NR 601 Week 4 Mid-term Review
Week 1: aging (chapter 1 – Kennedy)
The major impact of all of these physiological changes can be highlighted with three primary points. First, there is a reduced physiological reserve of
...
NR 601 Week 4 Mid-term Review
Week 1: aging (chapter 1 – Kennedy)
The major impact of all of these physiological changes can be highlighted with three primary points. First, there is a reduced physiological reserve of most body systems, particularly cardiac, respiratory, and renal. Second, there are reduced homeostatic mechanisms that fail to adjust regulatory systems such as temperature control and fluid and electrolyte balance. Third, there is impaired immunological function: infection risk is greater, and autoimmune diseases are more prevalent
Exercise (Kennedy, ch 3)
The preferred amount of exercise is 30 minutes per day for 5 days a week of moderate exercise; if weight management is part of this, 60 minutes per day is advised. This can be broken up into as little as 10-minute intervals throughout the day; any increase in physical activity is desirable and has some value over sedentary behavior
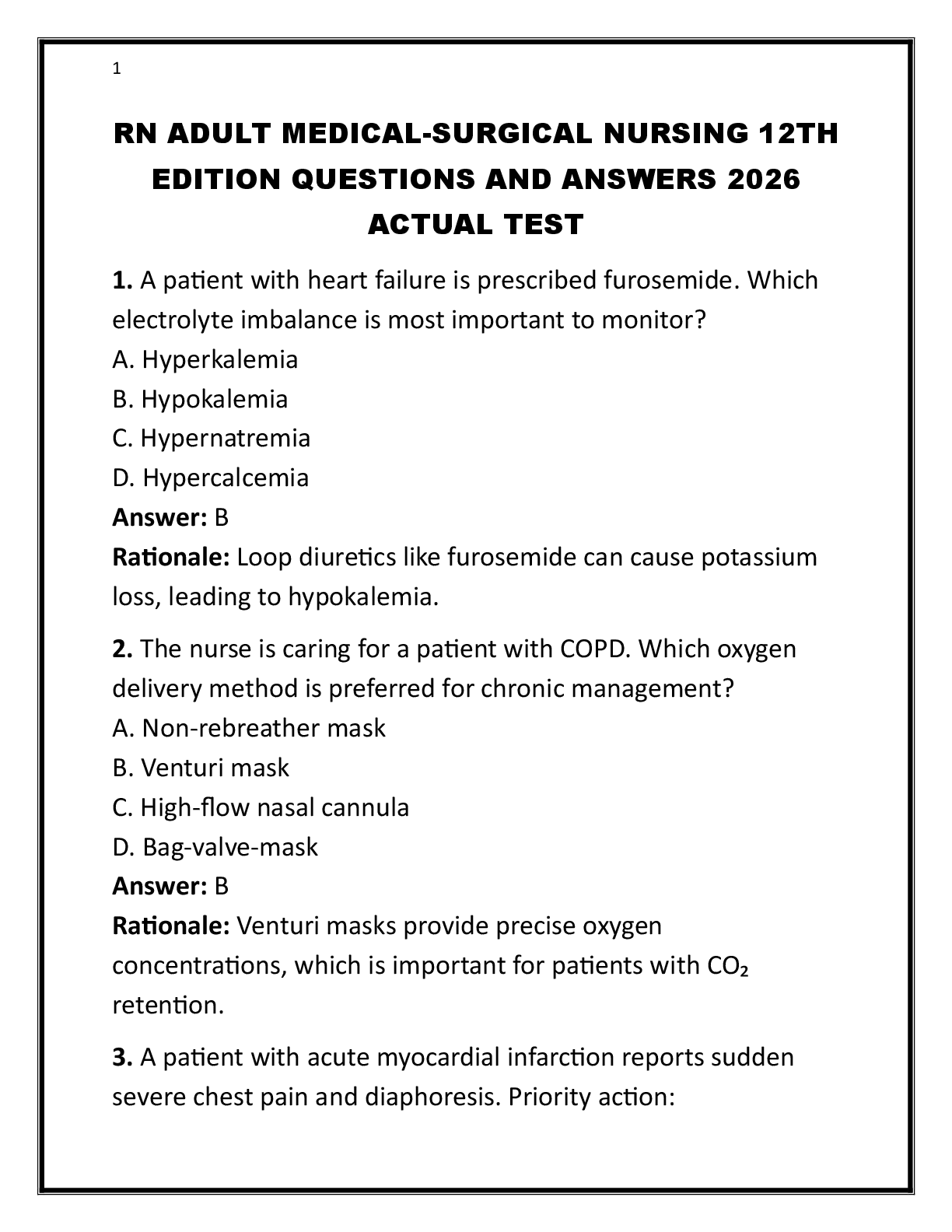
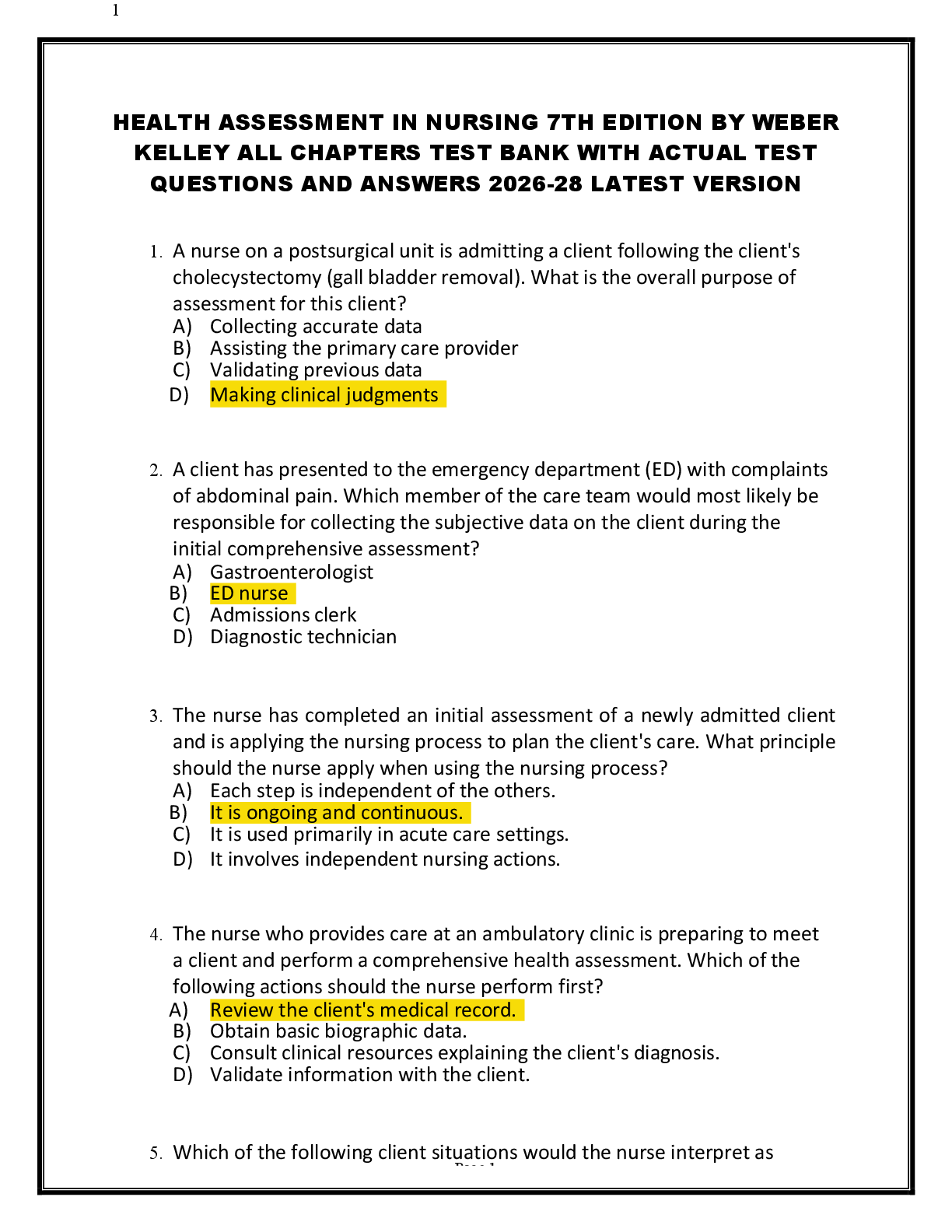
PFTs/Gold criteria
PFT is a group of test that provide quantifiable measurement of lung function and used to diagnose respiratory abnormalities or assess the progression or resolution of lung disease.
FEV1 (1st second Forced Expiratory Volume) and FVC (Forced Vital Capactiy)80% -120%
Patient criteria: FEV1/FVC <0.70 (ratio is the percentage of maximum inspiration expired in 1 second)
FEV1 ≥80% predicted GOLD 1: Mild
50% ≤FEV1 <80% predicted GOLD 2: Moderate
30% ≤FEV1 <50% predicted GOLD 3: Severe
FEV1 <30% predicted GOLD 4: Very Severe
Chest disorders = 8 and gorroll
COPD
Signal symptoms: Dyspnea, chronic cough with sputum production, decreased activity tolerance, wheezing.
Description: COPD (also called chronic obstructive lung disease [COLD]) encompasses a group of conditions distinguished by ongoing expiratory airflow limitation
• leading cause of death, it is a common, preventable, treatable disease that is characterized by persistent airflow limitation that is usually progressive and associated with an enhanced chronic inflammatory response in the airways and the lung to noxious particles
or gases. You will have airway fibrosis, luminal plugs, airway inflammation, increased airway resistance, small airway disease. There is a decreased elastic recoil of the alveoli. • Risk factors for COPD- smoking and increases with the number of pack years smoked.
Second hand smoke as well. Environmental pollution-endotoxins, coal dust, and mineral dust. Nonmodifiable risk factors are gender.
• Dyspnea get progressively worse and is an increased effort to breathe. The issue is getting air out, not in.
• Physical exam- The physical exam be normal in early disease states. So as severity of the airway obstruction increases, the physical exam they rebuild hyperinflation of the lung, decreased breath sounds, wheezes at the lung bases, and then you begin to hear distant heart tones because of the hyperinflation, So S1 and S2 sounds kind of way off in the distance. You will also see use of accessory muscles, pursed-lip breathing increased expiratory phase, neck vein distension.
• Diagnosing- Spirometry is the gold standard for diagnosing COPD- pre and postbronchodilator. Irreversible airflow limitation is a hallmark of COPD.
• Treatment: bronchodilators- beta e agaonists. And you've got a long acting and short acting, and then your anticholingeric, which are long acting and short acting, and then a combination of those. And so the beta agonists, the mechanisms of action of these is that it stimulates the beta-2-adrenergic receptors, increasing cyclic AMP with the resulting relaxing airways with muscles, so they can breathe better. anticholinergics, these block the effect of acetylcholine on the muscarinic-type 3 receptors, which results in bronchodilation. long-acting bronchodilators for moderate air flow limitation, you schedule long-acting bronchodilators because they relieve the symptoms, increases exercise tolerance, reduces the number of exacerbations, and improves your quality of life.
• NON-pulmonary diagnosis are CHF, hyperventilation syndrome, panic attacks, vocal cord dysfunction, obstructive sleep anea, aspergillosis and chronic fatigue syndrome.
CORONARY HEART DISEASE
Primary prevention- Framingham Risk Score Control HTN, hypercholesterolemia, smoking and obesity. Family history
HYPERTENSION
High levels of homocysteine are thought to be injurious to arterial walls, and initial epidemiologic study suggested a strong independent relationship, perhaps accounting for risk in persons with otherwise unexplained coronary events.
ASTHMA
Signal symptoms: Wheezing, shortness of breath, cough (especially at night), chest tightness. Seen every one to 6 months for evaluation.
CHRONIC BRONHCITIS
is a daily chronic cough with increased sputum production lasting for at least 3
consecutive months in at least 2 consecutive years, usually worse on awakening; this may or may not be associated with COPD
EMPHYSEMA
Emphysema is characterized by obstruction to airflow caused by abnormal airspace enlargement distal to terminal bronchioles. Recent evidence indicates that fibrosis occurs and the walls of the airspaces are destroyed, because inflammatory mediators, including polynuclear and mononuclear phagocytes, select T cells, and B cells, infiltrate the airways, resulting in chronic inflammation and remodeling. Air becomes trapped, hindering effective O2 and CO2 exchange.
ISCHEMIC HEART DISEASE
Signal symptoms: Chest pain, tightness, or discomfort.
Description: Ischemic heart disease (IHD) is an imbalance between the supply and demand for blood flow to the myocardium.
ARRHYTHMIAS
may cause symptoms due to a reduced blood flow or inadequate cardiac pump function. In the history, the patient may describe sensations that accompany abnormal cardiac rhythm such as pounding, racing, or skipped beats
LUNG CANCER
Signal symptoms: Cough, dyspnea, weight loss, anorexia, hemoptysis.
Description: Lung cancer is a malignant neoplasm originating in the parenchyma of the lung or airways
MYOCARDIAL INFARCTION
Signal symptoms: Typical symptom is prolonged chest pain (more than 20 minutes' duration); atypical symptoms include shortness of breath, neurological symptoms (confusion, weakness), and worsening of heart failure.
Description: Myocardial infarction (MI) is necrosis of heart tissue caused by lack of blood and oxygen supply to the heart. MIs can be classified as acute ST elevation
[Show More]
.png)

.png)