NUR 2032
RESPIRATORY PROJECT
Aspiration
Name and Definition: “Aspiration is inhalation of foreign material (e.g., oropharyngeal or
stomach contents) into the lungs (Hinkle, 2018).
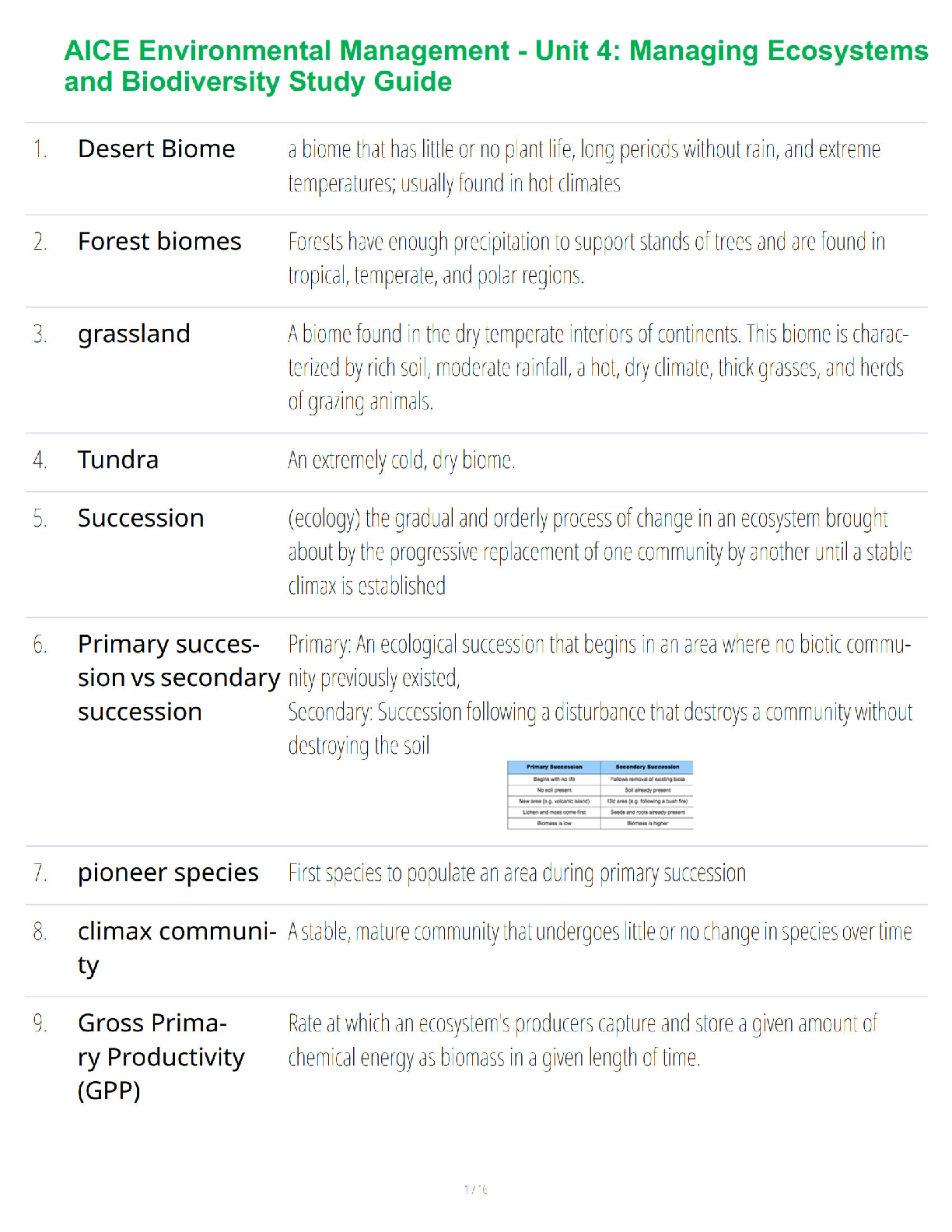
Pathophysiology: “The pathologic pr
...
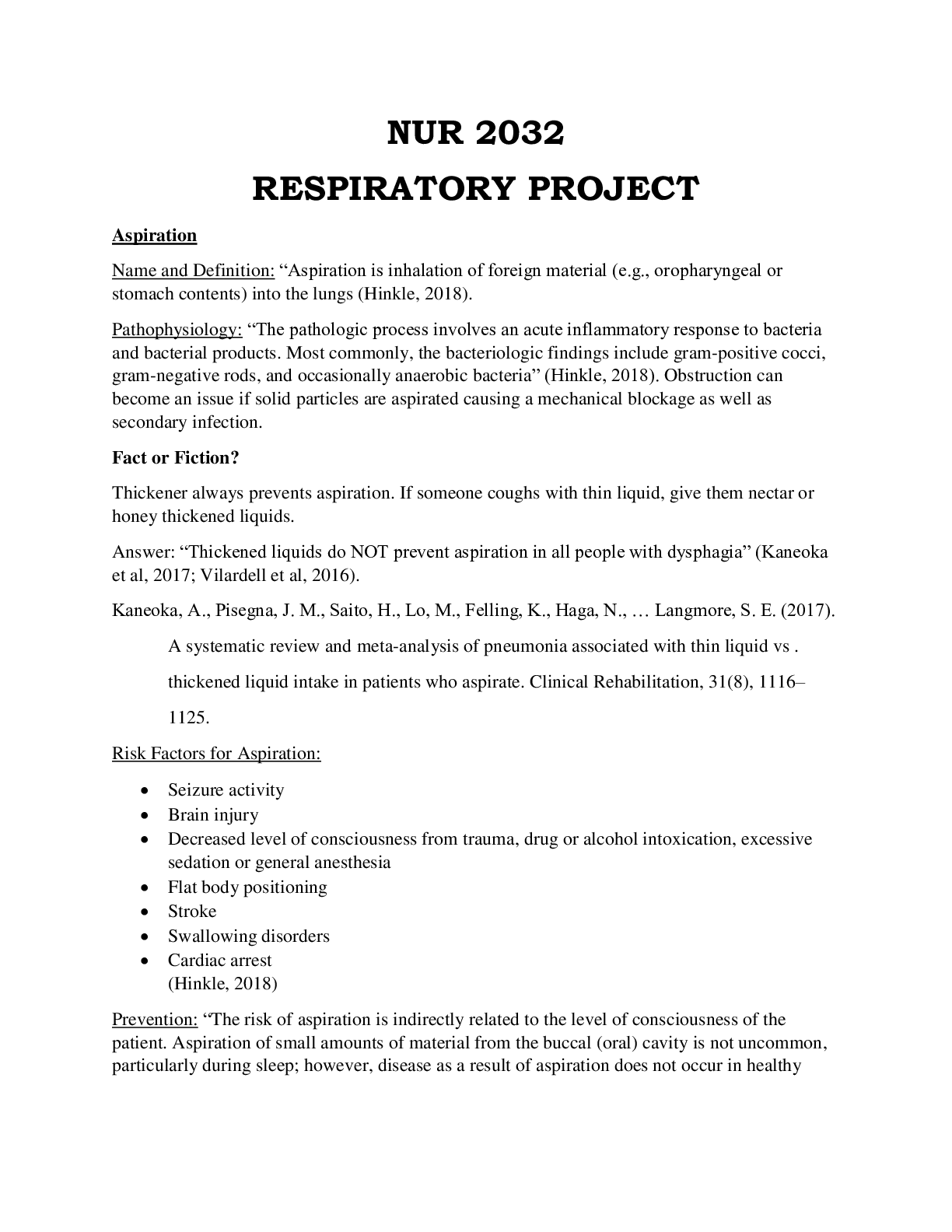
NUR 2032
RESPIRATORY PROJECT
Aspiration
Name and Definition: “Aspiration is inhalation of foreign material (e.g., oropharyngeal or
stomach contents) into the lungs (Hinkle, 2018).
Pathophysiology: “The pathologic process involves an acute inflammatory response to bacteria
and bacterial products. Most commonly, the bacteriologic findings include gram-positive cocci,
gram-negative rods, and occasionally anaerobic bacteria” (Hinkle, 2018). Obstruction can
become an issue if solid particles are aspirated causing a mechanical blockage as well as
secondary infection.
Fact or Fiction?
Thickener always prevents aspiration. If someone coughs with thin liquid, give them nectar or
honey thickened liquids.
Answer: “Thickened liquids do NOT prevent aspiration in all people with dysphagia” (Kaneoka
et al, 2017; Vilardell et al, 2016).
Kaneoka, A., Pisegna, J. M., Saito, H., Lo, M., Felling, K., Haga, N., … Langmore, S. E. (2017).
A systematic review and meta-analysis of pneumonia associated with thin liquid vs .
thickened liquid intake in patients who aspirate. Clinical Rehabilitation, 31(8), 1116–
1125.
Risk Factors for Aspiration:
Seizure activity
Brain injury
Decreased level of consciousness from trauma, drug or alcohol intoxication, excessive
sedation or general anesthesia
Flat body positioning
Stroke
Swallowing disorders
Cardiac arrest
(Hinkle, 2018)
Prevention: “The risk of aspiration is indirectly related to the level of consciousness of the
patient. Aspiration of small amounts of material from the buccal (oral) cavity is not uncommon,
particularly during sleep; however, disease as a result of aspiration does not occur in healthypersons because the material is cleared by the mucociliary tree and the macrophages” (Hinkle,
2018).
Nursing/ medical management:
Maintain head-of-bed elevation at an angle of 30-45 degrees, unless contraindicated
Use sedatives as sparingly as possible
Before initiating enteral tube feeding, confirm the tip location/ assess placement of the
feeding tube at 4-hour intervals, assess for gastrointestinal residuals (< 150mL before
next feeding) to the feedings at 4 hours residuals, avoid bolus feedings in those at high
risk for aspiration.
(Hinkle, 2018)
Pulmonary Tuberculosis
Name and definition: “Tuberculosis (TB) is an infectious disease that primarily affects the lung
parenchyma. It may also be transmitted to other parts of the body, including the meninges,
kidneys, bones and lymph nodes” (Hinkle, 2018).
Pathophysiology: TB begins when a susceptible person inhales mycobacterium and becomes
infected. The bacteria are transmitted through the airways to the alveoli, where they are
deposited and begin to multiply. The bacilli also are transported via the lymph system and
bloodstream to other parts of the body and lungs. The body responds by initiating an
inflammatory response and neutrophils, macrophages and TB specific lymphocytes engulf and
destroy the bacilli and normal tissue is collateral damage. This tissue damage is what results in
the accumulation of exudate in the alveoli, and subsequently causing bronchopneumonia.
Clinical Manifestations:
Low grade fever
Cough (may be productive, nonproductive or hemoptysis may occur)
Night sweats
Fatigue
Weight loss
Gerontologic Consideration: Older adults usually present with less pronounced
symptoms.
Assessment and Diagnostic Findings: Once a patient presents with a positive skin test, blood
test, or sputum culture for acid- fast bacilli, additional assessments MUST be done such as a
complete history, physical exam, tuberculin skin test, chest X-Ray and drug susceptibility
testing. When assessing the lungs for consolidation by evaluating breath sounds, diminished,
bronchial sounds and/or crackles may be found.
QuantiFERON-TB Gold ® In-Tube and T-SPOT® are blood tests available in the U.S; the
In-Tube and T-SPOT® are the preferred diagnostic tests for patient who have received the
vaccination for TB outside the United States and those who not likely to return for the skin test
reading. The results are available within 24-36 hours. A positive test indicates that the patient hasbeen infected with TB bacteria and additional tests are needed. A negative indicates that the
patient’s blood did not react to the test and a latent or active TB infection is unlikely.
Gerontologic Considerations: TB may have atypical manifestations in older adults such as
unusual behavior and altered mental status, fever, anorexia, and weight loss. In many older
adult patients, the TB sin test may not produce a reaction or a delayed reaction up to a
week later (recall phenomenon), so a second skin test should be performed 1-2 weeks
subsequent to the first. Older adults who reside in LTC facilities are at an increased risk
for primary TB compared to the community.
Medical Management: The continuing and increasing resistance of the TB causing bacteria to
medications is an ongoing concern. Usually, pulmonary TB is most often treated with TB antiTB agents for 6-12 months but sometimes a prolonged treatment is necessary to ensure
eradication of the organisms and to prevent relapse. There are 4 first line antituberculosis
medications for active disease; INH, rifampin (Rifadin), pyrazinamide (PZA) and ethambutol
(Myanbutol). Combination medications and medications given only twice a week are also
available to increase patient adherence. INH in particular may be used for prophylaxis for those
who are at risk for the disease such as household family members of a patient with active TB,
patients with HIV infection or other disease process that may weaken the immune system or
patients who are at high risk related to presence of comorbid conditions and a TB skin test
reaction of 10mm or more.
Nursing Management: The most important things for the nurse to remember when treating a
patient with TB is the promotion of airway clearance, advocating adherence to the treatment
regimen, promoting activity and nutrition and preventing transmission.
Airway Promotion is important due to the copious secretions that may obstruct the airway
and interfere with adequate gas exchange. “Increasing the fluid intake promotes systemic
hydration and serves as an effective expectorant” (Hinkle, 2018). The nurse may also educate
and instruct the patient on positions to help facilitate airway drainage.
Treatment Adherence is important because this is the best way to control the spread of
infection. “The major reason treatment fails is that patients do not take regularly and for the
prescribed duration” (Hinkle, 2018). Therefore, patient education is a vital component in the
treatment of TB. “For patients at risk of nonadherence, programs in the community setting may
include comprehensive case management and directly observed therapy” (Hinkle, 2018).Acute Tracheobronchitis
Name and Definition: Acute Tracheobronchitis is an acute inflammation of mucous membranes
of trachea and bronchial tree, often follows Upper Respiratory Infection
Pathophysiology: Inflamed mucosa of bronchi produce mucopurulent sputum in response to
infection, viral or fungal. Sputum culture is essential to identify organism. In addition, physical
and chemical irritants, gases, and other contaminants can also cause irritation leading to
inflammation.
Clinical Manifestations: Dry irritating cough, scant amount of mucoid sputum, may have fever or
chills, night sweats, headache, malaise. As infection progresses, patient may experience
shortness of breath, noisy ventilation (stridor or wheeze), purulent sputum. In severe cases,
patient may produce blood streaked secretions.
Assessment and Diagnostic: Chest X-Ray, sputum culture
Medical Management: Antibiotics may be indicated dependent on symptoms and culture results.
Patient should increase fluid intake to thin secretions. Suctioning and bronchoscopy may be
needed depending on severity. Rarely, intubation may be needed if patient goes into respiratory
failure or with other coexisting diagnosis that impair the respiratory system.
Nursing Management: Acute Tracheobronchitis is usually treated at home. The nurse should
encourage bronchial hygiene such as increased fluids to thin mucous and directed coughing to
expel mucous. Nurse should assist patient to sit up and cough effectively. Nurse should
emphasize the importance of completing all antibiotics and rest.
Pneumonia
Name and Definition: Pneumonia is an inflammation of the lung parenchyma caused by various
microorganisms.
Pathophysiology: Normally the upper airway prevents potentially infectious particles from
reaching the lower respiratory tract. Pneumonia arises from normal flora present in patients
whose resistance has been altered or with aspiration of flora present in the oropharynx. Patients
often have an acute or chronic underlying disease that impairs defenses. Pneumonia may also
result from bloodborne organisms that enter pulmonary circulation and are trapped in the
pulmonary capillary bed.
Clinical Manifestations: Pneumonia signs vary depending on type, organism and any underlying
diseases. It is not possible to diagnose specific form based solely from clinical manifestations
alone.- Streptococcal Pneumonia- Usually has sudden onset of chills, rapidly rising fever,
chest pain aggravated by dee breathing and coughing, tachypnea, respiratory distress.
Relative bradycardia may indicate viral infection.
- Some patients exhibit symptoms of Upper Respiratory Infection, headache, low grade
fever, myalgia, rash, pharyngitis. Severe cases may present with cyanosis.
- Some patients may exhibit orthopnea, poor appetite, fatigue.
- Signs and symptoms may differ with underlying conditions.
Assessment and Diagnosis: Diagnosis is made by obtaining a patient history, physical
examination, chest X-Ray, blood culture, sputum culture
Complications: Pneumonia is one of the most common causes of death from infectious diseases
in the US. Other complications include Hypotension, septic shock, respiratory failure, pleural
effusion, delirium.
Medical Management: Antibiotics may be indicated depending on results from culture and
sensitivity. Antibiotics are ineffective against viral cases and may lead to adverse reactions. Viral
cases are best treated symptomatically (antipyretics, antitussive)
Nursing Management: Removing secretions, increasing hydration, humidification, coughing,
deep breathing exercises, chest physiotherapy, oxygen therapy, promoting rest
[Show More]