
$ 7
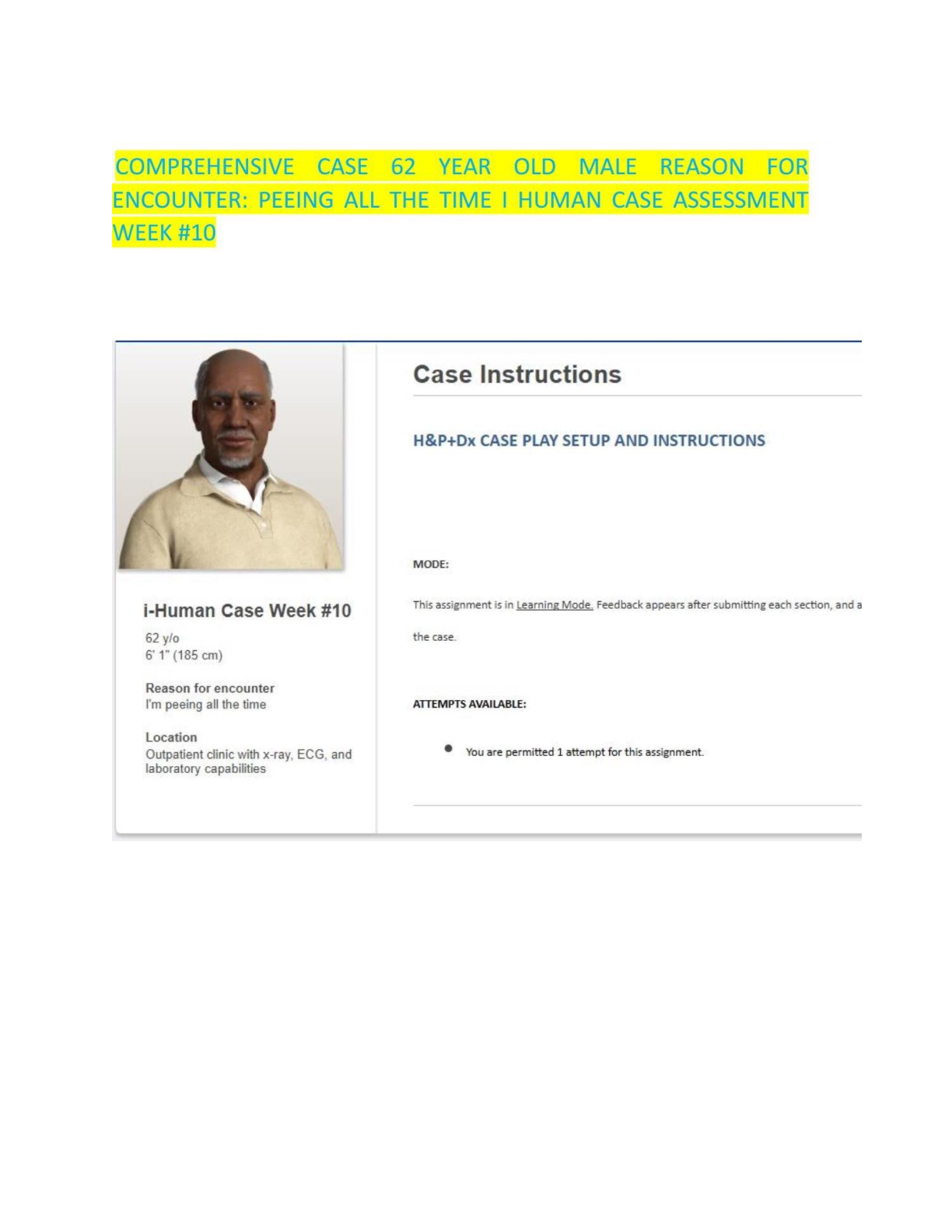
Comprehensive iHuman Case Study 62-Year-Old with I’m Peeing All theTime week #10
$ 11.5
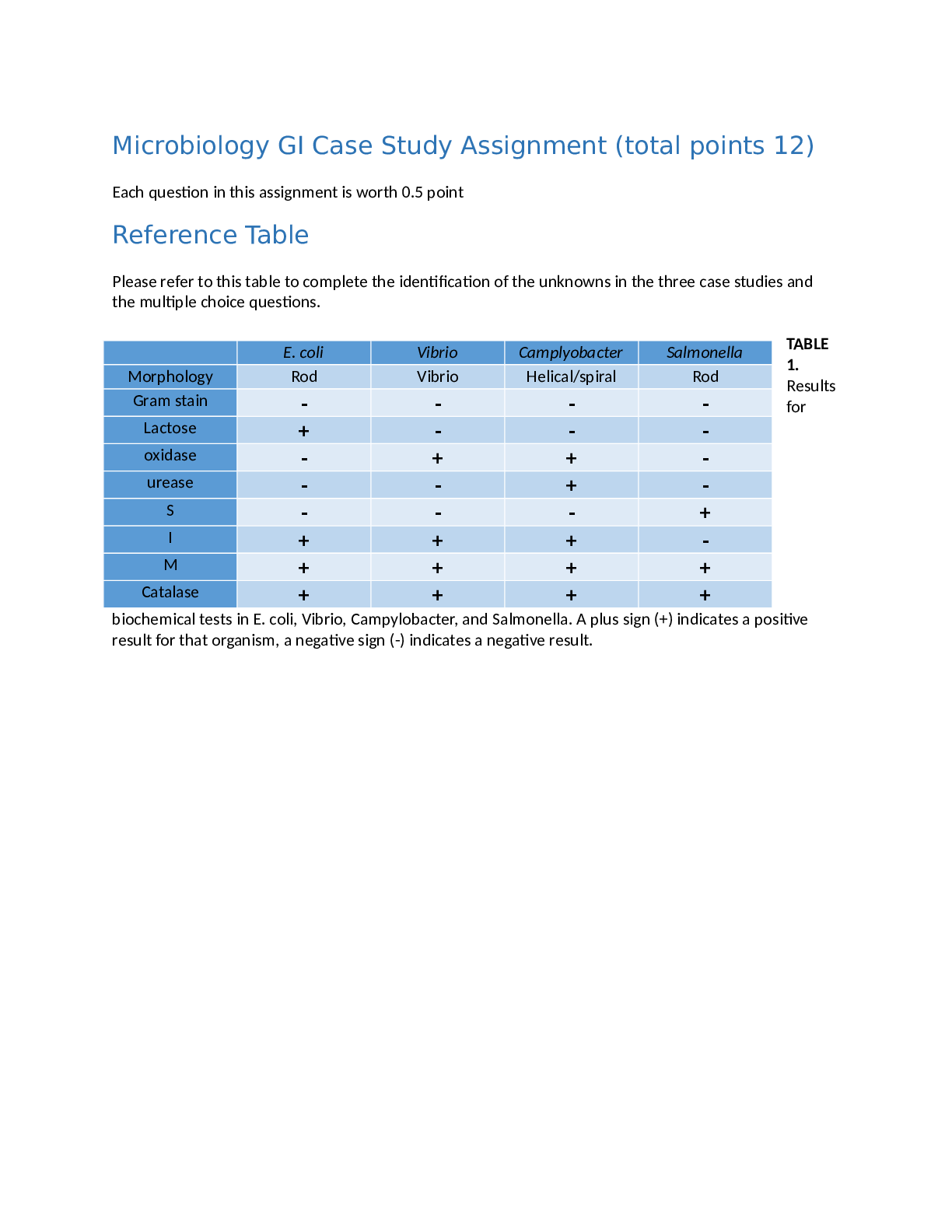
BIOS 242 WEEK 7 ASSIGNMENT: MICROBIOLOGY GI CASE STUDY. 100% correct
$ 15
TEAS 7 EXAM VERSION 1-3 | 3 DIFFERENT VERSION ALL QUESTIONS AND 100% CORRECT ANSWERS ALREADY GRADED A+ | LATEST UPDATE 2026/2027
$ 71
USAREUR Practice Exam, German Driver’s License, German Driver’s License, German Driver’s License, German driver’s license, Driver's License test for Germany (U.S officials only), Germany Driving Test, Germany Driving Course Questions and Answers Graded A+
$ 11
Assignment_File___Review_Questions_1749_( with 100% verified answers)
$ 7

AQA GCSE FRENCH 8658/WF Paper 4 Writing Foundation Mark scheme June 2021 Version: 1.0 Final
$ 8.5
WEEK 9 i-HUMAN CASE STUDY 16 YEARS OLD MALE WITH HAND PAIN 2026 UPDATE SCREENSHOTS
$ 36
 Linda A.png)
PRIORITIZATION, DELEGATION, AND ASSIGNMENT: Practice Exercises for the NCLEX Examination 4TH EDITION (2018, Mosby)
$ 20

OCR GCE Mathematics A H230/01: Pure Mathematics and Statistics AS Level Mark Scheme for June 2025
$ 15

English Language and Literature (EMC) H074/01: Non-fiction written and spoken texts Advanced Subsidiary GCE Question Paper
$ 6.5

ESCO Air Conditioning Exam Prep – Practice Questions with Correct Answers
$ 10
SHRM Learning System Practice Exam with Certified Solutions
$ 15
 (1).png)
OCR Interchange A Level Physics B[ A Level] Physics B H557/02
$ 11.5

IAAI CFI Exam Testbank & Study Guide (2025/2026) – Verified Questions & Detailed Answers | Certified Fire Investigator Prep
$ 23.5
Human Heredity Principles and Issues, 11e Michael Cummings (Test Bank)
$ 25
NASM PERSONAL TRAINING CERTIFICATION 100% CORRECT
$ 13.5
(Complete 90 Q&A) Med Surg 2(II) – Exam 3 Questions with Correct Answers |Graded A+
$ 8
Solution Manual For McGraw-Hill's Taxation of Individuals 2024 Edition, 15th Edition Spilker
$ 15
2025 OCR GCSE Physics A (Gateway Science) J249/01 (Foundation Tier) Complete Question paper with Marking Scheme Combined
$ 8
NHA phlebotomy national exam for 2024
$ 11
STS PRELIMINARY EXAM REVIEW WITH CORRECT ANSWERS
$ 6
NGN Comprehensive predictor test 85 correct answer, VATI Greenlight, VATI LATEST
$ 18
Introduction to Integrative Engineering A Computational Approach to Biomedical Problems 1st Edition By Guigen Zhang (Solution Manual)
$ 17

PROJ 598 Week 5 Assignment; Negotiation Exercise LATEST PROJECT OF 2020/2021 GUARANTEED GRADE A+SCORE
$ 15.5
TEST BANK For Microeconomics, 9th edition by Jeffrey M. Perloff, Chapters 1 - 20