NR 511 Week 1 SOAP - Case Study 1 SOAP NOTE
Case Study 1 SOAP NOTE
Mary, 44 year old female, Caucasian
S: Subjective
Chief Complaint (CC): "My right eye is red and was full of goop this morning."
History of prese
...
NR 511 Week 1 SOAP - Case Study 1 SOAP NOTE
Case Study 1 SOAP NOTE
Mary, 44 year old female, Caucasian
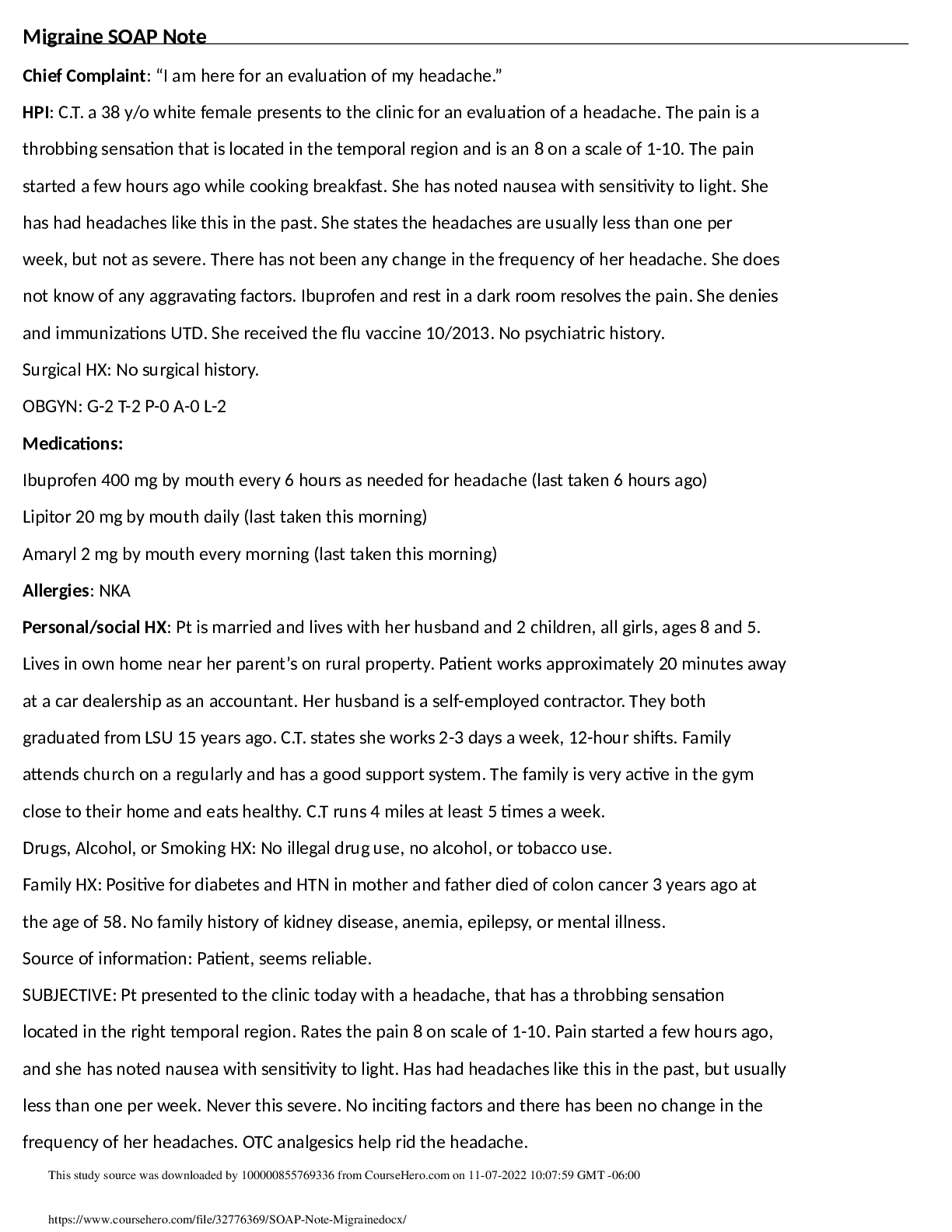
S: Subjective
Chief Complaint (CC): "My right eye is red and was full of goop this morning."
History of present illness (HPI):
O: Mary woke up this morning with her right eye red and with "goop" in it
L: right eye
D: right eye drainage and redness started this morning and continues
C: includes left eye; red and goopy drainage present upon waking this morning
A: states nothing makes it worse
R: states nothing makes it better
T: No treatment
PMI:
Denies past illness or injuries. Hospitalized x 2 for childbirth. No surgeries. No information about
immunizations. Drinks alcohol socially. Denies tobacco, illicit or prescription drug use. Sleeps between 6-
7 hours a night. No drug allergies. Does not take any prescriptions medication. She does take a daily
multivitamin and a B Complex supplement.
SOCIAL
Mary is a high school graduate and works full-time at a local business in the ordering department.
FAMILY
Mary lives at home with her husband, Patrick and her children: 4-year-old twin sons; 7-year-old daughter
and 10-year-old step-son. Mary's parents, Katie and John, also live in the home. They are retired and help
with child care. Mary has two siblings in good health. Patrick is an only child. His parents died of old age
in their 70s. Mary's mother has a history of HTN and HLD. Her father has a history of HTN and HLD and
has used tobacco since age 10. Patrick and John both smoke, but outside, and not in the house. There are
two dogs and a cat in the home as well.
Review of Systems (ROS)
Constitutional: denies fever and chills
[Show More]


.png)

.png)
.png)
.png)